Vasodilators
Introduction[edit | edit source]
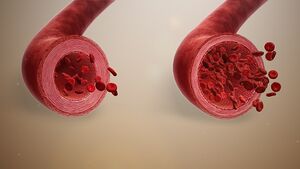
Vasodilators are medicines that dilate blood vessels allowing blood to flow more easily through. They are useful in the management of hypertension, angina, heart failure, myocardial infarction, and more.
There are different classes of vasodilators used today in the current clinical practice, and each has different actions on the coronary arteries and peripheral vasculature (arteries and veins). Vasodilators most commonly affect the arteries in the human body, however some vasodilators eg nitroglycerin can affect the venous system of the body predominantly[1].
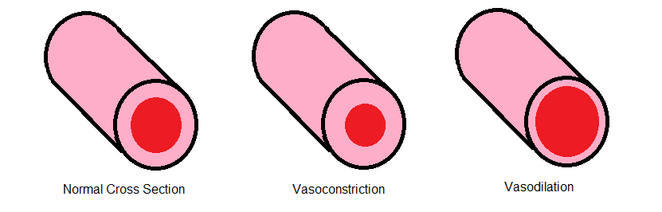
Vasodilators dilate or prevent constriction of the blood vessels, which allow greater blood flow to various organs in the body.[1][2]
Pharmacodynamics[edit | edit source]
The drug class of vasodilators treat hypertension by directly vasodilating blood vessels in the periphery.
- Vasodilators decrease resistance in the blood vessels resulting in a decrease in blood pressure.[3]
- Direct-acting vasodilators dilate arterioles specifically, without having a dilating effect on the venous system.[4]
- Many antihypertensive drugs ultimately produce vasodilation through a cascade of events. This class of antihypertensive drugs produce vasodilation by acting directly on the smooth muscle of the vasculature in the periphery.[5] Specifically, direct-acting vasodilators stimulate intracellular components by activating phosphorylation of cyclic-adenosine monophosphate (cAMP) and cyclic-guanosine monophosphate (cGMP).[3] These cyclic second-messengers inhibit smooth muscle contraction, as well as platelet aggregation.[3]
Pharmacokinetics and Adverse Effects[edit | edit source]
Direct vasodilators are usually not the first in line in the treatment of hypertension.
This class of drugs
- Have a fairly short half-life, which requires frequent doses throughout the day.[6]
- Primarily metabolized by the liver and excreted via the kidneys.[4]
While vasodilators are successful in controlling hypertension, these medications possess a myriad of side effects.
- Reflex tachycardia is the primary adverse effect of these drugs, as a consequence of the medication induced baroreflex response compensating for the sudden medication decrease in vascular resistance.
- Other less serious side effects include orthostatic hypotension, dizziness, weakness, fluid retention and nausea.[7]
PTs should be mindful of potential implications of adverse effects of these drugs or contraindications to therapy in patients.
Classes[edit | edit source]
Below are the specific mechanisms of action for different classes of vasodilators:
- ACE Inhibitors: Prevent the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor.
- Angiotensin Receptor Blockers: Prevent angiotensin II from binding to its receptor.
- Nitrates: Increase the amount of NO in vascular smooth muscle cells, causing vasodilation. Nitrates dilate veins more than arteries and decrease preload.
- Calcium Channel Blockers: Block calcium channels in the cardiac and smooth muscles, causing decreased muscle contractility and vasodilation. There are two classes of CCBs: Dihydropyridines (act on the vascular smooth muscle), and non-dihydropyridines (act on the heart).
- Minoxidil: Directly relaxes arteriolar smooth muscle, with minimal effect on the vein.
- Hydralazine: the exact mechanism is still unknown.
- Beta-Blockers
See also Pharmacological Management of Hypertension
References:[edit | edit source]
- ↑ 1.0 1.1 Hariri L, Patel J. Vasodilators. 2020 Available:https://www.ncbi.nlm.nih.gov/books/NBK554423/ (accessed 6.4.2022)
- ↑ Drugs.com Vasodilators Available from: https://www.drugs.com/drug-class/vasodilators.html (last accessed 20.6.2019)
- ↑ 3.0 3.1 3.2 Walter U, Waldmann R, Nieberding M. Intracellular mechanism of action of vasodilators. European Heart Journal. 1988;9(suppl H):1-6. doi:10.1093/eurheartj/9.suppl_h.1.
- ↑ 4.0 4.1 Cohn JN, Mcinnes GT, Shepherd AM. Direct-Acting Vasodilators. The Journal of Clinical Hypertension. 2011;13(9):690-692.
- ↑ Carter B, Saseen J. Hypertension. 5th ed. New York , NY: McGraw-Hill; 2002.
- ↑ Patel P, Jneid H. Interventional Pharmacology-Vasodilators. The Cardiology Advisor. https://www.thecardiologyadvisor.com/cardiology/interventional-pharmacologyvasodilators/article/583886/. Published September 17, 2018. Accessed October 10, 2018.
- ↑ Ciccone CD. Pharmacology in Rehabilitation. 5th ed. Philadelphia: F.A. Davis Company; 2016.