The Postural Control System
Original Editor - Megyn Robertson
Top Contributors - Samuel Adedigba, Kim Jackson, Mandy Roscher, Lucinda hampton, Heba El Saeid, Rachael Lowe, Megyn Robertson, Stacy Schiurring and Jess Bell
Introduction[edit | edit source]
Postural control is a term used to describe the way our central nervous system (CNS) regulates sensory information from other systems in order to produce adequate motor output to maintain a controlled, upright posture. The visual, vestibular, and somatosensory systems are the main sensory systems involved in postural control and balance[1][2].
- Postural orientation and equilibrium are two main functional goals of postural control[3].
- Postural orientation control the body’s alignment and tone with respect to gravity, support surface, visual environment, and internal references[4].
- The coordination of sensorimotor strategies to stabilize the body’s centre of mass during both self-initiated and externally triggered stimuli constitutes postural equilibrium[4].
Proper postural control is when an individual is able to engage in various static and dynamic activities, such as sitting, standing, kneeling, quadruped, crawling, walking, and running with the ability to contract the appropriate muscles required for a controlled midline posture, as well as the ability to make small adjustments in response to changes in position and movement, without the use of compensatory motions.
If even one of the three abovementioned systems is not working the way it is supposed to, it can affect postural control and balance. However, when one system is affected the other two can be trained to compensate. If more than one system is affected in combination with CNS involvement, postural control will be more greatly affected.
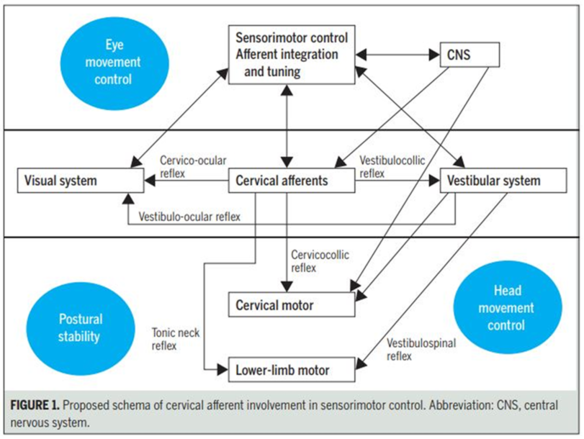
There are important reflexes involved in postural control known as the Cervicocollic Reflex (CCR), the Vestibulo-ocular reflex (VOR) and the Vestibulospinal Reflex (VSR) that work in conjuction with the vestibular nuclei and cerebellum, discussed in the last module (The vestibular system). The visual, vestibular and somatosensory are our three balance systems which are closely linked to control posture.
The Visual System[edit | edit source]
The visual system is the primary receiver of sensory information to maintain postural balance, and as such our postural stability increases with the improvement of the visual environment.
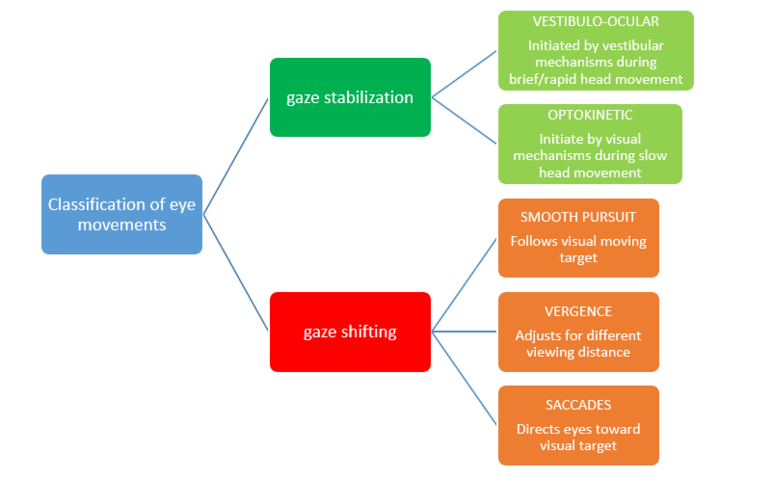
Figure 1: Flow diagram of classification of eye movement systems[5]
There are two functional classes of eye movements: those that stabilize the eye when the head moves or appears to move (gaze stabilization) and those that keep the image of a visual target focused on the fovea of the eye when the visual target changes or moves (gaze shifting).
Gaze Stabilization[edit | edit source]
Two gaze stabilization systems operate during head movement, namely the vestibulo-ocular[6] and the optokinetic systems. For gaze stabilisation to be effective there are conjugate movements in which both eyes move in the same direction.
Gaze Shifting[edit | edit source]
Three gaze shifting systems function to focus the image on the fovea.
- Smooth pursuit uses the eyes to track the movement of a visual target. Essentially, it enables us to stabilise the image of this moving target on / near the fovea.[7] Pursuit movements are described to be voluntary, smooth, continuous, conjugate eye movements with velocity and trajectory determined by the moving visual target.
- Vergence alters the angle between the two eyes to adjust for changes in distance from the visual target. Accommodation is the mechanism by which the eye changes focus from distant to near images. When shifting one's view from a distant object to a nearby object, the eyes converge (are directed nasally) to keep the object's image focused on the foveae of the two eyes.
- Saccades consist of short, rapid, jerky (ballistic) movements of predetermined trajectory that direct the eyes toward some visual target. Eye movements are initiated to bring an object-of-interest into view.
The Vestibular System[edit | edit source]
The vestibular system orientates the trunk to vertical using sensory orientation and weighting appropriate sensory cues under different sensory environments, for example, the patient stands on an inclined surface, or on foam, or with their eyes closed. It also controls the body’s centre of mass (COM) both for static and dynamic positions via postural responses (patient stands or walks on a beam) and stabilises the head during postural movements vis-à-vis the patient leans or is tilted.
The Somatosensory System[edit | edit source]
The somatosensory system is a complex system of sensory neurons and pathways that responds to changes at the surface or inside the body. It is also involved in maintaining postural balance by relaying information about body position to the brain, allowing it to activate the appropriate motor response or movement.
Mechanoreceptors are specific sensory receptors located in the muscle spindles. They provide the nervous system with information about the muscle’s length and velocity of contraction, thus contributing to the individual’s ability to discern joint movement and position sense[8]. The muscle spindles also provide afferent feedback that can be translated into appropriate reflexive and voluntary movements[9].
A very high amount of mechanoreceptors in muscle spindles are found in the suboccipital area, and are responsible for receiving and sending information to and from the CNS[10]. Mechanoreceptor impulses from the occiput to C3 (particulary upper cervical spine muscles) have direct access to vestibular nuclear complex (VNC) - a reflex centre that coordinates vision and neck movement.This same mechanoreceptor input also converges on the central cervical nucleus (CCN). The CCN is effectively a pathway to the cerebellum that integrates vestibular, ocular and proprioceptive information.The VNC also connects with the CCN, so there are interrelated pathways between all the systems. In a nutshell, mechanoreceptor input from the upper cervical region helps to coordinate vision, balance and movement of the neck[10] for effective postural control.
More sensorimotor dysfunction occurs with injury or whiplash associated disorders (WAD) to the upper cervical region than the lower cervical region because the upper region contains more muscle spindles, has a greater connection to the visual and vestibular systems, and more reflex activity[10][11].
For a more in depth analysis and understanding of the role of sensorimotor impairment in neck pain, please see Chris Worsfold’s course on Sensorimotor integration.
Summary[edit | edit source]
The vestibular system, somatosensory system and visual system do not act in isolation but are a complex postural control system that work together to achieve balance.
Postural stability happens with good sensorimotor integration between the upper cervical spine, visual and vestibular structures. Poor postural control occurs if there is a sensory mismatch, in other words the CNS is unable to distinguish between accurate and inaccurate sensory information from one or more of these systems, resulting in feelings of dizziness/unsteadiness/poor balance[10], and disruption in predictive timing of sensory input[12][13].
These patients often complain of headaches, dizziness, blurry vision, frontal headaches, eye strain and balance problems. These patients often have difficulty reading (horizontal deficits), they become headachey/dizzy when looking up at the board and down at the desk during note-taking (vertical deficits). These patients can also experience neck pain, as they may have an increase in muscle activity/stiffness as the body tries to compensate for a loss of balance[10]. They can even be symptomatic while running and trying to focus on a target such as a ball. Some patients complain of feeling disoriented/overwhelmed when driving in an unfamiliar city, driving in tunnels or pushing a trolley in the grocery aisles.
Figure 2: The complex interactions of the Postural Control System (www.semanticscholar.org accessed 7/9/2019)
Additional Resources[edit | edit source]
To learn more about the Postural System watch the lecture below.
References[edit | edit source]
- ↑ Ivanenko Y, Gurfinkel VS. Human postural control. Frontiers in neuroscience. 2018 Mar 20;12:171.
- ↑ Alcock L, O’Brien TD, Vanicek N. Association between somatosensory, visual and vestibular contributions to postural control, reactive balance capacity and healthy ageing in older women. Health care for women international. 2018 Dec 2;39(12):1366-80.
- ↑ Gandolfi M, Valè N, Filippetti M, Dimitrova EK, Geroin C, Picelli A, Smania N. Postural Control in Individuals with Parkinson’s Disease. InPhysiotherapy 2018 Nov 5. IntechOpen.
- ↑ 4.0 4.1 Horak, F.B. (2006). Postural orientation and equilibrium: What do we need to know About neural control of balance to prevent falls? Age and Ageing, 35(S2), ii7-ii11. doi: 10.1093/ageing/afl077
- ↑ https://nba.uth.tmc.edu/neuroscience/m/s3/chapter07.html (accessed 5 July 2019)
- ↑ Pritcher, M.R., Whitney, S.L., Marchetti, G.F. and Furman, J.M., 2008. The influence of age and vestibular disorders on gaze stabilization: a pilot study. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 29(7), p.982.
- ↑ Ono S, Kizuka T. Effects of Visual Error Timing on Smooth Pursuit Gain Adaptation in Humans. J Mot Behav. 2017;49(2):229-34.
- ↑ Shaffer SW, Harrison AL, Aging of the somatosensory system: a translational perspective. Phys Ther. 2007; 87 (2):193-207
- ↑ Kröger S. Proprioception 2.0: novel functions for muscle spindles. Current opinion in neurology. 2018 Oct 1;31(5):592-8.
- ↑ 10.0 10.1 10.2 10.3 10.4 Kristjansson E, Treleaven J, Sensorimotor function and Dizziness in Neck Pain: Implications for Assessment and Management. JOSPT 2009; 39 (5):364-77
- ↑ Treleaven J, Clamaron-Cheers C, Jull G. Does the region of pain influence the presence of sensorimotor disturbances in neck pain disorders?. Manual therapy. 2011 Dec 1;16(6):636-40. Abstract: [Accessed 26 June 2018] Available from: https://www.sciencedirect.com/science/article/pii/S1356689X11001214
- ↑ Howell DR, Osternig LR, Koester MC, Chou L-S (2014). The effect of cognitive task complexity on gait stability in adolescents following concussion. Exp Brain Res 232(6):1773–82.10.1007/s00221-014-3869-1
- ↑ King LA, Horak FB, Mancini M, Pierce D, Priest KC, Chesnutt J, et al. Instrumenting the balance error scoring system for use with patients reporting persistent balance problems after mild traumatic brain injury. Arch Phys Med Rehabil (2014) 95(2):353–9.10.1016/j.apmr.2013.10.015