Thermotherapy
Original Editor - Kirianne Vander Velden
Lead Editors - Bianca Geeroms, Anja Vanroelen, Charles Senay, Robert Wright, Kirianne Vander Velden, Admin, Kim Jackson, Daiton Wells, Ella Rubbens, Oyemi Sillo, WikiSysop, Tony Varela, 127.0.0.1, Hau Nguyen, Claire Knott, Chelsea Mclene, Aminat Abolade, Laura Ritchie, Evan Thomas and Scott Buxton
Definition/Description [edit | edit source]
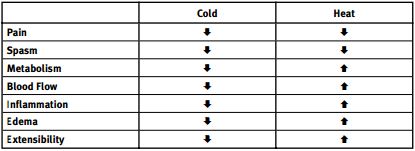
Thermotherapy consists of application of heat or cold (cryotherapie) for the purpose of changing the cutaneous, intra-articular and core temperature of soft tissue with the intention of improving the symptoms of certain conditions. Cryotherapy and thermotherapy are useful adjuncts for the treatment of musculoskeletal injuries and soft tissue injuries. Using ice or heat as a therapeutic intervention decreases pain in joint and muscle as well as soft tissues and they have opposite effects on tissue metabolism, blood flow, inflammation, edema and connective tissue extensibility. Thermotherapy can be used in rehabilitation facilities or at home. [1] [2] [3] [4]
Purpose[edit | edit source]
The goal of thermotherapy is to alter tissue temperature in a targeted region over time for the purpose of inducing a desired biological response. The majority of thermotherapies are designed to deliver the thermal therapy to a target tissue volume with minimal impact on intervening or surrounding tissues.
- Heat: By increasing the temperature of the skin/soft tissue, the blood flow increases by vasodilatation. The metabolic rate and the tissue extensibility will also increase. Heat increases oxygen uptake and accelerates tissue healing, it also increases the activity of destructive enzymes, such as collagenase, and increases the catabolic rate.
- Cold: By decreasing the temperature of the skin/soft tissue, the blood flow decreases by vasoconstriction. It will be followed afterwards by a vasodilatation which will prevent against hypoxic damage (hunting reflex: If the cold pack is left on the skin for more than 10 minutes, the blood vessels will dilatate). The tissue metabolism will decrease just like the neuronal excitability, inflammation, conduction rate and tissue extensibility. At joint temperatures of 30°C or lower, the activity of cartilagedegrading enzymes, including collagenase, elastase, hyaluronidase, and protease, is inhibited. the decreased metabolic rate limits further injury and aids the tissue in surviving the cellular hypoxia that occurs after injury.
Figure 1:Pathophysiologic effects of topical modalities [4]
Both applications can reduce the pain, but when we need to use which application is still the question. Therefore, patient’s preference can be taken into consideration when deciding which thermotherapy tool to use. [1] [5] [6] [7]
Application[edit | edit source]
- Heat: Heating of superficial tissues can be achieved using hot packs, wax baths, towels, sunlight, saunas, heat wraps, steam baths/rooms. We can also get the heat in the deeper tissues through electrotherapy (ultrasound, shockwave and infrared radiation).
- Cold: Cooling is achieved using ice packs, ice baths, cooling gel packs, cold air and sprays. [1] [2]
In the literature, they describe cryotherapie (ice application) as an effective treatment for soft tissue injuries. [8] [9] [4] It reduces the swelling, and it will improve the range of motion. However, there are still some doubts if it is actually effective for pain relief. So the application of ice may be useful for a variety of musculoskeletal pains, yet the evidence for its efficacy should be established more convincingly. [10] [11]
Exercise in warm water, usually called hydrotherapy or balneotherapy, is a popular and effective treatment[12] with a pain relief effect for many patients with painful neurologic or musculoskeletal conditions. The warmth of water may block nociception by acting on thermal receptors and mechanoreceptors, thus influencing spinal segmental mechanisms. It gives positive effects on cutaneous barrier homeostasis and a anti-inflammatory activity. In addition, the warmth may enhance blood flow and muscle relaxation. The hydrostatic effect may also relieve pain by reducing peripheral edema and by dampening sympathetic nervous system activity. [13] [14][ [12]
Mechanism of Action[edit | edit source]
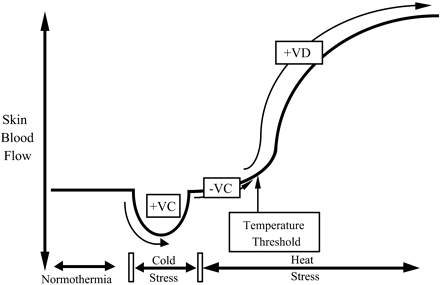
Skin blood flow is controlled by two branches of the sympathetic nervous system: a noradrenergic vasoconstrictor system and a cholinergic active vasodilator system. These dual sympathetic neural control mechanisms affect the major aspects of thermoregulatory responses over most of the human body’s surface.
Figure 2:Skin blood flow responses to cold stress and heat stress. [5]
VC = vasocondtriction, VD = vasodilatation
During periods of hypothermia, falling core and skin temperatures lead to reflexive increases in sympathetic active vasoconstrictor nerve activity to reduce skin blood flow and conserve body heat. During periods of heat stress, increasing core and skin temperatures lead to reflexive increases in sympathetic active vasodilator nerve activity to increase skin blood flow.
The effect of heat on pain is mediated by heat sensitive calcium channels. These channels respond to heat by increasing intracellular calcium. This generates action potentials that increases stimulation of sensory nerves and causes the feeling of heat in the brain. These channels are part of a family of receptors called TRPV receptors. TRPV1 and TRPV2 channels are sensitive to noxious heat, while TRPV4 channels are sensitive to normal physiological heat. Their multiple binding sites allow a number of factors to activate these channels. Once activated, they can also inhibit the activity of purine pain receptors. These receptors, called P2X2 and P2Y2 receptors, are mediated pain receptors and are located in the peripheral small nerve endings. For example, with peripheral pain, heat can directly inhibit pain. However, when pain is originating from deep tissue, heat stimulates peripheral pain receptors which can alter what has been termed gating in the spinal cord and reduce deep pain.
Previous studies have suggested that temperature can affect the exchange between Ca2+ and Na+ in neural cells. They have documented an increase in both pain threshold (PTH) and pain tolerance (PTO) with the use of cooling. [15] [11] [5] [3]
True or not true?Disadvantage: when you heat skin, vasodilatation (VD) distracts blood from soft tissue underneath and poor muscle circulation decreases metabolism in the muscles…
Increased superficial tissue temperature results in the release of chemical mediators, such as histamine and prostaglandins, which result in vasodilation. These vasodilatory mechanisms do not significantly affect blood flow in skeletal muscle since skeletal muscle blood flow is heavily influenced by other physiologic and metabolic factors. Exercise is the best means to increase blood flow to skeletal muscle. [16] [7]
Treatment[edit | edit source]
The treatment depends on the type of application and the type of disease.
There are 3 phases of the healing process: the inflammatory phase, the proliferation phase and the remodeling phase. [17] [18]
- The first phase, known as the inflammatory phase, protects the injured area from further injury while the body contains the damaged tissue. During this phase, cryotherapy can help to reduce swelling. Never use heat during this phase because heat increases the blood flow into the injured area and increases the amount of swelling. The inflammatory phase has a duration of 2 days.
- During the second phase, the proliferation phase, new tissue and scar tissue are formed. Heat can now be applied to the injured area to facilitate the healing process.
- The third and final phase, the remodeling phase, is the process of returning to health: the restoration of structure and function of injured or diseased tissues. The healing process includes blood clotting, tissue mending, scarring and bone healing. Heat therapy can also be used during this phase. [17] [18]
Physiological Effects[edit | edit source]
Many of the local physiologic effects of heat and cold have been studied thoroughly. For instance, heat increases skin and joint temperature, improves blood circulation and muscle relaxation and decreases joint stiffness. Cold will numb the pain, decrease swelling, constrict blood vessels and block nerve impulses to the joint. [17] [19] [2]
Deep heating is thought to lessen nerve sensitivity, increase blood flow, increase tissue metabolism, decrease muscle spindle sensitivity to stretch, cause muscle relaxation, and increase flexibility. Heat stimulates the cutaneous thermo receptors that are connected to the cutaneous blood vessels, causing the release of bradykinin which relaxes the smooth muscle walls resulting in vasodilation. Muscle relaxation occurs as a result of a decreased firing rate of the gamma efferents, thus lowering the threshold of the muscle spindles and increasing afferent activity. There is also a decrease in firing of the alpha motorneuron to the extrafusal muscle fibre, resulting in muscle relaxation and decrease in muscle tone. [20] [21]
Precautions[edit | edit source]
A very important note that needs to be made is that thermotherapy is safe for people with a normal skin sensation. When a patient has problems with thermal sensitivity, it could be dangerous. They cannot feel if they are being burned due to the application. [1] [22]
Effectiveness[edit | edit source]
There are still a lot of contradictions if the use of thermotherapy is effective; however, worldwide it is used to reduce the pain.
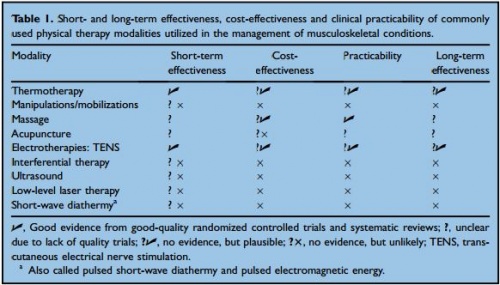
While there is good evidence that exercise relieves pain, improves function, and is cost-effective, evidence supporting the use of non-exercise physiotherapeutic interventions is much weaker. There is some support for the efficacy of thermotherapy, transcutaneous electrical neuromuscular stimulation (TENS), and massage. But there is little evidence to support the efficacy of electrotherapy, acupuncture or manual therapy.
For knee osteoarthritis (OA), ice massage is reported to improve joint movement, pain and function; ice packs can reduce swelling and improve movement but may not relieve pain. In rheumatoid arthritis (RA), heat or cold packs are reported to have no effect on edema, pain, movement, strength or function.
Cost effectiveness [1] [19] [22]
Despite conflicting evidence, the simple form of thermotherapy is widely recommended for many musculoskeletal conditions because it is a safe, effective, easy-to-apply and well-liked therapy based on anecdotal reports, expert opinion and patient preferences. Interventions that can be self-administered (thermotherapy, TENS, massage) are more likely to be cost-effective and less burdensome and hence much more attractive long-term management options. Complex thermal therapeutic modalities (heating deeper tissues) require special equipment, supervision and need to be delivered by a therapist, making them less accessible, more costly and higher risk.
Figure 3:Short- and long-term effectiveness, cost-effectiveness and clinical practicability of commonly '
used physical therapy modalities utilized in the management of musculoskeletal conditions. [1]
level of evidence: 1C
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 M. V. Hurley et al., Non-exercise physical therapies for musculoskeletal conditions, Best Practice & Research, Clinical Rheumatology, 2008. 1C
- ↑ 2.0 2.1 2.2 Brosseau L., Yonge K.A., Welch V. et al., Thermotherapy for treatment of osteoarthritis, the Cochrane library, 2003. 1A
- ↑ 3.0 3.1 Petrofsky J., Berk L., Lee H., Moist heat or dry heat delayed onset muscle soreness, Journal of clinical medicine research, 2013. 2B
- ↑ 4.0 4.1 4.2 Scott F. Nadler, DO, FACSM, Kurt Weingand, PhD, DVM, and Roger J. Kruse, MD; The Physiologic Basis and Clinical Applications of Cryotherapy and Thermotherapy for the Pain Practitioner, pain physician, 2004. 1A
- ↑ 5.0 5.1 5.2 D. L. Kellogg Jr., In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges, the American Physiological Society, 2006. 3A
- ↑ Hendee W.R., Physics of Thermal Therapy, Fundamentals and Clinical applications, By Taylor and Francis group, 2013.
- ↑ 7.0 7.1 Heinrichs K., Textbook of medical physiology, Philadelphia, 1986. (chapter 16: superficial thermal modalities).
- ↑ Bleakley C.,McDonough S.,MacAuley D., The Use of Ice in the Treatment of Acute Soft-Tissue Injury: A Systematic Review of Randomized Controlled Trials, The American Journal of Sports Medicine; 2004. 1A
- ↑ Tricia J. Hubbard et al., Does Cryotherapy Improve Outcomes With Soft Tissue Injury? Journal of Athletic Training, 2004. 1A
- ↑ Ernst E., Fialka V., Ice freezes pain? A review of the clinical effectiveness of analgesic cold therapy, J pain symptoms manage, 1994. 5
- ↑ 11.0 11.1 Amin A. Algafly, Keith P. George, The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance, Br J Sports Med, 2007. 3B
- ↑ 12.0 12.1 Choi YJ et al. Therapeutic effects and immunomodulation of suanbo mineral water therapy in a murine model atopic dermatitis. 1B
- ↑ Hiroharu K., Kiichiro T., Effectiveness of Aquatic Exercise and Balneotherapy: A Summary of Systematic Reviews Based on Randomized Controlled Trials of Water Immersion Therapies, Journal of epidemiology, 2010. 1A
- ↑ Eversden L, Maggs F, Nightingale P, Jobanputra P., A pragmatic randomized controlled trial of hydrotherapy and land exercises on overall well-being and quality of life in rheumatoid arthritis, BMC Musculoskeletal Disorders, 2007. 2A
- ↑ Lacy A. Holowatz et al., Mechanisms of acetylcholine-mediated vasodilatation in young and aged human skin, The Physiological Society, 2005. 3B
- ↑ Swenson C et al. Cryotherapy in sports medicine. Scand J Med Sci Sports. 1996 Aug6(4) 1B
- ↑ 17.0 17.1 17.2 Kathleen A. Sluka, PhD, PT, Michelle R. Christy, MPT, Wendy L. Peterson, MPT, Staci L. Rudd, MPT, Stacie M. Troy, MPT, Reduction of pain-related behaviors with either cold or heat treatment in an animal model of acute arthritis, Archives of Physical Medicine and Rehabilitation, March 1999. 3B
- ↑ 18.0 18.1 Fahey T.D., Athletic training: principles and practice, Mayfield.
- ↑ 19.0 19.1 19.2 Oosterveld F.G.J., Rasker J.J., Effects of local heat and cold treatment on surface and articular temperature of arthritic knees, American college of rheumatology, 1994. 1B
- ↑ William E. Prentice, An Electromyographic Analysis of the Effectiveness of Heat or Cold and Stretching for Inducing Relaxation in Injured Muscle, The journal of orthopaedic and sports physical therapy, 1982. 1B
- ↑ Steven E. Peres, David O. Draper, Kenneth L. Knight, Mark D. Ricard, Pulsed shortwave diathermy and prolonged long-duration stretching increase dorsiflexion range of motion more than identical stretching without diathermy, Journal of Athletic Training, 2003. 2B
- ↑ 22.0 22.1 22.2 Oosterveld F.G., Rasker J.J., Treating arthritis with locally applied heat or cold, semin Arthritis Rheum., 1994. 5