Triceps tendonitis
Introduction[edit | edit source]
Triceps tendon injuries are an uncommon clinical entity poorly described in the literature. Management of triceps tendinopathies depends on the mechanism of injury and the patient's motor examination.
- Triceps tendinopathies and partial tendon tears with intact strength can be managed conservatively with rest, ice, immobilization, nonsteroidal anti-inflammatory drugs, and physical therapy.
- If conservative management fails for 6 months or there are strength deficits on examination, surgery should be considered. Based on the current evidence, there are no clear guidelines for “best” surgical approach.[1]
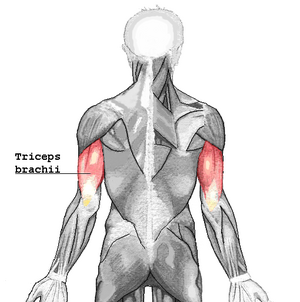
For anatomy see Triceps
Epidemiology/Etiology[edit | edit source]
- Triceps tears are more common in males than females.
- In sports triceps tendonopathies are more common in professional weight lifters[2], throwing athletes and soccer players[3] due to the constant of the elbow extension mechanism. Triceps tendonopathies also observed in sports that require quick triceps contraction such as off-road mountain biking, motorcycle riding and jumping[4].
- People with reduced strength or flexibility and simply lifting heavy objects increase the risk at tendonitis of the triceps. if not treated properly, the recovery process is lengthened.
- There are minimal reports of children with this condition.[1]
Pathophysiology[edit | edit source]
The pathophysiology of triceps tendinopathy is the same as the tendinopathies of other tendons. Repetitive use of the tendon leads to fibroblast proliferation. As a result, the fibroblasts release inflammatory and reparative mediators eg prostaglandin E2 (PGE2) which acts to degrade collagen in tendons as well as to decrease collagen synthesis. Substance P also is released by stretched tendon fibroblasts, which leads to fibrosis and pain. Both PGE2 and substance P contribute to tendon thickening, which is characteristic in tendinopathy[1]
- Tendonitits of the triceps occurs most often in the osteo-tendon joint of the tendon in the olecranon but also in the tendon itself or in the myotendinous joint.
- Risk factors that weaken the tendon include metabolic syndromes, endocrine disorders eg diabetes. Local factors that lead to weakening or injury of the tendon include the injection of corticosteroids, anabolic steroids and overtraining, leading to tendon disease or partial or complete rupture of the tendon.[5][6]
Clinical Representation[edit | edit source]
The main symptoms of triceps tendonitis are sensitivity and pain lengthwise of the tendon or sensitivity and localized pain in the insertion into the olecranon. The pain exacerbates with forced extension against resistance.[7] Patients describe pain and/or weakness in activities which require the elbow extension. It is also possible that there's swelling around the elbow. Distal triceps tendinitis is characterized by tenderness at the insertion of the triceps muscle, and pain is exacerbated with active or resisted elbow extension.
Triceps Tendinitis Associated Injuries / Differential Diagnosis[edit | edit source]
Differential diagnosis when evaluating a patient with a potential triceps tendon injury includes olecranon bursitis, posterior impingement syndrome, snapping triceps syndrome, ulnar collateral ligament injury, lateral collateral ligament injury, and, in pediatrics, medial epicondyle apophysitis and Panner disease. [1]
Diagnostic Procedures[edit | edit source]
Since triceps injuries are rare, there must be a high index of suspicion when evaluating these conditions. An X-ray should be obtained in all patients with elbow pain.[1]
Most of the times, diagnosis is delayed due to misdiagnosis. [8]A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose triceps tendonitis. Occasionally, further investigations such as an ultrasound, X-ray, CT scan or MRI scan may be required to assist with diagnosis and assess the severity of the condition.[9][10]
Outcome Measures[edit | edit source]
The dash questionnaire of disabilities of the arm, shoulder and hand.
Medical Management[edit | edit source]
In some cases, triceps tendonitis can be managed conservatively with activity modification, NSAIDs and occasionally resting splints.[11]
For complete triceps ruptures, surgery is the first-line treatment. There is currently no clear evidence to support one surgical technique as opposed to others. Postoperative rehabilitation is not well established, although recent data suggest 2 wk of immobilization with progressive return to full motion and strength exercises. Return to full activity is expected 3 months to 6 months postoperatively. The most significant surgical complication is rerupture, with a cited rerupture rate of 4.62%[1].
Physiotherapy Management[edit | edit source]
Physiotherapy management includes a period of immolization followed by ROM and then strengthening exercises.
Initial splint immobilization, with the elbow in 30 degrees of flexion, is continued for around 4 weeks. Following immobilization, gradual progression of elbow motion is allowed as tolerated, with the aim to achieve full ROM within 12 weeks.
The final stage is to introduce exercises to increase extension strength. Full extension strength can be achieved between 6 and 9 months.[12]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Casadei K, Kiel J, Freidl M. Triceps Tendon Injuries. Current sports medicine reports. 2020 Sep 1;19(9):367-72.Available: https://journals.lww.com/acsm-csmr/Fulltext/2020/09000/Triceps_Tendon_Injuries.9.aspx (accessed 31.12.2021)
- ↑ Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. Journal of Shoulder and Elbow Surgery. 1998 Mar 1;7(2):151-3.
- ↑ Sierra RJ, Weiss NG, Shrader MW, Steinmann SP. Acute triceps ruptures: case report and retrospective chart review. Journal of shoulder and elbow surgery. 2006 Jan 1;15(1):130-4.
- ↑ Jafarnia K, Gabel GT, Morrey BF. Triceps tendinitis. Operative Techniques in Sports Medicine. 2001 Oct 1;9(4):217-21.
- ↑ Taylor S, Hannafin J. Evaluation and Management of Elbow Tendinopathy. Sports Health: A Multidisciplinary Approach. 2012;4(5):384-393.
- ↑ Dunn JC, Kusnezov N, Fares A, Rubin S, Orr J, Friedman D, Kilcoyne K. Triceps tendon ruptures: a systematic review. Hand. 2017 Sep;12(5):431-8.
- ↑ Laratta J, Caldwell JM, Lombardi J, Levine W, Ahmad C. Evaluation of common elbow pathologies: a focus on physical examination. The Physician and Sportsmedicine. 2017 Apr 3;45(2):184-90.
- ↑ Lappen S, Geyer S, Scheiderer B, Macken C, Mazzocca AD, Imhoff AB, Siebenlist S. Distal triceps tendinopathies. Obere Extremität 2020:1-5.
- ↑ Tom JA, Kumar NS, Cerynik DL, Mashru R, Parrella MS. Diagnosis and treatment of triceps tendon injuries: a review of the literature. Clinical Journal of Sport Medicine. 2014 May 1;24(3):197-204.
- ↑ Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports Health. 2012 Sep;4(5):384-93.
- ↑ Donaldson O, Vannet N, Gosens T, Kulkarni R. Tendinopathies around the elbow part 2: medial elbow, distal biceps and triceps tendinopathies. Shoulder & Elbow. 2014 Jan;6(1):47-56.
- ↑ Demirhan M, Ersen A. Distal triceps ruptures. EFORT Open Reviews. 2016;1(6):255-259.