Trigeminal Nerve
Original Editor - Saumya Srivastava
Top Contributors - Saumya Srivastava, Riccardo Ugrin, Wendy Walker, Kim Jackson, Ahmed M Diab and Vidya Acharya
Description[edit | edit source]
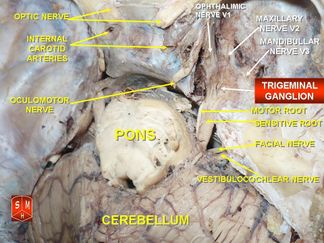
The Trigeminal Nerve is the fifth cranial nerve. It is also represented as CN V. It is the largest of all the cranial nerves. It is the most complex of all the cranial nerves due to it's extensive anatomic course. This nerve is a mixed nerve - having both sensory and motor fibres. The origin of the trigeminal nerve is the annular protuberance at the limit of the cerebellar peduncles[1]. It originates from three sensory nuclei (mesencephalic, principal sensory, spinal nuclei of trigeminal nerve) and one motor nucleus (motor nucleus of the trigeminal nerve) extending from the midbrain to the medulla[2].
Distal Roots and the Trigeminocervical Complex (TCC)[edit | edit source]
- More recent neuroanatomical and neurochemical studies revealed that most sensory fibres from the intracranial and the extracranial tissues originate in the trigeminal ganglion (TG). [3]
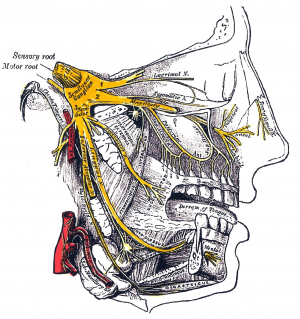
- Its sensory nuclei merge to form the sensory root at the level of the pons and the motor nucleus continues to form the motor root. As a result the sensory root of the trigeminal nerve is large (made up of about 50 fascicles)[1], while its motor root is more slender (composed of six or seven fascicles)[1].
- These roots are analogous to the dorsal and ventral roots of the spinal cord[2]. Fibers in the spinal trigeminal tract convey impulses concerned with thermal, tactile sense, and pain from the face, forehead, and mucous membranes of the nose and mouth[4]. The sensory root then expands into the trigeminal ganglion (TG), in the middle of the cranial fossa. The TG infact is located lateral to the cavernous sinus, in a depression of the temporal bone, known as the trigeminal cave[2].
- In addition to that the spinal trigeminal nucleus is described as a region of the upper cervical spinal cord where sensory nerve fibers in the descending tract of the trigeminal nerve (Pars Caudalis) are believed to interact with sensory fibers from the upper cervical roots. This functional convergence of upper cervical and trigeminal sensory pathways allows the bidirectional referral of painful sensations between the neck and trigeminal sensory receptive fields of the face and head[5]. As mentioned above the spinal trigeminal nucleus is a sensory tract descends to the caudal end of the medulla and to the spinal cord (as far as the third or fourth cervical level), where it becomes continuous with Lissauer’s tract and takes sensory information from different cranial nerves, including the trigeminal nerve and its branches.
- Because of that it is important to define the trigeminal ganglion and the spinal trigeminal nucleus as a Trigeminocervical Complex (TCC).
- The innervation of the face forms a somatotopic map in the TCC, which is stretched and distorted into the proportions of the Pars Caudalis of the spinal trigeminal nucleus.
- The primary function of the TCC is to carry information on temperature, deep or crude touch, and pain from the portion of the face. In addition to this major pathway, TCC is also responsible for conveying sensory and nociceptive signalling from the meninges and craniovascular structures to several higher order relays. Activation of these structures are believed to contribute to the perception of pain during migraine, and also to autonomic, endocrine, cognitive and affective symptoms that last throughout the migraine episode. Furthermore, the second order neurons receive inputs from the occipital nerve. This convergence may havemtreatment implications for some primary headache conditions as well as referred pain.[3]
- This neuroanatomically system could explain the clinical relation between headache, cervical pain and trigeminal sensory neuropathy. Infact clinically, trigeminal activation produces symptoms in the trigeminal and cervical territory and cervical activation produces symptoms in the cervical and trigeminal territory. The overlap between the trigeminal nerve and cervical is known as a convergence mechanism.[6]
- It is also demonstrated in animals the anatomic connection and neuroanatomical convergence[7] between the TG and the greater occipital nerve. Thus could also be clinical relevant for the treatment of headache and its correlation with cervical instability and trigeminal neuropathy[8]. This relation however has not still demonstrated in humans. The suggestion that the clinical improvement of occipital nerve blockades is not due to a direct inhibitory effect on trigeminal transmission is still controversial[9][10]
Peripheral Divisons of The Trigeminal Nerve into Branches-[edit | edit source]
The Trigeminal Nerve divides into 3 nerves distal to the trigeminal ganglion[11] -
- The Ophthalmic nerve (V1), passes forward in the lateral wall to the cavernous sinus. It then enters the orbit via the superior orbital fissure.
- The Maxillary nerve (V2), leaves the skull base through the foramen rotundum ossis sphenoidalis, inferolateral to the cavernous sinus. It then enters the pterygopalatine fossa, giving off several branches. The main trunk then continues anteriorly in the orbital floor and emerges onto the face as the infraorbital nerve
- The Mandibular nerve (V3), runs laterally along the skull base then exits the cranium by descending through the foramen ovale into the masticator space. The motor root of the trigeminal nerve bypasses the trigeminal ganglion and reunites with the mandibular nerve in the foramen ovale basis cranii. Hence the V3 is the only branch which contains both sensory and motor components:the Opthalmic (V1) and Maxillary (V2) nerves contain only sensory fibres.
This video explains the origin, course and distribution of the trigeminal nerve:
Function[edit | edit source]
It is a mixed nerve - the sensory part of the nerve supplies the face (includes touch, pain, and temperature) and the motor part is for muscles of mastication[11]. The sensory information is sent forth through the main trigeminal nucleus and nuclei of the thalamus before it travels to the cerebral cortex and synapses in the post-central gyrus. Just like any other sensory information of the body, the information from the face crosses over (decussates) to the contralateral brain hemisphere[13].
Motor -[edit | edit source]
- The motor root of the trigeminal nerve bypasses the trigeminal ganglion and reunites with the mandibular nerve in the foramen ovale basis cranii.
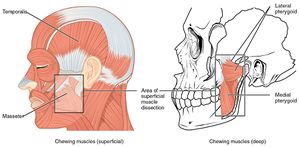
- The motor root of the mandibular nerve innervates the four muscles of mastication[13]
- Masseter,
- Temporalis muscle,
- The lateral pterygoids and
- The medial pterygoids.
- The muscles of mastication produce elevation, depression, protrusion, retraction, and the side-to-side movements of the mandible.
- Additionally, the motor component of the V3 also innervates the tensor veli palatini, the mylohyoid, the tensor tympani, and the anterior portion of the digastric muscle[13]
Sensory -[edit | edit source]
- The sensory components of the 3 branches carry pain, temperature and touch information from the skin of the face; mucosa of of the sinuses. nose and mouth; the teeth and portion of dura.
- They also carry proprioceptive information from the teeth, hard palate, tempomandibular joint and the muscles of mastication.
- The ophthalmic nerve is responsible for sensory innervation of the face and skull, derived from the frontonasal prominence, as well as the eye and portions of the nasal cavity[13]. It also contains sympathetic nerve fibers responsible for pupil dilation and supplies the ciliary body, iris, lacrimal gland, conjunctiva, and cornea[13]. Additionally also supplies the superior portion of the nasal cavity, the frontal sinus, and even deeper structures including the dura mater and portions of the anterior cranial fossa.
- The maxillary nerve innervates portions of the nasal cavity, sinuses, maxillary teeth, palate, and the middle portion of the face and skull above the mouth and below the forehead.
- The sensory fibres of the mandibular nerve are responsible for pain and temperature information from the mandibular teeth, buccal mucosa, temporomandibular joint, the face below the distribution of the maxillary nerve and the anterior two-thirds of the tongue; this is differentiated from taste which is produced by CN VII[13].
- The sympathetic and parasympathetic fibers, along with the 3 branches, are distributed to the nasal mucosa causing mucus secretion, to the pupil, to the sublingual glands, the lacrimal, the submaxillary glands and to the arterioles of the face.
Clinical Relevance[edit | edit source]
Knowing the course of the nerve further helps in understanding the relationship between the brainstem, skull base, and facial area.
- Trigeminal Neuralgia - is defined as sudden, brief, and excruciating facial pain attacks in one or more of the V branches. As a result, it leads to a severe reduction in the quality of life of affected patient. Its aetiology can be classified into idiopathic, classic and secondary[15]. For more information please read here.
- Trigeminal Neuralgia resulting from C2 fracture - The upper cervical spinal cord contains the spinal trigeminal tract and nucleus. Fibers with cell bodies in the trigeminal ganglion enter in the upper pons and descend caudally to C2 level. This case study reveals as the atlantoaxial instability after C2 spinal fracture could lead to a Trigeminal Neuralgia with facial pain.[4]
- Cluster Headaches - defined as unilateral headaches that affects the distribution of the Trigeminal Nerve. Along with the pain, they can be accompanied with nasal congestion, swelling, and lacrimation on the affected side. For more information please see here.
- Wallenberg Syndrome (Lateral Medullary Syndrome) - is defined as a condition in the which the lateral portion of the medulla in the brainstem gets damaged, like in case of a stroke. In this syndrome there is sensory loss in the distribution of the Trigeminal nerve on the same and contralateral sensory loss in the rest of the body. For more information please read here.
- Infections - generally occur in the peripheral divisions of the Trigeminal Nerve, mostly due to local tumours leading to direct spread and metastases from distant malignancies.
- Neoplasms[11] - just as infection, more common in the peripheral divisions of CNV. Extrinsic disease of the Meckel's cavity (which usually involves bony metastasis, chordoma, or chondrosarcoma) destroy adjacent bone as they extend toward the Meckel’s cavity and the Intrinsic disease of the same cavity simply expands it. Primary tumours of the Meckel’s cavity include epidermoid cyst, trigeminal schwannoma and meningioma.
- Trigeminal sensory neuropathy - upper cervical disc herniations patients can present with this kind of neuropathy with cervical extension of the spinal tract due to its anatomy in the brainstem. Common brainstem and upper cervical cord lesions which can lead to CN V symptoms include Multiple sclerosis, glioma, and infarction. Lesser common lesions include metastasis, haemorrhage, cavernous haemangiomas and arteriovenous malformation. Rarely, rhombencephalitis may develop as a result of retrograde extension of herpes simplex virus type 1 from the trigeminal ganglion into the brainstem[11]
Assessment[edit | edit source]
As we know by now, the CN V has three terminal branches that innervate the skin of the face and neck, mucous membranes and paranasal sinuses of the face, the corneas, and the muscles of mastication, Therefore trigeminal reflex can be used to assess the proper functioning of the nerve for each of the area it serves. A trigeminal nerve reflex is a natural response to stimuli indicating the proper functioning of the nerve[17]. As it has both sensory and motor fibers, clinical assessment/examinations should evaluate the response of each structure. When the reflex is present, eg jaw reflex or corneal reflex, it is safe to say the CN V tract is functioning with in its normal natural parameters. However, the absence of or variation in the strength of the reflex assists in localizing the lesion and assessing the severity of the abnormality within the CN V tract[17].
Sensory Examinations -[edit | edit source]
The 2 main sensory sensations that are examined in relation to the CN V are pain and light touch. The method of choice for light touch testing is using a cotton wisp, where the examiner gives instructions to the patient to close their eyes and say "yes" each time they feel a touch. This test is first performed on areas NOT supplied by the CN V as it forms a baseline reference point, assuming that there are no sensory deficits in that area. Once the subject closes their eyes, the examiner proceeds to lightly touch the area supplied by the nerve with the cotton wisp. The nerve is always tested bilaterally to check for unilateral or bilateral (B/L) lesions.
For testing nociception, the same procedure is followed as above, but this time the testing object is a sharp object rather than a cotton wisp.
- Corneal reflex - involves B/L involuntary blinking of the eyelids stimulated by thermal, painful or tactile stimulation of the cornea. The absence of this reflex is indicative of TNr/Ophthalmic nerve or facial nerve damage as the ophthalmic nerve is the afferent limb and the facial nerve is the efferent limb. Peripheral damage causes ipsilateral reflex deficits, while central damage tends to be associated with bilateral deficits[17]. Other disorders and environmental factors affecting the cornea can also influence this reflex eg Glaucoma and diabetes.
- Jaw jerk reflex- performed to check the integrity of the upper motor neurons, which project into the trigeminal motor nucleus. The examiner places a finger in between the lower lip and the chin of the subject, with the mouth slightly open. The examiner then taps on the finger in a downward angle. Normally the reflex is slight or absent. However, in a upper motor neuron lesions the reflex is exaggerated as the masseter muscles jerk the mandible upwards.
- Lacrimal reflex - in this reflex arc, irritation of the cornea and conjunctiva leads to production of tears. The ciliary fibers of the nasociliary branch of V1 in the trigeminal nerve is the afferent limb of the reflex arc and the facial nerve (CN VII) and the superior salivary nucleus are CNS component of the reflex arc. In an event of an abnormal reflex arc, leads to watering of the eyes with out an appropriate stimulus.
Motor Examination -[edit | edit source]
It is performed to test the superficial muscles of mastication, mainly the temporalis and master muscles[17].
- Muscle mass - the subject is asked to clench their teeth, while the examiner palpates the temporalis and the masseter muscle to assess its muscle mass.
- Muscle strength - can be assessed by placing the fingers of the examining hand beneath the chin and asking the patient to open the mouth and resist closure.
- Motor nucleus function - the subject is asked to open their mouth and deviate the jaw from left to right. Unintentional jaw deviation toward one side pin points towards a lesion of the trigeminal nerve nuclei innervating the pterygoid muscle on the affected side[17].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Barral JP, Croibier A. Trigeminal nerve. In:Barral JP, Croibier A editor(s). Manual Therapy for the Cranial Nerves. Churchill Livingstone, 2009, Pages 107-114,
- ↑ 2.0 2.1 2.2 Pazhaniappan N. The Trigeminal Nerve (CN V). Available from:https://teachmeanatomy.info/head/cranial-nerves/trigeminal-nerve/. (accessed 14 October 2020)
- ↑ 3.0 3.1 Edvinsson, J.C.A., Viganò, A., Alekseeva, A. et al. The fifth cranial nerve in headaches. J Headache Pain 21, 65 (2020).
- ↑ 4.0 4.1 Shim YW, Paeng SH, Lee KS, Kim ST, Lee WH. Trigeminal Neuralgia Resulting from Delayed Cervical Cord Compression after Acute Traumatic Fracture of Odontoid Process. Korean J Neurotrauma. 2019;15(1):38-42
- ↑ Bogduk, N. The Anatomical Basis for Cervicogenic Headache. J Manipulative Physiol Ther. 1992;15: 67-70,
- ↑ Piovesan EJ, Kowacs PA, Oshinsky ML. Convergence of cervical and trigeminal sensory afferents. Curr Pain Headache Rep. 2003 Oct;7(5):377-83.
- ↑ Bartsch, T., Goadsby, P.J. The trigeminocervical complex and migraine: Current concepts and synthesis. Current Science Inc 7, 371–376 (2003).
- ↑ Busch V, Jakob W, Juergens T, Schulte-Mattler W, Kaube H, May A. Functional connectivity between trigeminal and occipital nerves revealed by occipital nerve blockade and nociceptive blink reflexes. Cephalalgia. 2006 Jan;26(1):50-5.
- ↑ Busch V, Jakob W, Juergens T, Schulte-Mattler W, Kaube H, May A. Occipital nerve blockade in chronic cluster headache patients and functional connectivity between trigeminal and occipital nerves. Cephalalgia. 2007 Nov;27(11):1206-14
- ↑ Jürgens TP, Busch V, Opatz O, Schulte-Mattler WJ, May A. Low-frequency short-time nociceptive stimulation of the greater occipital nerve does not modulate the trigeminal system. Cephalalgia. 2008 Aug;28(8):842-6.
- ↑ 11.0 11.1 11.2 11.3 Kamal H.A.M, Toland J. Trigeminal Nerve Anatomy: Illustrated Using Examples of Abnormalities. American Journal of Roentgenology. 2001;176: 247-251.
- ↑ Trigeminal Nerve Anatomy - Cranial Nerve 5 Course and Distribution. Available from: http://www.youtube.com/watch?v=KZl3zdUAd-w
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Huff T, Daly DT. Neuroanatomy, Cranial Nerve 5 (Trigeminal) [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
- ↑ Anatomy Dissected: Cranial Nerve V (trigeminal nerve). Available from: http://www.youtube.com/watch?v=psaGiXycPIo
- ↑ Gambeta E, Chichorro JG, Zamponi GW. Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Mol Pain. 2020;16:1744806920901890.
- ↑ Wallenberg syndrome , Lateral medullary syndrome - posterior inferior cerebellar artery syndrome. Available from: http://www.youtube.com/watch?v=p3qUpkGDDwE
- ↑ 17.0 17.1 17.2 17.3 17.4 Ogino MH, Tadi P. Neuroanatomy, Trigeminal Reflexes. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
- ↑ Cranial Nerve Examination: CN 5 Trigeminal nerve. Available from: http://www.youtube.com/watch?v=ACEhdCD_6rw