Trendelenburg Gait
Original Editor - Emma De Moerloose
Top Contributors - Uchechukwu Chukwuemeka, Scott Buxton, Glenn Demeyer, Kim Jackson, Redisha Jakibanjar, Shaimaa Eldib, Manisha Shrestha, Oyemi Sillo, Emma De Moerloose, Olivia Wayteck, Lauren Lopez, Admin, Carina Therese Magtibay, Daphne Jackson, Lenaertz Kiara, WikiSysop, Candace Goh and Claire Knott
Definition/ Description[edit | edit source]
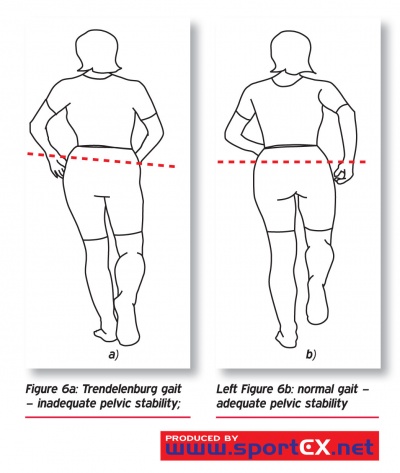
The trendelenburg gait is caused by weakness of the hip abductors, mostly the gluteal musculature. This condition makes it difficult to support the body’s weight on the affected side. In a normal gait situation, both legs bears half of the body weight. When the left leg is lifted, the right leg takes the entire weight. If a person walks, during the stance face of the gait, the pelvis tilts, rising on the side not taking weight. But at the pathologic situation when there is a abductor weakness as muscular dystrophies or in poliomyelitis, the pelvis drops instead of rising on the unsupported side.
In an attempt to lessen this effect, a child compensates by leaning over the affected hip. It means that the center of gravity is over the hip and so it reduces the degree of the pelvic drop.
[1] [2] [3][4][5]
See also: Trendelenburg Test
Clinically Relevant Anatomy[edit | edit source]
The hip joint is composed of acetabulum and the femur head. This structures are surrounded by soft tissues and twenty two active muscles. The muscles provides the stability and the forces for movement of the femur during activity. [6]
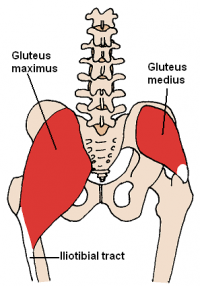
Trendelenbrug is described by a neuromuscular weakness of the hip abductors: the gluteus medius and gluteus minimus. The two muscles abduct the hip, they support the opposition of the pelvis and prevents the pelvis from dropping. The upward displacement of the greater trochanter shortens the fibers of the gluteus medius muscle. The fibers will be more horizontal instead vertical. [7][8]
| [9] | [10] |
In the above right video, Muscle Activation During Gait, concentric muscle contraction is indicated in yellow, isometric contraction in orange and eccentric contraction in purple.
Epidemiology/ Etiology[edit | edit source]
Trendelenburg gait occurs when the patient has to deal with weakness of the abductors of the hip (Musculus gluteus medius). [11] Patients who have significantly shorter height and greater body mass index sustained the Trendelenburg gait.[12] Level of evidence: B.
Trendelenbrug gait is caused by a neuromuscular weakness of the hip abductors or a hip disease.
By the neuromuscular weakness of the hip abductors caused by a damage or a neuronal injury of the superior gluteal nerve. Sometimes a pathologic condition affecting a proximal hip abductor muscles, most of the time the gluteus medius muscle.[13][14]
Trendelenburg gait is also observed in patients with developmental dysplasia of the hip, congenital cox vara, or cox valga secondary to another disorder in example: Legg-Calvé-Perthes desease or slipped capital femoral epiphysis. In those conditions, the abductor muscles are normal but they have a mechanical disadvantage. Patients with Slipped capital femoral emphysis also have muscular weakness that leads to trendelenburg gait.[15][16]
Trendelenburg gait is also seen after medical surgery. By patients with hip replacement, trendelenburg gait can be noticed. During the medical surgery of hip replacement, the gluteus medius muscle must be cut to expose the joint. It leads to a abductor dysfunction, trendelenburg. Level of evidence: 1B.[15]
Characteristics/Clinical Presentation[edit | edit source]
A trendelenburg gait, in which there is weakness of the hip abductors (gluteus medius muscle), is characterized by trunk shift over the affected hip and is best visualized from behind of in front of the patient. Observation of the patient’s gait from the side enables the examiner to detect stride and step length deficiendies as well as motion of the trunk and lower extremity in the sagittal plane, including the extensor or gluteus maximus lurch in which the patient thrusts the trunk posteriorly to compensate for weak hip extensors (gluteus maximus muscle). Observation from the side also enables detection of ankle dorsiflexor weakness and footdrop leading to inability of the foot to clear the ground, which is compensated for by excessive lower extremity flexion to facilitate foor clearande of the ground (steppage gait).[17]
Differential Diagnosis[edit | edit source]
Weak hip abductor muscles: no stabilizing effect of these muscles during stance fase. The patient exhibits an excessive lateral list in which the thorax is thrust laterally to keep the center of gravity over the stance leg.[18]
Bilateral weakness of the gluteus medius muscle: the gait shows accentuated side-to-side movement, resulting a wobbling gait or “chorus girl swing”.[19]
Some people compensate this by flexing their trunk over the weightbearing hip.[20]
This disturbance in the gait cycle is frequently observed in children with the development of congenital dislocation of the hip (CDH), dysplasia of the hip (DDH) and congenital coxa vara. Coxa vara can also occur from other disorders such as Legg-Calvé-Perthes disease or slipped capital femoral epiphysis (SCFE) - these are two of the most common causes of hip pain or limp.[21] [22] [23] The Trendelenburg gait can also occur as the result of a neuronal injury. A lesion of the superior gluteal nerve (SGN), which is the main nerve stimulating the hip abductors, can lead to weakness.[24] [25] This nerve also supplies the gluteus medius, gluteus minimus and tensor fascia lata muscles.[26] Other conditions in which a Trendelenberg gait may be observed include muscular dystrophy and hemiplegic cerebral palsy.[27]
Diagnostic Procedures[edit | edit source]
The Trendelenburg test determines the integrity of hip abductor muscle function. The therapist can use this test when there is no X-ray taken but there are signs of Trendelenburg. The person has to stand on one leg and tilt the other one up. The test is negative when the hip of the leg that is pulled up, will also go up. There is no sign for trendelenburg. When the hip from the leg is pulled up will become lower then the other one, we talk about a positive sign for the trendelenburg test. These persons may have trendelenburg, to be absolutely sure, these persons have to take an X-ray to confirm the trendelenburg pathology.[28]
When pain in the hip is diagnosed, the surgeon will base the diagnose on data obtained vrom clinical and X-ray assessments. These two data sources will provide an answer to:
- The level of the proximal osteotomy
- The amount of valgus, extension and derotation at the proximal osteotomy
- The level of the distal osteotomy
- The amount of varus and lengthening at the distal osteotomy.[29] [30] [31] Level of evidence: B
Outcome Measures[edit | edit source]
Examination[edit | edit source]
The modified McKay criteria is useful to assess if a patient has Trendelenburg gait. These criteria measure pain symptoms, gait pattern, Trendelenburg sign status, and the range of hip joint movement. Level of evidence: A2
| Grade | Criteria |
| Excellent | Stable, painless hip; no limp; negative Trendelenburg sign; full range of movement |
| Good | Stable, painless hip; slight limp; slight decrease in range of movement |
| Fair | Stable, painless hip; limp; positive Trendelenburg sign; and limited range of movement, or a combination of these |
| Poor | Unstable or painful hip or both; positive Trendelenburg sign |
Medical Management[edit | edit source]
While no treatment modalities currently exist for patients with compensated Trendelenburg gait, medical management can attempt to deal with the causes underlying a Trendelenburg gait. Open reduction and Salter innominate osteotomy (SIO) without preoperative traction is effective in the management of development dysplasia of the hip in children younger than 6 years. [32] Level of evidence: A2
Pelvic support osteotomies cause a significant improvement in outcomes relating to posture, gait and walking tolerance in patients who had untreated congenital dislocations.[33] [34] Level of evidence: B
Osteopathic Manipulative Treatment (OMT) could result in improved gait parameters for individuals with somatic dysfunctions, as measured by a GaitMat II system. Further research is needed to better understand the relationship between somatic dysfunctions and gait deviations. [35] Level of evidence: C
There is a significant difference in the incidence of a positive Trendelenburg gait between surgical approaches, using trochanteric osteotomy or not. This shows the effectiveness of distal trochanteric transfer.[36] Level of evidence: A2
Physical Therapy Management[edit | edit source]
Trendelenburg gait can result in the development of other pathologies of the bones in the hip and knee such as arthritis or premature wear in the hip joints. Therefore it is of great importance to find out a form of physical therapy that will cause a reduction in the degree of Trendelenburg gait to minimize the secondary injuries. [37] (LoE: 5) [38] (LoE: 2b)
Trendelenburg gait is an abnormal gait caused by weakness of the hip abductors. Therefore, the main purpose of physical therapy with regards to this impairment is to strengthen the abductors of the hip. An appropriate exercise to strengthen the hip abductors is to have the patient lay side-lying on the less affected side and abduct the upper leg towards the ceiling. To make the exercise more challenging, a weight or theraband can be placed around the active limb. Other exercises in the revalidation of Trendelenburg gait include functional closed-chain exercises, lateral step-ups and functional balance exercises. It is also important to strengthen the rest of the leg on the affected side. Level of evidence: D.
Research has shown the importance of strengthening the muscles. Not only the M. gluteus medius, but also the quadriceps and the hamstrings. These increases in strength of the muscles, results in a reduction of the degree of Trendelenburg gait.
The use of an Electromyogram (EMG) reduces the Trendelenburg gait by an average of 29 degrees. The average stride length has been shown to increase from 0,32 ± 0,3m to 0,45 ± 0,2m and the speed of gait has been shown to increase from 1,6 ± 0,4 kmh−1 to 3,1 ± 0,5 kmh−1. [39] (LoE: 4).
During the treatment, EMG biofeedback has been used. As weakness of the gluteus medius muscles is the prime contributor to Trendelenburg gait, the device provides warning tones giving feedback of improper gait through too little gluteus medius activity.
In every day life the therapist isn’t constantly with the patient. So, when the patient walks incorrectly, trunk shift over the affected hip, during the day, the positive effects of the therapy can be reversed.
With this in mind, researchers investigated the usefulness of a two-channel EMG biofeedback training device that patients could wear at home. The conclusion of this study was that the group that used the home training device, showed almost normal gait after two months. This goal is only achievable when patients are doing exercises which strengthen the hip abductors in combination with the two-channel EMG biofeedback device.[38] (LoE: 2b) [40] (LoE: 4) [41] (LoE: 5)
Patients with trendelenburg suffer from abnormal range of motion in hip and trunk. The purpose of the treatment is to increase the range of motion. The people get visual feedback about how the walk. They get advises from the therapists so they will think about you must walk correctly. This kind of treatment is good for increasing the range of motion of the hip and the trunk.[42] (LoE: 4)
Key Research[edit | edit source]
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Hensinger RN: Limp. Pediatr Clin North Am 1986; 33:1355.
- ↑ Pomeroy VM, Chambers SH, Giakas G, Bland M. Reliability of measurement of tempo-spatial parameters of gait after stroke using GaitMat II. Clin Rehabil. 2004;18(2):222-227.
- ↑ Vasudevan P.N., et al. Can trendelenburg's sign be positive if the hip is normal. R.V. Institute of research Ilizarov Technology, Kerala, India. 2BfckLRCAN TRENDELENBURG’S SIGN BE POSITIVE IF THE HIP IS NORMAL ,P. N. VASUDEVAN, K. V. VAIDYALINGAM, P. BHASKARAN NAIR, From the R. V. Institute of Research in Ilizarov Technology, Kerala, India. 2B
- ↑ Apley G. Apley’s system of orthopaedics and fractures. 6th edition, ELBS, 1986:243.
- ↑ Castro, W. H. (sd). Examination and diagnosis of musculoskeletal disorders. Thieme.
- ↑ Poitout, D. G. (2004). Biomechanics and Biomaterials in orthopedics. Springer. P 528- 530
- ↑ McGee, S. R. (2007). Evidence- based physical diagnosis . Elsevier. p51
- ↑ Pai VS, Significance of the Trendelenburg test in total hip arthroplasty, J Arthroplasty, 1996; 11 (2): 174-179 1B
- ↑ Roda D. The gait cycle: a breakdown of each component. Available from: http://www.youtube.com/watch?v=5j4YRHf6Iyo [last accessed 2013/11/24]
- ↑ Oberhofer K. Muscle activation during gait. Available from: http://www.youtube.com/watch?v=GV6CAZiv5Zo [last accessed 2013/11/24]
- ↑ Hensinger RN: Limp. Pediatr Clin North Am 1986; 33:1355.
- ↑ Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg [Br] 1982;64:17-9.
- ↑ European Journal of Applied Physiology * September 2001, Volume 85, Issue 5, pp 491-495 * The use of electromyogram biofeedback to reduce Trendelenburg gait *Jerrold Petrofsky
- ↑ McGee, S. R. (2007), Evidence- based physical diagnosis, Elsevier, p51-54
- ↑ 15.0 15.1 Tachdjan's. (sd). Pediatric orthopeadics. Elsevier. P79,p80,p95
- ↑ Use of Osteopathic Manipulative Treatment to Manage Compensated Trendelenburg Gait Caused by Sacroiliac Somatic Dysfunction ,Adam C. Gilliss, DO; Randel L. Swanson II, OMS III; Deanna Janora, MD; Venkat Venkataraman, PhDfckLRThe journal of of the americal osteopathic association , 3B
- ↑ Richard J. Ham, et. Al, Primary care geriatrics: a case-based approach, Mosby Elsevier, 2007.
- ↑ David J. Magee, Orthopedic physical assessment, Musculoskeletal rehabilitation series, fifth edition, 2006.
- ↑ J. Gross, J. Fetto, Elaine Rosen, Musculoskeletal Examination, 3rd Edition.
- ↑ McGee S., Evidence based physical diagnosis, 3rd edition, 2012.
- ↑ Hensinger RN: Limp. Pediatr Clin North Am 1986; 33:1355.
- ↑ Kelsey JL. Epidemiology of slipped capital femoral epiphysis: a review of the literature. Pediatrics 1973.
- ↑ Yochum TR, Rowe LI. Essentials of skeletal radiology. Baltimore: Williams and Wilkins, 1987; 465-68.; 51: 1042-50.
- ↑ Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg [Br] 1982;64:17-9.
- ↑ Jacobs LG, Buxton RA. The course of the superior gluteal nerve in the lateral approach to the hip. J Bone Joint Surg [Am] 1989;71:1239-43.
- ↑ Bülbül M, Ayanoğlu S, Öztürk K, İmren Y, Esenyel C, Yeşiltepe R, et al. How reliable is the safe zone of Hardinge approach for superior gluteal nerve? Trakya Univ Tıp Fak Derg 2009;26:134-6.
- ↑ Flynn JM, Widmann RF. The limping child: evaluation and diagnosis. J Am Acad Orthop Surg 2001;9:89-98.
- ↑ P. HardCastle, S. Nade, The significance of the trendelenburg test, J Bone Joint Surg Br November 1985 vol. 67-B no. 5 741-746.
- ↑ Saleh M, Milne A (1994) Weight-bearing parallel-beam scanography for the measurement of leg length and joint alignment. J Bone Joint Surg Br 76(1):156–157.
- ↑ Paley D (2002) Normal lower limb alignment and joint orientation. In: Paley D (ed) Principles of deformity correction. Springer, Berlin, pp 1–18.
- ↑ Gage JR (1991) Gait analysis in cerebral palsy, 1st edn. Clinics in developmental medicine, vol 121. Mac Keith Press, London.
- ↑ Bohm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg Am 2002;84:178–86.
- ↑ Lance PM (1936) Osteotomies sous-trochanterienne dans le traitement des luxations congenitales inveterees de la hanche. Masson Cie, Paris.
- ↑ Milch H (1941) The ‘pelvic support’ osteotomy. J Bone Joint Surg Am 23(3):581–595.
- ↑ Rosano C, Brach J, Longstreth Jr WT, Newman AB. Quantitative measures of gait characteristics indicate prevalence of underlying subclinical structural brain abnormalities in high-functioning older adults [published online ahead of print October 25, 2005]. Neuroepidemiology. 2006;26:52-60.
- ↑ Fernandez DL, Isler B, Müller ME. Chiari’s osteotomy: a note on technique. Clin Orthop 1984;185:53-8.
- ↑ Andrews J., Harrelson G.,Wilk K., Physical rehabilitation of the injured athlete, Elsevier Saunders, 2012, 4th edition (LoE: 5)
- ↑ 38.0 38.1 European Journal of Applied Physiology * September 2001, Volume 85, Issue 5, pp 491-495 * The use of electromyogram biofeedback to reduce Trendelenburg gait *Jerrold PetrofskyfckLRhttp://link.springer.com/article/10.1007/s004210100466 (LoE: 2b)
- ↑ J. S. Petrofsky. Microprocessor-based gait analysis system to retrain Trendelenburg gait. Medical and Biological Engineering and Computing , Volume 39, Number 1, 140-143, DOI: 10.1007/BF02345278. (LoE: 4)
- ↑ J. S. Petrofsky. Microprocessor-based gait analysis system to retrain Trendelenburg gait. Medical and Biological Engineering and Computing , Volume 39, Number 1, 140-143, DOI: 10.1007/BF02345278. (LoE: 4)
- ↑ Davis C.M., Complementary therapies in rehabilitation, SLACK incorporated, 2009, 3th edition (LoE: 5)
- ↑ D. Hamacher, D. Bertram, C. Fölsch, L. Schega, Evaluatiob of a visual feedback system in gait retraining: A pilot study, Elsevier, 2012. Level of evidence: 4