Ventricular Fibrillation
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Uchechukwu Chukwuemeka and Nupur Smit Shah
Introduction[edit | edit source]
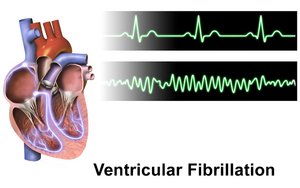
Ventricular fibrillation (VF) is considered the most serious cardiac arrhythmias. Disordered electrical activity causes the ventricles to quiver (or fibrillate) instead of contracting normally. This prevents the heart from pumping blood, causing collapse and cardiac arrest.
VF has been identified in nearly 70% of cardiac arrest patients. Without treatment, the condition is fatal within minutes. The rates of survival for VF patients outside the hospitals have increased slightly however many are left with residual anoxic brain damage and neurological deficits[1][2].
Etiology[edit | edit source]
The cause of ventricular fibrillation is not always known but it can occur during certain medical conditions. VF most commonly occurs during an acute heart attack or shortly thereafter. The root causes include: Coronary artery disease; Damage to the heart muscle from eg myocardial infarction; Cardiomyopathy; Electrolyte abnormalities (hypokalemia/hyperkalemia, hypomagnesemia); Acidosis; Hypothermia; Hypoxia; Alcohol use; Drug toxicity; Sepsis (severe body infection); Family history of sudden cardiac death.[1]
Epidemiology[edit | edit source]
The total annual burden of Out of Hospital Cardiac Arrest (OHCA) was estimated at 356,500 in 2017 in America. At least 23% of OHCA treated by Emergency Medical Service have VF/VT as the initial rhythm. With more than 60% of cardiovascular deaths resulting from cardiac arrest, it remains the leading cause of death worldwide.
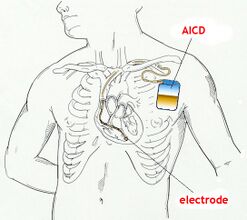
Modern advances in assistive devices such as implantable cardioverter-defibrillator (ICD) have had a significant impact on these numbers. [1][3].
Presentation[edit | edit source]
Symptoms of VF include:
- Near fainting or transient dizziness
- Fainting
- Acute shortness of breath
- Cardiac arrest
Diagnosis[edit | edit source]
Acute presentation of symptoms and ECG findings lead to the diagnosis.
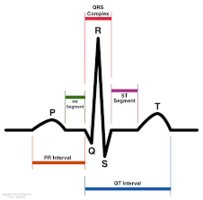
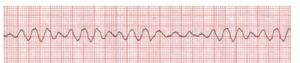
ECG Findings
- Fibrillation waves of varying amplitude and shape.
- No identifiable P waves, QRS complexes, or T waves
- Heart rate anywhere between 150 to 500 per minute
Patients surviving VF should have a thorough history and physical examination[1]. Including:
- Vital signs
- Overall health and medical history
- Description of symptoms that patient, a loved one, or a bystander provides
- A physical exam[4]
Treatment[edit | edit source]
V-fib comes on quickly and needs prompt treatment. Steps involved:
- Cardiopulmonary resuscitation (CPR) to keep blood moving
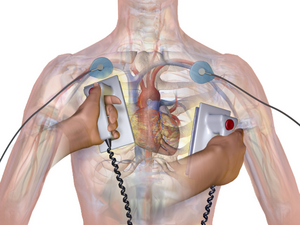
- Defibrillation/Cardioversion
- Medication to make the rhythm stable again
Less Frequent Action
- Catheter ablation. This procedure uses energy to destroy small areas of your heart affected by the irregular heartbeat. This rarely used procedure for V-fib looks to eliminate electrical triggers of V-fib.
- Left cardiac sympathetic denervation. This is a surgical procedure that may help if there's a frequent V-fib events. It is not yet commonly used and is reserved for people with uncontrolled V-fib with a genetic[4] predisposition.
Prognosis[edit | edit source]
Prognosis of VF depends on the time from onset to early intervention and defibrillation. Shorter delays are associated with survival rates as high as 50%.
VF outside the hospital can be reversed, as today there are defibrillators available in many places. The success of reversal declines at a rate of 5-10% for every minute that is delayed. Unfortunately many develop residual neurological deficits because of anoxia. Full recovery is rare[1].
Physiotherapy[edit | edit source]
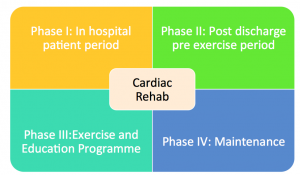
The health professional team may advise cardiac rehabilitation following hospitalisation and stabilisation of condition.
Cardiac rehabilitation is a complex, interprofessional intervention customized to Coronary artery disease (CAD); Myocardial infarctions.
Risk Reduction[edit | edit source]
Those at risk for ventricular fibrillation and its serious consequences, the doctor may recommend:
- Arrhythmia medications, which can help control rhythm disturbances
- An implantable cardioverter defibrillator (ICD), which can correct abnormal heart rhythms
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Ludhwani D, Goyal A, Jagtap M. Ventricular Fibrillation.Available: https://www.ncbi.nlm.nih.gov/books/NBK537120/(accessed 28.2.2022)
- ↑ Heart org.Ventricular Fibrillation Available:https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/ventricular-fibrillation (accessed 28.2.2022)
- ↑ Wiki doc. Ventricular tachycardia epidemiology and demographics Available: https://www.wikidoc.org/index.php/Ventricular_tachycardia_epidemiology_and_demographics(accessed 28.2.2022)
- ↑ 4.0 4.1 John Hopkins VF Available:https://www.hopkinsmedicine.org/health/conditions-and-diseases/ventricular-fibrillation (accessed 1.3.2022)
- ↑ Dr. John Campbell.Ventricular fibrillation causes cardiac arrest. Available from: http://www.youtube.com/watch?v=Xq0gNFcBJXc [last accessed 30/4/2022]