Gait in prosthetic rehabilitation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 72: | Line 72: | ||
== <br> Pathological Gait == | == <br> Pathological Gait == | ||
Pathological gait is an altered gait pattern due to deformities, weakness or other impairments, for example, loss of motor control or pain<ref name="Fish" />. | Pathological gait is an altered gait pattern due to deformities, weakness or other impairments, for example, loss of motor control or pain<ref name="Fish" />. Alterations can broadly be divided into neurological or musculoskeletal causes<ref name="Malanga">Malanga G &amp;amp;amp;amp;amp;amp;amp;amp;amp; Delisa J.A. Section One: Clinical Observation. Office of rehabilitation Research and Development No Date. http://www.rehab.research.va.gov/mono/gait/malanga.pdf (accessed 6 February 2010)</ref>. | ||
=== Musculoskeletal Causes === | === Musculoskeletal Causes === | ||
| Line 163: | Line 163: | ||
|} | |} | ||
<br> | <br> | ||
== Prosthetic Gait == | == Prosthetic Gait == | ||
Revision as of 11:55, 20 April 2015
Original Editor - Abby Cain as part of the WCPT Network for Amputee Rehabilitation Project
Top Contributors - Admin, Rachael Lowe, Kim Jackson, Tarina van der Stockt, Naomi O'Reilly, Jess Bell and Simisola Ajeyalemi
Normal Gait [edit | edit source]
Gait is a term used to describe a walking pattern. ‘Normal gait’ is used to define a pattern which has been generalised from the general public across many variables, including age and sex[1].
A complete cycle of gait begins at initial contact of one limb and ends at the repeated initial contact of the same limb, performing all phases of gait in doing so. This full cycle can be described as a stride. A step is sometimes incorrectly used to describe this cycle. A step however, is different; it is described as the distance of heel strike from one leg to the heel strike of the opposite leg[2].
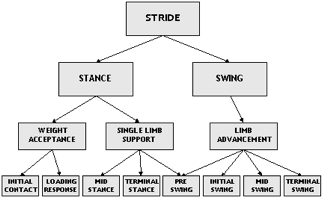
The gait cycle can be split into 2 stages;
- Stance Phase -Time the foot is in contact with the floor, weight acceptance and single leg stance, which makes up 60% of the cycle[1]
- Swing Phase – The period of time where the limb is lifted from the floor, limb advancement. This makes up 40% of the cycle[1]
In order to describe the elements of gait, the cycle can be broken down further into 8 sub factors[1][2]:
- Initial contact
- Loading response
- Midstance
- Terminal stance
- Preswing
- Initial swing
- Midswing
- Terminal swing
The diagram demonstrates this division of gait cycle.
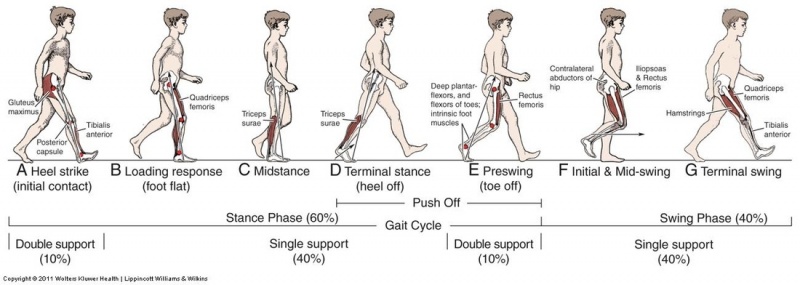
Initial contact[edit | edit source]
Also known as heel strike. This is the first moment the foot comes into contact with the floor. The hip is flexed approximately to 30 degrees , knee extended between 0-5 degrees and ankle dorsiflexed to a neutral position, giving contact with the floor at approximately a 25 degree angle. This is the first phase of double limb support. The aim of initial contact is to stabilise the limb in preparation for it to take the impending forward translation of body weight[2][3].
Loading response[edit | edit source]
The foot flattens on the floor through pronation. The hip begins to extend and propels the body forwards and over the foot, using the heel as a ‘rocker’. The knee then flexes to allow shock absorption. The aim of this phase is shock absorption, weight bearing stability and preservation of progression[2][3].
Mid stance[edit | edit source]
This is the first half of single limb support. Weight is aligned fully over the supporting foot through ankle dorsiflexion, while the hip and knee extend, as the other foot lifts of the floor. The body weight is fully supported on one leg[2][3].
Terminal stance[edit | edit source]
This is the second half of single leg support; it begins as the other leg lifts of the floor. The heel of the loaded limb lifts off the floor and the body weight moves forward past the forefoot, as the hip increases in extension. The knee gains full extension and begins to flex again. This phase is completed when the non-loaded limb makes contact with the floor[2][3].
Pre-swing[edit | edit source]
Also known as ‘toe off’ and is the final phase of stance. The other limb has now begun a new stance phase and is in the initial contact phase. The limb is rapidly off loaded with a forward push to transfer the weight onto the opposite limb. The knee is flexed and the ankle plantarflexes as the toe leaves the ground[2][3].
Initial swing[edit | edit source]
The foot is lifted off the floor by hip and knee flexion, as the ankle begins to dorsiflex. The other foot will be in midstance phase. When the off loading limb is level with the leg in stance phase the initial swing phase is complete[2][3].
Mid swing[edit | edit source]
The limb swings forward of the body through hip flexion as the knee begins to extend. The foot is clear of the floor[2]
Terminal swing[edit | edit source]
Also known as late swing, the knee becomes fully extended and the ankle dorsiflexes to neutral as the foot prepares to make contact with the floor[2].
The diagram below demonstrates the 8 phases of the gait cycle:
Pathological Gait [edit | edit source]
Pathological gait is an altered gait pattern due to deformities, weakness or other impairments, for example, loss of motor control or pain[1]. Alterations can broadly be divided into neurological or musculoskeletal causes[4].
Musculoskeletal Causes[edit | edit source]
Pathological gait patterns resulting from musculoskeletal are often caused by soft tissue imbalance, joint alignment or bony abnormalities. Infliction of these on one joint often then impacts on other joints, affecting the gait pattern as a result[4]. The common deviation can be categorised broadly as[4]:
- Hip Pathology
- Knee pathology
- Foot and ankle pathology
- Leg length discrepancy
- Pain
Hip pathology[edit | edit source]
Arthritis is a common cause of pathological gait. An arthritic hip has reduced range of movement during swing phase which causes an exaggeration of movement in the opposite limb ‘hip hiking[4].
Excessive hip flexion can significantly alter gait pattern most commonly due to; • Hip flexion contractures • IT band contractures, • Hip flexor spasticity, • Compensation for excessive knee flexion and ankle DF, • Hip pain • Compensation for excess ankle plantar flexion in mid swing[2]. The deviation of stance phase will occur mainly on the affected side. The result is forward tilt of the trunk and increased demand on the hip extensors or increased lordosis of the spine with anterior pelvic tilt. A person with reduced spinal mobility will adopt a forward flexion position in order to alter their centre of gravity permanently during gait[2].
Hip abductor weakness. The abductor muscles stabilise the pelvis to allow the opposite leg to lift during the swing phase. Weak abductor muscles will cause the hip to drop towards the side of the leg swinging forward. This is also known as Trendelenburg gait[5]
Hip adductor contracture. During swing phase the leg crosses mid line due to the weak adductor muscles, this is known as ‘scissor gait’[5]
Weak hip extensors will cause a person to take a smaller step to lessen the hip flexion required for initial contact, resulting in a lesser force of contraction required from the extensors. Overall gait will be slower to allow time for limb stabilisation. Compensation is increased posterior trunk positioning to maintain alignment of the pelvis in relation to the trunk[2][5]
Hip flexor weakness results in a smaller step length due to the weakness of the muscle to create the forward motion. Gait will likely be slower and may result in decreased floor clearance of the toes and create a drag[2]
Knee pathologies[edit | edit source]
Weak quadriceps. The quadriceps role is to eccentrically control the knee during flexion through the stance phase. If these muscles are weak the hip extensors will compensate by bringing the limb back into a more extended position, reducing the amount of flexion at the knee during stance phase. Alternatively heel strike will occur earlier increasing the ankle of plantar flexion at the ankle, preventing the forward movement of the tibia, to help stabilise the knee joint[2][5].
Severe quadriceps weakness or instability at the knee joint will present in hyperextension during the initial contact to stance phase. The knee joint will ‘snap’ back into hyperextension as the body weight moves forwards over the limb[2][5]
Knee flexion contraction will cause a limping type gait pattern. The knee is restricted in extension, meaning heel strike is limited and step length reduced. To compensate the person is likely to ‘toe walk’ during stance phase. Knee flexion contractures of more than 30 degrees will be obvious during normal paced gait. Contractures less then this will be more evident with increased speeds[2][4][5].
Ankle Pathologies[edit | edit source]
Ankle dorsi flexion weakness results in a lack of heel strike and decreased floor clearance. This leads to an increased step height and prolonged swing phase[2][5].
Calf tightening or contractures due to a period of immobilisation or trauma will cause reduced heel strike due to restricted dorsiflexion. The compensated gait result will be ‘toe walking’ on stance phase, reduced step length and excessive knee and hip flexion during swing phase to ensure floor clearance[2][4].
Leg length discrepancy[edit | edit source]
Leg length discrepancy can be a result of an asymmetrical pelvic, tibia or femur length or for other reasons such as a scoliosis or contractures. The gait pattern will present as a pelvic dip to the shortened side during stance phase with possible ‘toe walking’ on that limb. The opposite leg is likely to increase its knee and hip flexion to reduce its length[4].
Antalgic Gait[edit | edit source]
Antalgic gait due to knee pain presents with decreased weight bearing on the affected side. The knee remains in flexion and possible toe weight bearing occurs during stance phase[4]
Antalagic gait due to ankle pain may present with a reduced stride length and decreased weight bearing on the affected limb. If the problem is pain in the forefoot then toe off will be avoided and heel weight bearing used. If the pain is more in the heel, toe weight bearing is more likely. General ankle pain may result in weight bearing on the lateral border[2][4][5].
Antalgic gait due to hip pain results in reduced stance phase on that side. The trunk is propelled quickly forwards with the opposite shoulder lifted in an attempt to even the weight distribution over the limb and reduce weight bearing. Swing phase is also reduced[2][4].
Common neurological causes of pathological gait[edit | edit source]
Hemiplegic gait, often seen as a result of a stroke. The upper limb is in a flexed position, adducted and internally rotated at the shoulder. The lower limb is internally rotated, knee extended and the ankle inverted and plantar flexed. The gait is likely to be slow with circumduction or hip hitching on the affected limb to aid floor clearance[6][4].
Diplegic gait. Spasticity is normally associated with both lower limbs. Contractures of the adductor muscles can create a ‘scissor’ type gait with a narrowed base of support. Spasticity in the lower half of the legs results in plantarflexed ankles presenting in ‘tip toe’ walking and often toe dragging. Excessive hip and knee flexion is required to overcome this[6][4].
Parkinsonian gait often seen in Parkinson’s disease or associated with conditions which cause parkinsonisms. Rigidity of joints results in reduced arm swing for balance. A stooped posture and flexed knees are a common presentation. Bradykinesia causes small steps which are shuffling in presentation. There may be occurrences of freezing or short rapid bursts of steps known as ‘festination’ and turning can be difficult[6][4].
Ataxic gait is seen as uncoordinated steps with a wide base of support and staggering/variable foot placement. This gait is associated with cerebellar disturbances and can be seen in patients with longstanding alcohol dependency[6][4]
People withsensory disturbances may present with a sensory ataxic gait. Presentation is a wide base of support, high steps and slapping of feet on the floor in order to gain some sensory feedback. They may also need to rely on observation of foot placement and will often look at the floor during mobility due to lack of proprioception[6][4].
Myopathic gait. Due to hip muscular dystrophy, if it is bilateral the presentation will be a ‘waddling gait’, unilaterally will present as a Trendelenburg gait[6].
Neuropathic gaits. High stepping gait to gain floor clearance often due to foot drop[6]
Below are links to videos demonstrating normal gait and various gait abnormalities:
Prosthetic Gait [edit | edit source]
After an amputation the amputee uses different muscle groups in order to create a smoother gait pattern. Overall energy consumption required is higher, due to the increased effort required to compensate for the lose of the limb. The amount of metabolic oxygen consumption in a non amputee correlates directly to increased walking distance and speeds. In the amputees, however, this metabolic cost is higher even at normal speed. On average these increased requirements are[7]:
- Traumatic Transtibial gait - 25% increased energy requirement
- Vascular Transtibial gait- 40 % increase
- Traumatic Transfemoral gait-68% increase
- Vascular transfemoral gait -100% increase
Transtibial Gait[edit | edit source]
The average gait pattern will vary dependent on the type of prosthesis used for mobility, however generalisations can be made. The ankle of the prosthesis has a reduced range of movement compared to the anatomical ankle. This results in prolonged heel strike and weight bearing through the heel before flat foot contact, with delayed forefoot loading[8]
Knee flexion is decreased at initial contact and the overall maximum flexion achieved is reduced as the foot moves to floor contact to[8]. During swing phase of the non prosthetic limb the body weight begins to move forward over the prosthetic limb, which is in stance phase. In order to gain adequate step length of the non prosthetic limb, heel rise on the prosthesis occurs earlier. The heel rise achieved is greater than that of a normal gait pattern[8]. This creates an elevation of the body and results in a greater loading force on the non prosthetic side (approx 130% compared to average 111%) as the body weight drops more rapidly onto the limb. Greater quadriceps contraction is needed to absorb the force[7][8]. The ‘toe off’ force generated from the prosthetic limb is reduced, which is compensated for by the hip flexors. Flexion of the knee on the prosthetic limb occurs with some hamstring contraction but mainly eccentric contraction of the quadriceps[9]
During the stance phase the energy generated by the prosthetic limb is reduced by 50% to that which would be generated by the normal limb, this is compensated by greater energy expenditure in muscles higher up the limb. The rocker effect of the prosthesis results in increased instability and the reduced knee flexion achieved on the prosthetic side requires hip muscles to generate greater energy to ensure stability. As the body transfers weight in a forward motion this energy generation is then transmitted to the trunk muscles in order to generate enough force to propel the body forward and to compensate for the loss of energy through the prosthesis[7].
Due to the reduced ankle movement of the prosthesis the range of extension at the hip is reduced to approx half of that of the opposite limb. The stance time on the non prosthetic side is also increased compared to the prosthetic side[8].
Transfemoral gait[edit | edit source]
A person with a transfemoral amputation has to compensate for the loss of both the knee and ankle joint[7]. The gait cycle is affected by the quality of the surgery, the type and alignment of prosthesis, the condition of the stump and the length of the remaining muscular structure and how well these are reattached[9].
The main focus of the gait cycle is to prevent the knee from buckling during stance phase. A ‘fixed knee’ prosthesis will counteract this issue. A ‘free knee’ will need to remain in extension for longer throughout the stance phase approx 30-40% to ensure buckling does not occur[7]. This extension causes prolonged heel strike and the body will move forward over the prosthetic leg as one unit for stance phase. The hip extensors on the prosthetic side will work to stabilise the limb in prosthetic weight bearing[7].
During swing phase of the prosthetic limb the hip extensors and calf muscles on the non prosthetic side help to generate force for the non prosthetic limb to gain swing forwards. Hip flexors on the prosthetic limb must generate the same force required during normal gait. Although the prosthesis is generally 30% lighter than the limb would be, speed generated by the hip flexors is required in order to snap the prosthesis of a ‘free knee’ into extension for heel strike[7][8]. General control and strength is reduced in a transfemoral amputation due to the shortened lever length of the thigh muscles, which reduces the force of contraction[7]. For amputees with a fixed knee prosthesis floor clearance is reduced during swing phase, due to the lack of knee flexion and ankle dorsi flexion. Elevation of the hip using trunk and hip muscles is required to prevent dragging on the floor known as ‘hip hitching’ or ‘hip hiking’[8]. Stance time on the non prosthetic limb is increased as it is for transtibial amputees, because of the instability resulting from the prosthesis and the reduced range of motion available. Overall energy expenditure is higher than is required for a transtibial amputee due to the energy which is lost through the prosthesis over two joints and not one. Greater compensation is required by the hip and trunk muscles and the contra lateral limb to generate the energy required for stability and movement throughout the gait cycle[7].
Gait Deviations [edit | edit source]
While assessing amputee gait it is important to be aware of normal gait and how normal gait in the amputee is affected. Furthermore there may be deviations which an amputee will adopt to compensate for the prosthesis, muscle weakness or tightening, lack of balance and fear. These deviations create an altered gait pattern and it is important that these are recognised, as rehabilitation of the gait will need to encompass corrections of these deviations[9][8].
Common deviations are;
Transtibial[edit | edit source]
External rotation of the prosthesis at heel strike
Causes; heel to hard, too hard a plantar flexion bumper, socket too loose[10].
Knee fully extended at heel strike
Causes; faulty suspension of the prosthesis- too soft heel cushion or plantar flexor bumpers, foot placement too far forward on stepping, lack of pre-flexion of the socket, discomfort/pain, quads weakness[8][11]
Increased Knee flexion at heel strike
Causes; faulty suspension of prosthesis, prosthetic foot too set in too much dorsiflexion, stiff heel cushion, flexion contracture of the knee, foot to posterior in relation to socket[8][10][11]
Rotation of foot at heel strike
Causes; heel too hard, loose socket[11]
Unequal stride length
Causes; faulty suspension limiting knee flexion, poor gait pattern[8]
Knee flexion ‘jerky’ in presentation during heel strike to foot flat
Causes; weak quadriceps[8]
Abrupt knee flexion as foot moves in flat foot contact with the floor;
Causes; excessive dorsiflexion of the prosthetic foot, foot too posterior in relation to socket of the prosthesis, lack of suspension in the prosthesis, lack of cushion due to the shoe, heel of the shoe too high[8].
Knee stays extended from heel strike to flat foot contact
Causes; Step length too long, foot too anterior on the prosthesis, foot too planter flexed on the prosthesis, heel too soft, discomfort when flexing the knee in the prosthesis, not enough heel on the shoe[8][10].
Amputee drops into the socket as the foot moves into flat foot
Causes; lack of prosthetic socks, suspension loose, faulty socket.
Medio or lateral shift during stance phase
Causes; foot placement (medial placement causes lateral thrust and vice versa), foot alignment on the prosthesis, socket loose[8][11]
Heel off occurs too early causing early knee flexion (drop off)
Causes; foot too posterior on the prosthesis in relation to the socket, excessive dorsiflexion of the foot on the prosthesis, soft heel bumper on the prosthesis[8][11]
Delayed heel causing hyperextension of the knee- walking up hill sensation
Causes; foot set too far forward on the prosthesis in relation to socket, too hard a heel cushion, too much plantar flexion on the foot[10]. (9)(10)
The socket drops down off the limb after ‘toe off’
Causes; socket too lose, not enough prosthetic socks[8]
During swing phase foot ‘whips’ laterally or medially
Causes; poor suspension, knee internally or externally rotated[8][11]
Transfemoral gait deviations[edit | edit source]
Rotation of the heel at heel strike
Causes; socket too loose, poor limb control, alignment of foot on the prosthesis, heel of the prosthesis too hard[12].
Knee instability (with ‘free knee’ prosthesis)
Causes; knee set too far anterior, heel cushion too firm, weak hip extensors, heel of the shoe too high causing the pylon of the prosthesis to move anteriorly, severe hip flexion contracture[8][11]
Foot slap
Causes; patient forcing foot contact to gain knee stability, heel cushion too soft, plantar flexion cushion too soft, excessive dorsiflexion[8][11][12]
Abducted gait- increased base of support during mobility, prosthetic foot placement is lateral to the normal foot placement during the gait cycle[12]
Causes; prosthesis too long, socket too small, suspension belt may be insufficient-band may be too far from the ileum, pain in the groin or medial wall of the prosthesis, hip abductor contractures, lateral wall of the prosthesis not supporting the femur sufficiently, socket of prosthesis abducted in alignment, fear/lack of confidence transferring weight onto prosthesis, alignment of the lower half of the pylon of the prosthesis in relation to socket[8][11][12]
Lateral trunk bending- Trunk flexes towards prosthesis during prosthetic stance phase
Causes: prosthesis too short, short stump length, weak or contracted hip abductors, foot outset excessively in relation to socket, lack of prosthetic lateral wall support, pain on the lateral distal end of the stump, lack of balance, habit[8][11][12]
Excessive pelvic lift on heel lift on prosthetic side
Causes; toe lever too long[8]
Pelvic dip on heel lift on prosthetic side
Causes; toe lever too short[8]
Increased lumbar lordosis
Causes; poor shaping of posterior wall of the prosthesis or pain on ischial weight bearing, resulting in anterior pelvic rotation, flexion contracture at the hip, weak hip extensor, habit, poor abdominal muscles, lack of support from the anterior wall of the socket, insufficient socket flexion[8][11][12]
Whip during swing phase
Causes; prosthetic knee alignment, incorrect donning of the prosthesis i.e. applied internally rotated or externally rotated weakness around femur, prosthetic too tight[8][12]
Socket dropping of when prosthesis lifted
Causes; insufficient suspension, socket too loose[8] • Delayed knee flexion during toe off (‘free knee only’) Causes; increased resistance of the prosthesis, Alignment of prosthesis[8].
Excessive heel rise
Causes; lack of friction on prosthetic knee, amputee generating more force then required to gain knee flexion, poor/lack of extension aid[8][11][12]
Reduced heel rise
Causes; locked knee, lack of hip flexion, too much friction on free knee, extension aid to tight[11]
Circumduction-lateral curvature of swing phase of prosthesis
Causes; prosthesis too long, fixed knee and poor hip hitching, poor suspension causing prosthesis to slip, excessive plantar flexion of the foot, abduction contractures, habit, weak hip flexors, socket too small, insufficient knee flexion[8][11][12]
Vaulting, amputee rises onto toe of the non prosthetic limb during prosthetic swing phase
Causes; prosthesis too long, habit, fear of catching toe on the floor, insufficient knee flexion (free knee) due to decreased confidence, lack of ‘hip hitching’ with a ‘locked/fixed knee’, poor suspension prosthesis-slips off during swing phase, socket too small, excessive friction on knee flexion of the prosthesis[8][10][11][12]
Forcible impact as knee goes into extension at end of terminal swing phase, just before heel strike
Causes; lack of friction of knee flexion, extension aid too excessive, absent extension bumper, amputee deliberately snaps knee into extension by excessive force to ensure extension[8][12]
Both Transfermoral and Transtibial[edit | edit source]
Uneven step length
Causes; fixed flexion deformity at knee, insufficient friction of prosthetic knee creating an increased step length on prosthetic side, hip flexion contracture, pain leading to decreased weight bearing on prosthetic side[8][12]
Uneven arm swing- arm on the prosthetic side is held close to the body
Causes; poor prosthetic fit, poor balance, fear and habit[12]
Unequal weight bearing/reduced stance phase on prosthesis
Causes; poor fitting socket leading to reduced stability, pain, muscle weakness, poor balance, fear and insecurity, poor extension aid or insufficient knee friction resulting in early excessive heel off and reduce stance time on prosthesis, inadequate prosthetic foot position[12]
This is not an exhaustive list and the deviation described for each level of amputation is not exclusive to that level, but is more likely to occur for that amputation.
Summary[edit | edit source]
Amputees should have a full functional and physical assessment and rehabilitation should be based around personalised functional goals. Individualised exercise programmes are developed thorough assessment. An awareness of normal gait and the deviations and their cause formulates the basis of the correct rehabilitation of the individual[13][14]. There are numerous techniques that can be used during rehabilitation and not all of them will be appropriate for each individual, therefore the programme and technique must be applied to each individual and reviewed regularly to ensure it remains adequate[8][13]. The amputee’s previous level of activity, overall health and potential to improve needs to be taken into consideration when formulating a rehabilitation programme and should aim at translating the function gained in a controlled environment into their own home functional environment[13][14].
Resources[edit | edit source]
Exercises for Prosthetic Rehabilitation (ICRC)
Amputee Exercises (ICRC)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Fish DJ and Nielsen CP. Clinical Assessment of Human Gait. Journal of prosthetics and Orthotics 1993. 2(39).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 Perry J &amp;amp;amp;amp;amp;amp;amp;amp; Burnfield J.M Gait Analysis, Normal and Pathological Function. 2nd Ed. USA, SLACK Incorporated USA 2010
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Physiopedia. Gait Cycle http://www.physio-pedia.com/Gait_Cycle (accessed 5 February 2015)
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Malanga G &amp;amp;amp;amp;amp;amp;amp;amp; Delisa J.A. Section One: Clinical Observation. Office of rehabilitation Research and Development No Date. http://www.rehab.research.va.gov/mono/gait/malanga.pdf (accessed 6 February 2010)
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 University of Washington. Pathologic Gait: Musculoskeletal http://courses.washington.edu/anatomy/KinesiologySyllabus/PathGait1Ortho.pdf (accessed 5 February 2015)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Standford School of medicine #2 Gait Abnormalities http://stanfordmedicine25.stanford.edu/the25/gait.html (Accessed 5 February 2012)
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 Kishner's Gait Analysis after Amputation updated July 2013 http://emedicine.medscape.com/article/1237638-overview (accessed 3 February 2015)
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 8.15 8.16 8.17 8.18 8.19 8.20 8.21 8.22 8.23 8.24 8.25 8.26 8.27 8.28 8.29 8.30 8.31 8.32 8.33 Smith D,, Michael J, W and Bowker J,H American Academy of Orthopaedic Surgeons. Atlas of Amputations and Limb deficiencies. Surgical, prosthetic and rehabilitation Principles. 3rd Ed. USA. 2011
- ↑ 9.0 9.1 9.2 Australian Physiotherapists in Amputee Rehabilitation http://austpar.com (accessed 7 February 2015)
- ↑ 10.0 10.1 10.2 10.3 10.4 Berger N. Analysis of Amputee Gait. Chapter 14. Atlas of limb prosthetics: Surgical, Prosthetic and rehabilitation Principles. Abridged version. O&amp;amp;amp;amp;amp;amp;P Virtual library http://oandplibrary.org/alp/chap14-01.asp (accessed 5 February 2015)
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 11.14 Hunter New England. NSW Health Duff K. Prosthetic gait deviations. Page link on Australian Physiotherapist in Amputee Rehabilitation. http://www.austpar.com/portals/gait/docs-and-presentations/ProstheticGaitDeviations.pps (accessed 6 February 2015)
- ↑ 12.00 12.01 12.02 12.03 12.04 12.05 12.06 12.07 12.08 12.09 12.10 12.11 12.12 12.13 Evans S. Prosthetics Education Session. July 2012. Ottobock
- ↑ 13.0 13.1 13.2 Gailey R,S and Curtis R,C. Physical Therapy Management of Adult Lower-Limb Amputees. Atlas of Limb Prosthetics; Surgical Prosthetic and Rehabilitation Principles. Chapter 23. Abridged version. O and P Virtual Library
- ↑ 14.0 14.1 British association of Chartered Physiotherapists in Amputee Rehabilitation. Evidenced Based Clinical Guidelines for the Physiotherapy Management of Adults with Lower limb Prosthesis. CSP Clinical Guideline 03. November 2012