Detrusor Sphincter Dyssynergia
Introduction[edit | edit source]
According to the International Classification of Syndromes (ICS), detrusor sphincter dyssynergia (DSD) is "the impaired coordination between detrusor and sphincter during voiding due to a neurologic abnormality".[1]
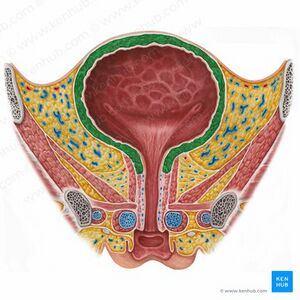
During normal micturition, the detrusor muscle of the bladder and the striated smooth muscle of the urethral sphincter work synergistically. The urethral sphincter relaxes during this process, and the detrusor contracts to push the bladder's urine into the urethra. The pontine micturition centre, a specialised region in the caudal brainstem, is in charge of controlling this synergy between the detrusor muscle and the external urethral sphincter. DSD is frequently caused by disruption of the pathways between this region to the caudal portion of the spinal cord.[2]
DSD refers to an involuntary detrusor contraction that is accompanied by an involuntary external sphincter contraction. This condition prevents adequate voiding and may result in hydronephrosis, renal scarring, a low compliant and thick-walled bladder, elevated retrograde pressures in the ureter and pelvis, and terminal kidney failure. [2]
For more info about the anatomy of the bladder, click here.
Pathophysiology[edit | edit source]
The detrusor relaxes when the pelvic nerve afferents are regulated by sympathetic output during normal filling, while keeping the bladder neck sphincter's tone in check. Input from the pontine micturition center (PMC) facilitates tonic activity of the EUS. The inhibitory impulses from the frontal cortex to the PMC are cut off during voluntary micturition, enabling activation of the micturition reflex. The PMC provides excitatory impulses to the bladder and blocks the spinal guarding reflexes. The detrusor contracts with synergistic relaxation of the external urinary sphincter (EUS) to lower urethral pressure while simultaneously increasing detrusor pressure, allowing urine to escape.[3][4][2]
DSD happens when there are neurological problems between the PMC and sacral spinal cord. Spinobulbospinal pathways are believed to be disrupted as a result, failing to inhibit spinal guarding reflexes, incorrectly activating Onuf's nucleus, causing EUS contraction to occur during detrusor contraction, and elevating detrusor pressures.[3][2][5]
Predisposing factors[edit | edit source]
- Multiple sclerosis (about 20-25% of people affected).[6][7]
- Spinal cord injury.[8][9]
- Spina bifida (about 50% of infants affected)[10]
- Transverse myelitis and other uncommon conditions affecting the spinobulbospinal tract.[11]
- Human T-cell Lymphotropic Virus 1 (HTLV-1).[12]
- Stroke.[13]
Clinical Presentation[edit | edit source]
- Urinary incontinence
- Urinary tract infections
- Bladder calculi
- Neurological symptoms
Diagnosis[edit | edit source]
- Electromyography (perineal surface electrodes or needle electrodes into the anal sphincter).[17][2]
- Voiding cystourethrogram (VCUG).[17][2]
Medical and Surgical Management[edit | edit source]
The management concepts are to lower intravesical pressure and promote bladder emptying.
- Antimuscarinic medications.
- Botulinum toxin.
- Alpha-adrenoceptor blockers.
- Nitric oxide.
- Catheterisation.
- Balloon dilatation.
- Urethral stents.
- External sphincterotomy.
Physiotherapy Management[edit | edit source]
- Behavioural interventions.[19]
- Kinesiotherapy as a form of pelvic floor muscle training.[20]
- Electrical stimulation of the bladder and pelvic floor muscles.[21]
- Pelvic floor exercises.
Resources[edit | edit source]
- ↑ Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Subcommittee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167-178.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Castro‐Diaz D, Taracena Lafuente JM. Detrusor‐sphincter dyssynergia. International Journal of Clinical Practice. 2006 Dec;60:17-21.
- ↑ 3.0 3.1 Sandananda P, Vahabi B, Drake MJ. Bladder outlet physiology in the context of lower urinary tract dysfunction . Neurourol Urodyn 2011 ; 30 , 708 – 11
- ↑ Klausner AP, Steers WD. The neurogenic bladder: An update with management strategies for primary care physicians . Med Clin N Am 2011 ; 95 : 111 – 20
- ↑ 5.0 5.1 Mahfouz W, Corcos J. Management of detrusor external sphincter dyssynergia in neurogenic bladder . Eur J Phys Rehabil Med 2011; 47:1 – 12
- ↑ Stoffel JT. Contemporary management of the neurogenic bladder for multiple sclerosis patients. Urol Clin North Am 2010;37:547-57.
- ↑ Araki I, Matsui M, Ozawa K, et al. Relationship of bladder dysfunction to lesion site in multiple sclerosis. J Urol April 2003;169:1384-7.
- ↑ Schurch B, Schmid DM, Karsenty G, et al. Can neurologic examination predict type of detrusor sphincter-dyssynergia in patients with spinal cord injury? Urology 2005;65:243-6.
- ↑ Bellucci CH, Wöllner J, Gregorini F, et al. Acute spinal cord injury--do ambulatory patients need urodynamic investigations? J Urol 2013;189:1369-73.
- ↑ Bauer SB, Dieppa RA, Labib KK, et al. Predictive value of urodynamic evaluation in newborns with myelodysplasia. JAMA 1984;252:650-2.
- ↑ Gliga LA, Lavelle RS, Christie AL, et al. Urodynamics findings in transverse myelitis patients with lower urinary tract symptoms: Results from a tertiary referral urodynamic center. Neurourol Urodyn 2015;34:507-12.
- ↑ Castro NM, Freitas DM, Rodrigues W, et al. Urodynamic features of the voiding dysfunction in HTLV-1 infected individuals. Int Braz J Urol 2007;33:238-44; discussion 244-5.
- ↑ Meng NH, Lo SF, Chou LW, et al. Incomplete bladder emptying in patients with stroke: is detrusor external sphincter dyssynergia a potential cause? Arch Phys Med Rehabil 2010;91:1105-9.
- ↑ Rivas DA, Chancellor MB. Neurogenic vesical dysfunction . Urol Clin North Am 1995 ; 22 : 579 – 91
- ↑ Reynard JM, Vass J, Sullivan ME, Mamas M. Sphincterotomy and the treatment of detrusor-sphincter dyssynergia: current status, future prospects .Spinal Cord 2003 ; 41 : 1 – 11
- ↑ Blaivas JG, Sinha HP, Zayed AA, Labib KB. Detrusor-external sphincter dyssynergia: a detailed electromyographic study . J Urol 1981 ; 125 : 545 – 8
- ↑ 17.0 17.1 Stoffel JT. Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies. Translational andrology and urology. 2016 Feb;5(1):127.
- ↑ Ahmed HU, Shergill IS, Arya M, Shah PJ. Management of detrusor–external sphincter dyssynergia. Nature Clinical Practice Urology. 2006 Jul 1;3(7):368-80.
- ↑ Skaudickas D, Kevelaitis E. Modern approach to treatment of urinary incontinence. Medicina (Kaunas). 2011;47(10):541-547. Available from: http://medicina.kmu.lt/1007/1007-10l.pdf [Accessed March 10, 2011].
- ↑ Burgio KL. Update on behavioral and physical therapies for incontinence and overactive bladder: the role of pelvic floor muscle training. Curr Urol Rep. 2013;14:457-464.
- ↑ Andrade RC, Neto JA, Andrade L, Oliveira TS, Santos DN, Oliveira CJ, Prado MJ, Carvalho EM. Effects of physiotherapy in the treatment of neurogenic bladder in patients infected with human t-lymphotropic virus 1. Urology. 2016 Mar 1;89:33-9.
- ↑ Wikipedia Audio. Bladder sphincter dyssynergia - Wikipedia Article Audio. Available from: https://www.youtube.com/watch?v=mCnAFqim5yM [last accessed 16/7/2018]