Overview of Traumatic Brain Injury
Original Editor - Wendy Walker
Lead Editors - Wendy Walker, Naomi O'Reilly, Kim Jackson, Rachael Lowe, Vidya Acharya, Lucinda hampton, Kalyani Yajnanarayan, Stacy Schiurring, George Prudden, Uchechukwu Chukwuemeka, Shaimaa Eldib, Nicole Hills, Lauren Lopez, Mande Jooste, 127.0.0.1, Tony Lowe, Nupur Smit Shah, WikiSysop, Simisola Ajeyalemi and Karen Wilson
Definition[edit | edit source]
Traumatic Brain Injury [TBI}, also known as Head Injury and Acquired Brain Injury [ABI], is defined as injury to the brain which occurred as a result of trauma, and is non-progressive.
It occurs when an external force impacts the brain, & often is caused by a blow, bump, jolt or penetrating wound to the head.
However, not all blows or jolts to the head cause TBI: some just cause bony damage to the skull but do not cause brain injury.
Causes of TBI[edit | edit source]
The 2 most common causes of TBI are:
- Falls
- Road Traffic Accident [RTA] This includes vehicle collisions, pedestrians being hit by a vehicle, vehicle-cyclist and car-motorcyclist collisions as well as bicycle and motorbike crashes which do not involve another vehicle.
Until recently, RTA was the primary cause of brain injury, but an international study published in 2013 reported that "falls have now surpassed road traffic incidents as the leading cause of this injury"[1].
Incidence of TBI[edit | edit source]
One study found that TBI was "a major cause of death and disability on the United States, contributing to about 30% of all injury deaths[2]".
A 2010 study looked at data from several nations, and reported that:"each year 235 000 Americans are hospitalized for non-fatal TBI, 1.1 million are treated in emergency departments, and 50 000 die. The northern Finland birth cohort found that 3.8% of the population had experienced at least 1 hospitalization due to TBI by 35 years of age. The Christchurch New Zealand birth cohort found that by 25 years of age 31.6% of the population had experienced at least 1 TBI, requiring medical attention (hospitalization, emergency department, or physician office). An estimated 43.3% of Americans have residual disability 1 year after injury. The most recent estimate of the prevalence of US civilian residents living with disability following hospitalization with TBI is 3.2 million."[3]
Mechanism of Injury[edit | edit source]
Closed head injury[edit | edit source]
Often occurs as a result of RTA, or a blow to the head, or a fall where the head strikes the floor or another hard surface..
In closed head injury, the skull is not penetrated, but it is frequently fractured.
Generally there is both focal and diffuse axonal damage.
Open head injury[edit | edit source]
This is caused by a penetrating wound, eg. by a weapon or from a bullet.
In these cases the skull is penetrated.
The brain injury is usually largely focal axonal damage.
Deceleration injury[edit | edit source]
This frequently occurs in RTA, when rapid deceleration occurs as the skull meets a stationary object, causing the brain to move inside the skull.
Mechanical brain injury occurs due to axonal shearing, contusion and brain oedema.
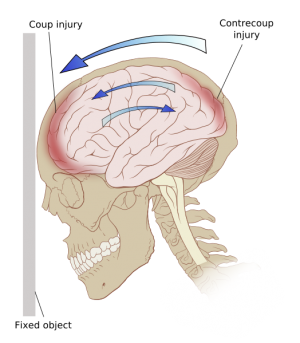
Coup-contracoup injury[edit | edit source]
Coup injury[edit | edit source]
This occurs beneath the point of impact - may be associated with a skull fracture at the site of impact
Contracoup injury[edit | edit source]
This occurs when the impact is sufficient to cause the brain to move within the skull; the brain moves in the opposite direction, and hits the opposite side of the skull, causing bruising.
Coup-contracoup injury[edit | edit source]
This is a frequent occurence - opposite poles of the brain suffer injury.
See illustration at the top of this page.
Pathological Process[edit | edit source]
Mechanical Damage[edit | edit source]
AKA Primary Damage andPrimary Insult. Primary mechanical brain injury is the direct injury to the brain cells caused by the initial impact.
The mechanical forces can cause intracranial haematoma [ defined as "a localised swelling that is filled with blood caused by a brea in the wall of a blood vessel"] and/or vascular injury, as well as injury to cranial nerves.
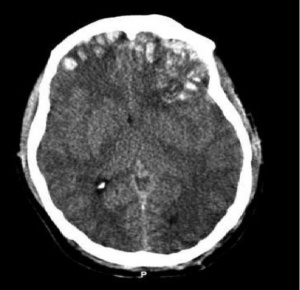
Intracranial haematomas are categorised in the following way:
- Epidural haematomas
- Subdural haematomas
- Subarachnoid haematomas
In the CT scan image shown here, skull fractures are visible, as well as multiple frontal, parietal and emporal lobe contusions with a subdural haematoma on the left isde as well as associated interhemispheric haemorrhages.
Delayed non-mechanical Damage[edit | edit source]
AKA Secondary Damage. Non-mechanical brain injury is caused by ischaemic[4], cytotoxic and inflammatory processes.
One of the most significant factors is the excessive release of glutamate and aspartate, which alter cell wall permeability which ultimately leads to destruction of axons[5].
Clinical Presentation[edit | edit source]
The presentation depends on the areas of the brain which have been damaged.
One of the early signs of TBI, often developing a week after the head injury, is the onset of spasticity.
Spasticity symptoms include hypertonicity and spasm of the affected muscles and an increase in deep tendon reflexes; it's severity can range from mild stiffness of the muscles to severe (and painful) muscle spasms.
Classifiation of TBI[edit | edit source]
There are 3 ways of classifying head injury:
- Patho-anatomic ie. what damage has occurred where in the brain, for instance, subdural haemorrhage
- Injury severity, typically using the Glasgow Coma Scale [GCS] as the measure, where a score of 8 or less is defined as Severe TBI
- Physical mechanism causing the injury, categorised as contact or "impact" loading when the head is struck or strikes an object, as oppsed to noncontact or "inertial" loading (which is when the brain moves within the skull.
Signs & Symptoms[edit | edit source]
- Loss of consciousness:
In Moderate brain injury, loss of consciousness [LOC] ranges from 30 minues to 6 hours, and gnerally the patient will have a GCS score between 9 and 12.
In Severe brain injury, loss of consciousness occurs for more than 6 hours and the GCS score is 8 or lower.
- Cognitive issues:
these may include problems with concentration, attention, memory, speed of processing, language comprehension, confusion, impulsive behaviour
- Speech and language issues:
receptive aphasia (ie. not understanding the spoken word), expressive aphasia (difficulty with/inability to talk), slurred speech
- Vision:
blindness or partial blindness, blurred vision, double vision (diplopia), photophobia, light sensitivity
- Hearing:
Deafness, or reduction in hearing, tinnitus (ringing in the ears), increased sensitivity to sounds (hyperacusis, phonophobia)
- Smell and taste:
Reduced or loss of sense of smell and/or taste, reduced appetite
- Emotional and Social
Irritability, aggression, depression, apathy, disinhibition, lack of insight, reduced motivation, mood swings
Diagnostic Procedures[edit | edit source]
Magnetic Resonance Imaging (MRI) and Computerised Tomography (CT) scanning are frequently used in order to image the brain.
CT scanning is indicated in the very early stages post injury, as it shows fractures and can detail haemorrhages and haematomas in the brain, as well as contusions and swelling.
MRI is often used once the patient is medically stable to give a more detailed view of the brain tissue.
Management / Interventions[edit | edit source]
Surgical Interventions[edit | edit source]
Emergency surgery is often required to minimise brain damage:
- surgery to remove haematoma and thus reduce pressure on brain tissue
- removal of part of the skull in order to relieve pressure
- surgical repair of severe skull fractures, and/or removal of skull fragments from brain tissue
Medical Interventions[edit | edit source]
Medication may be used to limit secondary damage to the brain:
- Coma-inducing medication may be given, as a brain in coma requires far less oxygen so if there is reduced oxygen and nutrient supply due to blood vessels being compressed by increased pressure, being in coma is therapeutic
- Diuretics (given intravenously) can be used to reduce the amount of fluid in soft tissues and thus help reduce pressure in the brain
- Anti-epileptic medication is often given in the early stages in orer to avoid any additional brain damage which might be caused if a seizure were to occur.
Resources[edit | edit source]
BrainLine is an American multimedia website providing information and resources about treating and living with TBI; it includes a series of webcasts, written online resources and an electronic newsletter. It has a version in Spanish too.
Headway is a UK charity for TBI which has a comprehensive website, with information on the different aspects of TBI and its rehabilitation. It has a number of useful written resources for patients on the website, including ones on Brain injury and Epilepsy, Loss of taste and smell after Brain injuryand Balance problems and Dizziness after Brain injury
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Changing patterns in the epidemiology of traumatic brain injuryfckLRBob Roozenbeek, Andrew I. R. Maas & David K. Menon Nature Reviews Neurology 9, 231-236 (April 2013)
- ↑ Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Faul M, Xu L, Wald MM, Coronado VG. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010
- ↑ The Epidemiology of Traumatic Brain InjuryfckLRCorrigan, John D. PhD, ABPP; Selassie, Anbesaw W. DrPH; Orman, Jean A. (Langlois) ScD, MPH The Epidemiology of Traumatic Brain Injury March/April 2010 - Volume 25 - Issue 2
- ↑ Ischaemic brain damage in fatal non-missile head injuries. Graham DI, Adams JH, Doyle D. J Neurol Sci. 1978, 39 (2–3): 213-34
- ↑ Axonal Damage in Traumatic Brain Injury. Smith DH, Meaney DF. The Neuroscientist. 2000, 6: 483-495