The Postural Control System
Original Editor - Megyn Robertson
Top Contributors - Samuel Adedigba, Kim Jackson, Mandy Roscher, Lucinda hampton, Megyn Robertson, Heba El Saeid, Rachael Lowe, Jess Bell and Stacy Schiurring
Introduction[edit | edit source]
Postural control is a term used to describe the way our central nervous system (CNS) regulates sensory information from other systems in order to produce adequate motor output to maintain a controlled, upright posture. The visual, vestibular, and somatosensory systems are the main sensory systems involved in postural control.
Postural orientation and equilibrium are two main functional goals of postural control. Postural orientation control the body’s alignment and tone with respect to gravity, support surface, visual environment, and internal references[1]. The coordination of sensorimotor strategies to stabilize the body’s centre of mass during both self-initiated and externally triggered stimuli constitutes postural equilibrium[1].
So what does proper postural control look like? This is when an individual is able to engage in various static and dynamic activities, such as sitting, standing, kneeling, quadruped, crawling, walking, and running with the ability to contract the appropriate muscles required for a controlled midline posture, as well as the ability to make small adjustments in response to changes in position and movement, without the use of compensatory motions. If even one of the three abovementioned systems is not working the way it is supposed to, it can affect postural control and balance. However, when one system is affected the other two can be trained to compensate. If more than one system is affected in combination with central nervous system involvement, postural control will be more greatly affected.
So far we have discussed the 3 important reflexes, namely the CCR, VOR and VSR. We have learnt that there are pathways that work in conjunction with the vestibular nuclei and cerebellum. We are now going to learn about 3 balance systems (visual, vestibular and somatosensory) with close neurophysiological pathways.
The Visual System[edit | edit source]
The primary sensory information to maintain postural balance is the visual system[2]. Therefore, postural stability increases with the improvement of the visual environment.
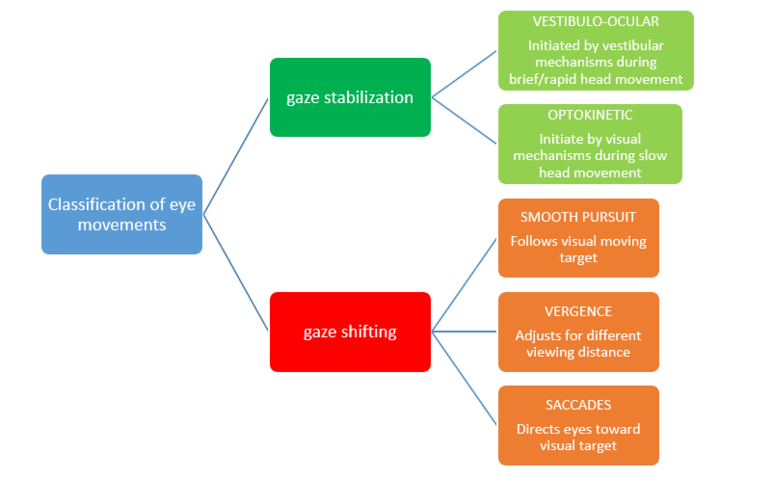
There are two functional classes of eye movements: those that stabilize the eye when the head moves or appears to move (gaze stabilization) and those that keep the image of a visual target focused on the fovea when the visual target changes or moves (gaze shifting).
Gaze Stabilization[edit | edit source]
Two gaze stabilization systems operate during head movement, namely the vestibulo-ocular and the optokinetic systems. For gaze stabilisation to be effective there are conjugate movements in which both eyes move in the same direction.
Gaze Shifting[edit | edit source]
Three gaze shifting systems function to focus the image on the fovea.
- Smooth Pursuit uses the eyes to track the movement of a visual target. Pursuit movements are described to be voluntary, smooth, continuous, conjugate eye movements with velocity and trajectory determined by the moving visual target.
- Vergence alters the angle between the two eyes to adjust for changes in distance from the visual target. Accommodation is the mechanism by which the eye changes focus from distant to near images. When shifting one's view from a distant object to a nearby object, the eyes converge (are directed nasally) to keep the object's image focused on the foveae of the two eyes.
- Saccades consist of short, rapid, jerky (ballistic) movements of predetermined trajectory that direct the eyes toward some visual target. Eye movements are initiated to bring an object-of-interest into view.
The Vestibular System[edit | edit source]
The vestibular system was discussed in detail earlier in this chapter. In summary the vestibular system orientates the trunk to vertical using sensory orientation and weighting appropriate sensory cues under different sensory environments (for example the patient stands on inclined surface, or on foam, with eyes closed). It also controls the body’s centre of mass (COM) both for static and dynamic positons via postural responses (patient stands or walks on a beam) and stabilises the head during postural movements vis-à-vis the patient leans or is tilted.
The Somatosensory System[edit | edit source]
The somatosensory system is a complex system of sensory neurons and pathways that responds to changes at the surface or inside the body. It is also involved in maintaining postural balance by relaying information about body position to the brain, allowing it to activate the appropriate motor response or movement.
Mechanoreceptors are specific sensory receptors located in the muscle spindles. They provide the nervous system with information about the muscle’s length and velocity of contraction, thus contributing to the individual’s ability to discern joint movement and position sense[4]. The muscle spindles also provide afferent feedback that can be translated into appropriate reflexive and voluntary movements.
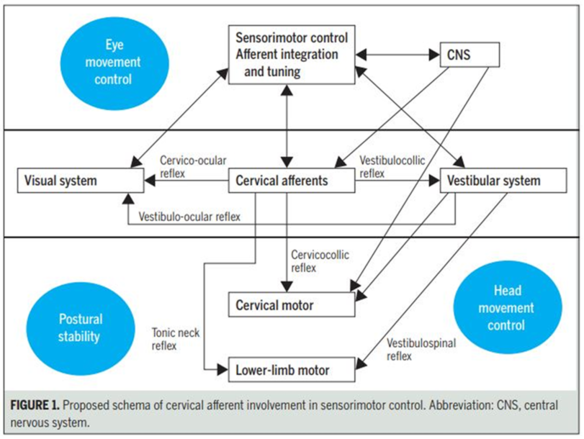
A very high amount of mechanoreceptors in muscle spindles are found in the suboccipital area, and are responsible for receiving and sending information to and from the central nervous system[5]. Mechanoreceptor impulses from neck are then transmitted through the nerve cells in the C2 and C3 dorsal root ganglion (DRG) which have direct access to vestibular nuclei. Mechanoreceptor input from C0-2 converges on the central cervical nucleus (CCN) in the C1-2 segments of the spinal cord. The CCN integrates vestibular, ocular and proprioceptive information. In a nutshell, mechanoreceptor input from the upper cervical region and muscles leads to a coordination between vision and movement of the neck[6].
More sensorimotor dysfunction occurs with injury or whiplash associated disorders to the upper cervical region than the lower cervical region because the upper region contains more muscle spindles, has a greater connection to the visual and vestibular systems, and more reflex activity[6][7].
For a more indepth analysis and understanding of the role of sensorimotor impairment in neck pain, please see Chris Worsfold’s course on Sensorimotor integration.
Summary[edit | edit source]
The vestibular system, somatosensory system and visual system do not act in isolation, but are a complex postural control system that integrate together to achieve balance.
Postural stability changes happen because of changes in the sensory input between the upper cervical spine and the vestibular structures. Thus the patient’s vestibular structures are unable to distinguish between the inaccurate information resulting in a sensory mismatch that leads to feelings of dizziness/unsteadiness/poor balance[6], and disruption in predictive timing of sensory input[8][9].
These patients often complain of headaches, dizziness, blurry vision, frontal headaches, eye strain and balance problems. These patients often have difficulty reading (horizontal deficits), they become headachey/dizzy when looking up at the board and down at the desk during note taking (vertical deficits).These patients can also experience neck pain, as they may have an increase in muscle activity/stiffness as the body tries to compensate for a loss of balance[6]. They can be symptomatic while running and trying to focus on a target such as a ball. Some patients complain of feeling disoriented/overwhelmed when driving in an unfamiliar city.
References[edit | edit source]
- ↑ 1.0 1.1 Horak, F.B. (2006). Postural orientation and equilibrium: What do we need to know About neural control of balance to prevent falls? Age and Ageing, 35(S2), ii7-ii11. doi: 10.1093/ageing/afl077
- ↑ Uchiyama & Demura, 2009.
- ↑ https://nba.uth.tmc.edu/neuroscience/m/s3/chapter07.html (accessed 5 July 2019)
- ↑ Shaffer & Harrison, 2007.
- ↑ Is it Treleaven et al 2001 or 2011?
- ↑ 6.0 6.1 6.2 6.3 Kristjansson E, Treleaven J (2009). Sensorimotor function and dizziness in neck pain: implications for assessment and management. JOSP 39(5):364-77. [Accessed 26 June 2018] Available from: http://www.neckcare.com/wp-content/uploads/Sensorimotor-function-and-dizziness-in-neck-pain_Implication-for-assessment-and-management.pdf
- ↑ Treleaven J, Clamaron-Cheers C, Jull G. Does the region of pain influence the presence of sensorimotor disturbances in neck pain disorders?. Manual therapy. 2011 Dec 1;16(6):636-40. Abstract: [Accessed 26 June 2018] Available from: https://www.sciencedirect.com/science/article/pii/S1356689X11001214
- ↑ Howell DR, Osternig LR, Koester MC, Chou L-S (2014). The effect of cognitive task complexity on gait stability in adolescents following concussion. Exp Brain Res 232(6):1773–82.10.1007/s00221-014-3869-1
- ↑ King LA, Horak FB, Mancini M, Pierce D, Priest KC, Chesnutt J, et al. Instrumenting the balance error scoring system for use with patients reporting persistent balance problems after mild traumatic brain injury. Arch Phys Med Rehabil (2014) 95(2):353–9.10.1016/j.apmr.2013.10.015