Vertebral Fractures in Children and Adolescents
Original Editor - User Name
Top Contributors - Daisy Meffan, Alexia Derbyshire, Cindy John-Chu and Angeliki Chorti
Definition/Description[edit | edit source]
A spinal fracture happens when a vertebral body collapses and when this happens in the paediatric population the bones are still developing and therefore can have severe consequences. A vertebral fracture is less obvious compared to a long bone fracture and is often very painful [35].
Clinically Relevant Anatomy[edit | edit source]
C- spine:
- Epiphyseal variants
- Epiphyseal plates are smooth and regular and have sclerotic lines
- Unique vertebral architecture
- Incomplete ossification of synchondroses and apophyses
- Hyper-mobility
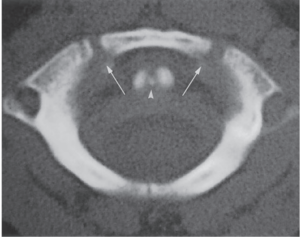
C1:
- Anterior arch is ossified in only 20% of cases at birth
- Becomes visible as an ossification centre by 1 year of age
- Neural arches appear in 7th foetal week
- Anterior arch fuses with the neural arches by 7
- Non-fusion before this can be mistaken for a fracture
- The neural arches fuse posteriorly by 3 years of age.
- Occasionally, the anterior ossification centre of C1 does not develop and the neural arches attempt to fuse anteriorly- This fusion abnormality can be differentiated from a fracture in that it demonstrates sclerotic margins
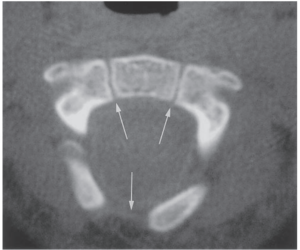
C2 (the axis, has the most complex and unique development of all vertebrae):
There are four ossification centres at birth:
- One for each neural arch
- One for the body
- One for the odontoid process
The odontoid process forms in utero from two separate ossification centres that fuse in the midline by the 7th foetal month. A secondary ossification centre appears at the apex of the odontoid process (os terminale) between 3 and 6 years of age and fuses by age 12 years. The body of C2 fuses with the odontoid process by 3–6 years of age. This fusion line (subdental synchondrosis), or the remnant of the cartilaginous synchondrosis, can be seen until age 11 years and may be confused with a fracture. The neural arches fuse posteriorly by 2–3 years of age and with the body of the odontoid process between 3 and 6 years of age [14],[16],[15],[33],[25]. C3 through C7 can be discussed as a unit because they exhibit the same developmental pattern.
Three ossification sites are present:
- The body - which arises from a single ossification site
- The two neural arches
The neural arches fuse posteriorly by age 2–3 years, and the body fuses with the neural arches between 3 and 6 years of age. Additionally, secondary ossification centres may be seen at the tips of the transverse processes and spinous processes that may persist until early in the 3rd decade of life and simulate fractures. Secondary ossification centres can also appear at the superior and inferior aspects of the cervical vertebral bodies and remain unfused until early adulthood [2],[14],[16], [15],[33]
Ligaments in the C-spine:
- The anterior and posterior atlanto-occipital membranes extend from the upper aspect of C1 to the anterior and posterior aspects of the foramen magnum.
- The anterior atlantoaxial ligament extends from the anterior midportion of the dens to the inferior aspect of the anterior arch of C1.
- The tectorial membrane is the superior extension of the posterior longitudinal ligament and attaches to the anterolateral aspect of the foramen magnum.
- The transverse ligament extends from the tubercle on the inner aspect of one side of the atlas to the tubercle on the other side.
- The apical ligament lies between the superior longitudinal fasciculus of the cruciform ligament and the anterior atlanto-occipital membrane.
- The alar ligaments connect the lateral aspect of the dens and the medial inferior aspect of the occipital condyles- the main function of the alar ligaments is to limit rotation to the contralateral side [14],[15], [33],[8].
Paediatric Versus Adult Cervical Spine[edit | edit source]
Cervical spine injuries in children usually occur in the upper cervical spine from the occiput to C3. This fact may be explained by the unique biomechanics and anatomy of the paediatric cervical spine.
- The fulcrum of motion in the cervical spine in children is at the C2-C3 level; in the adult cervical spine, the fulcrum is at the C5-C6 level [17][28].
- The immature spine is hypermobile because of ligamentous laxity, shallow and angled facet joints, underdeveloped spinous processes, and physiologic anterior wedging of vertebral bodies, all of which contribute to high torque and shear forces acting on the C1-C2 region.
- Incomplete ossification of the odontoid process, a relatively large head, and weak neck muscles are other factors that predispose to instability of the paediatric cervical spine [23],[28],[16],[15],[33],[22],[4].
Kyphosis and Lordosis[edit | edit source]
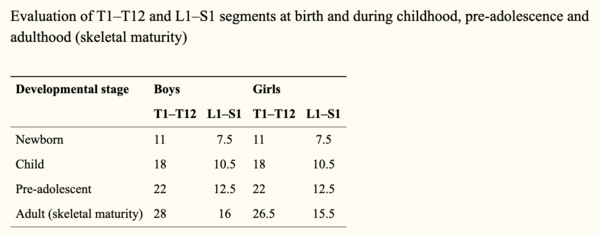
Kyphosis and lordosis are shown to increase at a linear rate from a child to adolescent age.
- Kyphotic curves increase from 25° at 7 years of age to 38° at 19 years of age (kyphotic angle = 25° + 0.58 × age)
- Lordotic curves increase from 22° at 5 years of age to 32° at 20 years of age (lordotic angle = 24° + 0.51 × age).
- There were no differences between males and females. [39]
Epidemiology/Aetiology[edit | edit source]
Spinal fractures make up only 1-3% of all paediatric fractures [7]. This is less incidence than in the adult population due to the child’s spine being more mobile and elastic and having a smaller mass compared to adults [26]. Bone structure and strength are considered a vital predictors of fracture occurrence [34] in children a bone mass reduction of 6.4% doubles the risk of fracture [6]. The incidence of these fractures are higher in children under the age of 5 and over the age of 10 years [30]. Spinal fractures in adolescents can have devastating consequences such as spinal deformity, scoliosis and Syringomyelia [30].
The cervical spine is the most common location for factures in infants, because of the anatomy of the infant spine such as a heavy head and less muscular development of the neck which puts more strain on the spine [30]. As previously mentioned, the paediatric spinal anatomy is different to the adult which predisposes children to flexion and extension injuries. Some of these differences include the facet joints being orientated different meaning there is a greater mobility but worse stability in the spine [7].
The IV discs are strong and vertebral end plate hard meaning this child’s spine has a higher resistance against compression forces (30). A Japanese study found a high stress distribution in the anterior compartment in children's spines predisposing this area in particular to fractures. Paediatric spinal fractures are normally caused by high impact and speed injuries. These include predominantly falls, sporting impact injuries and road traffic accidents. These include predominantly falls, sporting impact injuries and road traffic accidents. The most common fractures are compression fractures where the vertebrae bodies collapse.
In a review by Tan et al [34] bone strength was the main outcome assessed which was defined as the ability to resist fractures including bones extrinsic properties of bone mineral mass and distribution of bone mass. Studies provide strong evidence of the relationship between physical activity on bone mass due to concentric and eccentric muscle contractions caused during physical activity which cause high loads being placed on the skeleton [34].
In the review by Tan et al [34] all physical activities and observational studies were included; it was found that bone apposition (diameter) was highly related to pubertal stage, fracture incidence peaks at early puberty, 10-12 year in girls and 13-15 years in boys [6].
Mechanism of Injury[edit | edit source]
Neck fractures are common in children due to their disproportionately large head in comparison to weak neck muscles, which cause a bending movement on impact that is larger than the neck muscles can protect from. The upper cervical facet joints are also horizontally orientated and shallow with laxity in the ligaments [19] Usually ligament laxity prevents injury in other body parts by transferring energy however this property is not shared by the spinal cord [19].
Due to the positioning of the paediatric spine and it's increased elasticity from the increased cartilage and intervertebral disc thickness, there has to be a considerable amount of force obtained to cause an unstable fracture [26].
- Motor Vehicle accidents – both passengers and pedestrians (Most Common) [19][30]
- Cycling
- Falls from a height (also common)[19][ 30]
- Sporting Injuries [30][19]
- Assault
Fractures Types
Contiguous compression fractures - common in paediatric spinal injury due to the increased C- spine mobility, commonly linked to flexion movements, however increased mobility does mean there is reduced neurological compromise [19]
Burst fractures – make up only 10% of all thoracolumbar injuries in paediatrics due to the increase in spinal flexibility meaning the pressure isn't concentrated in one area - the common cause of burst fractures. This also reduces neurological damage along the increased size of the paediatric spinal canal compared to the spinal cord and cauda equina [19]
Chance fracture – common in children when wearing lap belts in motor traffic accidents. The seat belt acts as a fulcrum causing hyperflexion, commonly seen alongside intra-abdominal and head injuries [19].
Impression fractures [30]
Apophyseal ring fractures - only found in the paediatric population. Normally seen in adolescents and occurs due to the ring apophysis and the vertebral body not fusing completely and may separate in the process [12].
Characteristics/ Clinical Presentation[edit | edit source]
Signs and Symptoms
- Commonly seen with associated severe and frequently fatal injuries [19]
A 10 year report at a children's university hospital, found symptoms were: [19] and [30]
C-spine Fracture
- neck pain
- neurological deficit
- fixed abnormal head positions
- Common Additional Injuries - facial/head injuries, skull and facial fractures, facial lacerations, intercranial injury
T-spine Fracture
- back pain
- ecchymoses (skin discolouration due to bleeding below skin)
- localised tenderness
- neurological deficit
- Common Additional injuries - simple or multiple rib fractures, fractured sternum, pulmonary contusion, abdominal/visceral injuries including splenic haematoma
L-spine Fracture
- Back pain
- ecchymoses (skin discolouration due to bleeding below skin)
- localised tenderness
- abdominal pain
Due to children having a larger spinal canal than their spinal cord they can tolerate more compression than adults can before neural damage
Make sure to look for fractures at all levels of the spine (C-spine, T-spine and L-spine) when assessing for potential spinal fracture [30]
Prevalence[edit | edit source]
In children below 5 the most common area to injure was T8 followed by lumbar [30]
Between the ages of 5-10 the most common fracture area was the thoracolumbar region [30]
In teenagers the most common area begins to shift to the lumbar spine [30]
From 15 years and older the lumbar area is most affected [30]
Differential Diagnosis[edit | edit source]
- Low Back Pain
- Spondylosis
- Juvenile Ankylosing Spondylitis
- Disc Herniation
- Spinal cord injury without radiographic abnormality
Diagnostic Procedures[edit | edit source]
- Sensation of ‘breath arrest’ - immediately after the trauma the children would feel extremely short of breath, this is a predictive factor for vertebral fracture, particularly thoracolumbar fractures.
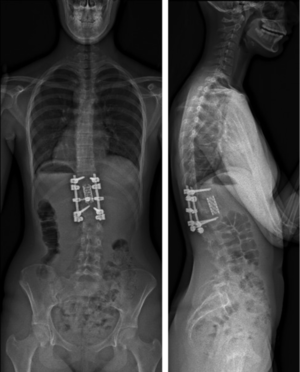
- X-ray – due to cartilaginous nature of the vertebra, fractures were not always clear from routine x-rays and children can go undiagnosed.
- MRI – used to determine diagnosis of potential fractures shown on x-ray, they give clear images of the vertebra allowing for more accurate diagnosis. This allows for direct visualisation and confirmation of the fracture, where it is in the spine and what type of fracture has occurred.
- CT scan – CT scans have better prognostic ability than x-ray as they show bony details in higher definition than an x-ray, its therefore more likely to get a clearly diagnosis from a CT scan than x-ray. However, like with x-rays fractures can go unnoticed on CT scans, therefore if there is any doubt about the potential of a fracture it will be followed up with an MRI scan to clarify a potential diagnosis.
- Flexion/Extension C-spine x-rays – often used after CT scans if no findings are present to determine if there is any undiagnosed cervical instability
[20], [9], [24]
Other Diagnostic Tools:
Nexus criteria – National Emergency R-ray Utilisation Group criteria assess low-risk patients for cervical spine injury, it is primarily used to determine if an x-ray is required or if further imaging is needed after an x-ray to determine possible diagnosis.
Nexus criteria [32]:
- Absence of midline cervical tenderness
- No evidence of intoxication
- Normal level of alertness
- Normal neurological exam
- Absence of a painful, distracting injury
Canadian C-spine Rule – these are a set of guidelines to help a clinician decide if cervical imaging (i.e. x-ray, CT or MRI scan) are appropriate for trauma patients. However, for children consideration needs to be taken around developmental stage, so applying these rules can be difficult.
C-spine rules[11]:
- Any high-risk factors which mandate radiography
- Dangerous mechanism of injury
- Age > 65
- Paraesthesia in extremities
- Any low-risk factor which allows safe assessment of range of motion
- Simple rear-end motor vehicle collision
- Sitting position in ED
- Ambulatory at any time
- Delayed onset of neck pain
- Absence of midline spine tenderness
- Able to actively rotate neck
- 45 degrees left and right
Management[edit | edit source]
Conservative Management
- Casting - There are two types, Minerva and Plaster and usually stay on for period of around 2 months [26]
- Halo Vests - to be worn for an average of 8 weeks [26]
- Bed Rest - until acute symptoms subside, followed by a moulded body cast [26]
In a case series of adolescents below the age of 16 with traumatic spine injury, in the 44 patients, 20 had stable injuries and were managed conservatively with the above methods. It was identified that the three cervical fractures, and nine wedge-shaped compression fractures, healed without significant deformity [26]. The eight stable burst fractures managed with conservative management showed the vertebral body had non-perfect reconstruction, however at follow up the maximum deformity was maximum 10 degrees involving one vertebrae above and below [26]. The remaining six fractures that were conservatively managed, all had significant angular deformities [26].
Conservative management, particularly of wedge fractures without neurological lesions can be successful, leaving only moderate residual deformities, however it is important there is an accurate diagnosis to confirm the stability of the fracture to ensure accurate and correct treatment is provided [26].Whilst nonoperative treatment is viable for burst fractures in children with no neurological deficits and minimal initial kyphosis, operative treatments are recommended for unstable burst fractures to correct the deformity [26].
Angelliaume et al, 2017 [1]:
- In a case of a stable spinal fracture without neurological deficiency, conservative treatment must be the first treatment of choice in children
- The significant difference between the initial and the final local kyphosis at the thoracic level was not found for the lumbar level.
- It is hypothesized that the brace is more efficient at the thoracic level than at the lumbar level and enables more remodelling, decreasing compressive forces by an antikyphotic effect- furthermore, it is easier to correct a thoracic kyphosis than a lumbar one using an antikyphotic brace
Functional outcomes:
- Functional results indicated a high rate of back pain.
- However, patients’ functional results were satisfactory because they reported no limitations in their daily life activities and did not use painkillers.
- Variable rates of functional outcomes have been reported, with 12–57% incidences of back pain after a conservative treatment
- However, rates of back pain in adolescents without back injury are also high, with a prevalence of 7–70% .
Surgical Management
Overall surgical interventions depends on the type and severity of the fracture. The Denis classification can be used to differentiate between a stable and a unstable vertebral fracture which can help decide on management options. Generally according to the evidence lots of stable fractures can be treated conservatively however unstable fractures will require surgical management [31][26] Furthermore if the patient has a neurological deficit or a spinal cord injury, surgery is necessary to stabilise the fracture and gain neurological function [10]. Surgical outcomes within the population have been positive, Vander et al [36] found surgical intervention was positive in ensuring the correction of the kyphosis of the spine compared to conservative management that which led to worsening of kyphosis.
Types of surgery can vary depending on the type of fracture and the age. Adolescent’s can be treated using adult type instrumentation due to a more developed spine [31], where as younger children have smaller pedicles so a normal screw placement in this area can be challenging [31]. Evidence suggest a shorted fusion is the prefered approach in peadiactric fractures in order to preserve growth and mobility [18]. In the lumbar spine, lumbar fusion can be used which involves fusing the vertebral bodies together so no movement can occur between them enabling the fracture to be repaired, this can be managed via a posterior approach [5]. If the fracture is more severe reconstruction surgery such as vertebroplasty or kyphoplasty can take place [5]. Although conservative management has been proven to correct initial conditions and deformity’s these deformities can return overtime leading to a short term fix as opposed to a long term fix.
Prevention[edit | edit source]
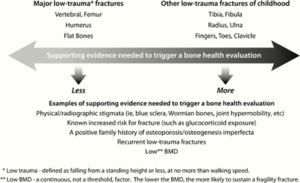
Over recent years there has been an increased recognition of the need to identify children with bone fragility [37], this is due to osteoporosis being thought to root from childhood therefore preventative efforts should be initiated in early life to ensure life-long bone health [13].
- calcium: intake during infancy, childhood and adolescents contribute to bone mass gain. Dietary supplementations may be offered to those who cannot intake enough calcium. [13].
- vitamin D: testing for vitamin D deficiency is recommended for those who have recurrent traumatic fractures even on low-impact. [13].
- mechanical loading and weight bearing exercise: puts force on the skeleton that increases bone formation [13]. In a review by Tan et al [34] bone strength was the main outcome assessed which was defined as the ability to resist fractures including bones extrinsic properties of bone mineral mass and distribution of bone mass. Studies included in the review provided strong evidence of the relationship between physical activity on bone mass due to concentric and eccentric muscle contractions caused during physical activity which cause high loads being placed on the skeleton [34].
Dual Energy X-ray absorptiometry (DXA) is the most used method of assessment for bone mass, its preferred due to low radiation and is used commonly used for the lumbar [13]. Fracture risk not only depends on the factors above but also history of fractures, there is growing literature showing an association between low bone mass measured using DXA and increased fracture risk in children. [13].In adolescent females if mensuration has not occurred for more than 6 months then a DXA should be considered and clinicians, athletes and parents should be educated on female the athlete triad [13].
There is a need to evaluate each child on an individual basis to identify if they need a bone health evaluation, in the diagram below (13) it can be seen that health factors should be considered in the decision of whether to conduct a bone health evaluation, for example joint hypermobility or family history of osteoporosis [37]
An additional consideration is road traffic safety, Leonard et al [19] investigated paediatric spinal trauma and associated injuries found that those who were restrained by a lap belt in rear of a vehicle whereby head on collision occurred leads to smaller children particular to ‘submarine’ beneath the belt causing hyperflexion of the spine to take-place. Associated injuries from this causes included both intra-abdominal and head injuries [19]. To prevent these injuries cross-body seat belts and booster seats where needed should be used.
References[edit | edit source]
1. Angelliaume A, Simon AL, Boissière L, Bouty A, de Gauzy JS, Vital JM, Gille O, Tournier C, Aunoble S, Pontailler JR, Lefèvre Y. Conservative treatment of pediatric thoracic and lumbar spinal fractures. Journal of Pediatric Orthopaedics B. 2017;26(1):73-9.
2. Bailey DK. The normal cervical spine in infants and children. Radiology. 1952 Nov;59(5):712-9.
3. Behringer M, Vom Heede A, Yue Z, Mester J. Effects of resistance training in children and adolescents: a meta-analysis. Pediatrics. 2010 Nov 1;126(5):e1199-210.
4. Bilston LE, Brown J. Pediatric spinal injury type and severity are age and mechanism dependent. Spine. 2007 Oct 1;32(21):2339-47.
5. Boddu, S., 2020. Surgery for Spinal Compression Fractures. [online] Weill Cornell Brain and Spine Center. Available at: <https://weillcornellbrainandspine.org/condition/spinal-compression-fractures/surgery-spinal-compression-fractures> [Accessed 21 May 2021].
6. Boreham CA, McKay HA. Physical activity in childhood and bone health. British journal of sports medicine. 2011 Sep 1;45(11):877-9.
7. Bouyer, B., Vassal, M., Zairi, F., Dhenin, A., Grelat, M., Dubory, A., Giorgi, H., Walter, A., Lonjon, G., Dauzac, C. and Lonjon, N., 2015. Surgery in vertebral fracture: Epidemiology and functional and radiological results in a prospective series of 518 patients at 1year's follow-up. Orthopaedics & Traumatology: Surgery & Research, 101(1), pp.11-15.
8. CATTELL HS, FILTZER DL. Pseudosubluxation and other normal variations in the cervical spine in children: A study of one hundred and sixty children. JBJS. 1965 Oct 1;47(7):1295-309.
9. Cui S, France J. Fractures of the Spine in Children [Internet]. Ota.org. 2016 [cited 18 May 2021]. Available from: https://ota.org/sites/files/2018-06/P13-Fractures%20of%20the%20Spine%20in%20Children.pdf
10. Ferrero, E., Compagnon, R., Pesenti, S., Lefèvre, Y., Polirsztok, E., Ilharreborde, B. and Sales de Gauzy, J., 2020. Surgical management of burst fractures in children and adolescents: A Multicentre Retrospective Study. Orthopaedics & Traumatology: Surgery & Research, 106(1), pp.173-178.
11. Fox S. Paediatric Cervical Spine Injury [Internet]. Pediatric EM Morsels. 2019 [cited 18 May 2021]. Available from: https://pedemmorsels.com/pediatric-cervical-spine-injury.
12. Gadi, D., Kumar, R., Grover, A. and Raghavendra, R., 2015. Lumbar Apophyseal Ring Fracture- A Case Report. JOURNAL OF CLINICAL AND DIAGNOSTIC RESEARCH, 9(5).
13. Golden NH, Abrams SA. Optimizing bone health in children and adolescents. Pediatrics. 2014 Oct 1;134(4):e1229-43.
14. Gray’s anatomy. 37th ed. Philadelphia, Pa: Lea & Febiger, 1989.
15. Harris JH, Harris JH, Mirvis SE. The radiology of acute cervical spine trauma. Lippincott Williams & Wilkins; 1996.
16. Herman MJ, Pizzutillo PD. Cervical spine disorders in children. Orthopedic Clinics of North America. 1999 Jul 1;30(3):457-66.
17. Kokoska ER, Keller MS, Rallo MC, Weber TR. Characteristics of pediatric cervical spine injuries. Journal of pediatric surgery. 2001 Jan 1;36(1):100-5.
18. Lalonde, F., Letts, M., Yang, J. and Thomas, K., 2001. An analysis of burst fractures of the spine in adolescents. American Journal of Orthopeadics, 2(30), pp.115-120.
19. Leonard M, Sproule J, Mc Cormack D. Paediatric spinal trauma and associated injuries. Injury. 2007 Feb 1;38(2):188-93.
20. Leroux J, Vivier P, Ould Slimane M, Foulongne E, Abu-Amara S, Lechevallier J et al. Early diagnosis of thoracolumbar spine fractures in children. A prospective study. Orthopaedics & Traumatology: Surgery & Research[Internet]. 2013 [cited 18 May 2021];99(1):60-65. Available from: https://pubmed.ncbi.nlm.nih.gov/23276683/
21. Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K, Brown JH, Diamond AS, Black K, Singh S. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003 May;23(3):539-60
22. Marx Rosen’s emergency medicine: concepts and clinical practice. 5th ed. St Louis, Mo: Mosby, 2002; 274–276
23. McGrory BJ, Klassen RA, Chao EY, Staeheli JW, Weaver AL. Acute fractures and dislocations of the cervical spine in children and adolescents. The Journal of bone and joint surgery. American volume. 1993 Jul 1;75(7):988-95.
24. Murphy A, Knipe H. Cervical spine (flexion and extension views) [Internet]. Radiopaedia.org. 2015 [cited 18 May 2021]. Available from: https://radiopaedia.org/articles/cervical-spine-flexion-and-extension-views
25. Ogden JA. Radiology of postnatal skeletal development. Skeletal radiology. 1984 Sep;12(3):169-77.
26. Parisini, P., Silvestre, M. and Greggi, T., 2002. Treatment of Spinal Fractures in Children and Adolescents. Spine, 27(18), pp.1989
27. Rizkalla, J., Lines, T. and Nimmons, S., 2019. Classifications in Brief: The Denis Classification of Sacral Fractures. Clinical Orthopaedics & Related Research, 477(9), pp.2178-2181.
28. Roche C, Carty H. Spinal trauma in children. Pediatric radiology. 2001 Oct;31(10):677-700.
29. Sairyo, K., Goel, V., Masuda, A., Vishnubhotla, S., Faizan, A., Biyani, A., Ebraheim, N., Yonekura, D., Murakami, R. and Terai, T., 2006. Three-dimensional finite element analysis of the pediatric lumbar spine. Part I: pathomechanism of apophyseal bony ring fracture. European Spine Journal, 15(6), pp.923-929.
30. Saul, D. and Dresing, K., 2018. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatric Reports, 10(1).
31. Sayama, C., Chen, T., Trost, G. and Jea, A., 2014. A review of pediatric lumbar spine trauma.
32. Stiell I. Prospective Validation of the NEXUS Low-risk Criteria for Cervical Spine Radiography. Academic Emergency Medicine [Internet]. 2002 [cited 18 May 2021];9(5):360-360. Available from: https://www.sciencedirect.com/science/article/pii/S019606440301117X
33. Swischuk LE. Emergency imaging of the acutely ill or injured child. Lippincott Williams & Wilkins; 2000.
34. Tan VP, Macdonald HM, Kim S, Nettlefold L, Gabel L, Ashe MC, McKay HA. Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. Journal of bone and mineral research. 2014 Oct;29(10):2161-81.
35. Todd, S. and Di Marco, M., 2019. Vertebral Fractures in Children. [online] Smn.scot.nhs.uk. Available at: <https://www.smn.scot.nhs.uk/wp-content/uploads/2019/01/Vertebral-fractures-in-children.pdf> [Accessed 23 May 2021].
36. Vander Have, K., Caird, M., Gross, S., Farley, F., Graziano, G., Stauff, M. and Segal, L., 2009. Burst Fractures of the Thoracic and Lumbar Spine in Children and Adolescents. Journal of Pediatric Orthopaedics, 29(7), pp.713-719.
37. Ward LM, Weber DR, Munns CF, Högler W, Zemel BS. A contemporary view of the definition and diagnosis of osteoporosis in children and adolescents. The Journal of Clinical Endocrinology & Metabolism. 2020 May;105(5):e2088-97.
38. Dimeglio A, Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. European Spine Journal. 2012 Jan;21(1):64-70.
39. Giglio CA,Volpon JB. Development and evaluation of thoracic kypohsis and lumbar lordoduring growth. Journal of childrens orthopeadics. 2007 Sept 1;1 (3): 187
40. Kwok, S., 2013. Website review: KidsHealth. Journal of Paediatrics and Child Health, 49(12), pp.1085-1086.