Tetanus
Original Editors - Natalie Gutmann from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Natalie Gutmann, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, WikiSysop, 127.0.0.1 and Wendy Walker
Definition/Description[edit | edit source]
Tetanus derived from the greek word "to stretch"[1] is an acute disease caused by the anaerobic (without oxygen)
, gram positive, non-capsulated spore forming bacteria Clostridium tetani ("C. tetani"). C. tetani can resist very high temperatures and is not spread from person to person. Tetanus is a rare and often fatal neurological disease that causes increased tone and muscle spasms due to the bacteria.[2],[3] The most common way the bacterium enters the body is through wounds which are susceptible to infection if they are: “contaminated with soil, feces, or saliva, puncture wounds including unsterile injection sites, devitalized tissue including burns, avulsions and degloving injuries”.[4]
The disease tetanus extends all the way back to the fifth century BC. However, it was not until the late 1800s that Arthur Nicolaier discovered the toxins that caused tetanus which have the ability to infect several species and that protection could be provided by passive transfer of an antitoxin. A few years after the discovery of the tetanus toxins Robert Koch was able to obtain a culture of the bacteria.[3][1] In 1924, the immunization to protect people against tetanus was developed by Pierre Descombey and by 1940 the tetanus immunization became routine in children’s vaccinations.[1][2]
Prevalence[edit | edit source]
In the United States, from 2000-2007 there has been an “average of 31 reported cases per year with the majority of them being over the age of 40.”[5] In recent years the percent of people who contract the bacteria, to those that die from it, has decreased from 30% to 10%. Since 1989 there has only been 2 reported cases of tetanus in the neonatal population.[5] It is estimated that about 800,000 to one million people die of tetanus every year worldwide.[2] The majority of the cases are found in underdeveloped countries with children and neonates representing most of the cases due to inadequate immunizations and unhealthy medical procedures especially during childbirth.[4] The prevalence of tetanus in the United States has been identified in males over the age of 50, women without formal education, and African Americans in the southern states. Recently, immigrants and intravenous drug users have had a higher prevalence for contracting tetanus. Anyone over the age of 60 are at an increased risk for contracting tetanus due to the fact that they may not have received the protective immunity. [2]
Characteristics/Clinical Presentation[edit | edit source]
There are four different forms of tetanus: generalized tetanus, local tetanus, cehalic tetanus, and neonatal tetanus.
Generalized tetanus
Generalized tetanus attacks muscles throughout the entire body and is the most common form of te
tanus occuring in about 80% of the cases.[5][6] In generalized tetanus, the tetanospamin attacks and inhibits mostly the motor neurons of the CNS and later the neurons of the ANS as well. As a result a person experiences uncontrollable intense muscle contractions.[4] The first muscles affected are the facial and jaw muscles because of their short nerve pathways. This condition is commonly referred to as lock jaw or trismus. As the disease progresses the person will experience stiffness of the neck, difficulty swallowing, and stiffness of the abdominal muscles.[4][5] Spasms can be produced by a stimulus such as light, noise, touch, or happen unexpectedly with no specific cause.[4] Spasms are extremely painful and can occur frequently and can last for several minutes.[4][5] In generalized tetanus “spasms continue for 3-4 weeks and complete recovery may take months.”[5] After several days the ANS will be affected showing others signs such as fever, sweating, elevated blood pressure, and increased or rapid heart rate.[4][5]
Local tetanus
Local tetanus can occur before generalized tetanus but this is a much milder form with a decreased amount of associated toxin release.[4] Local tetanus, for the most part, just attacks muscles in a specific (local) area of the body[6] Localized tetanus is rare, but there is a better prognosis with only about 1% of the cases resulting in death.[5] The presentation of local tetanus is muscle rigidity and continuous contractions close to the injury site.[4][5]
Cehalic tetanus
Cehalic tetanus is also rare and shows a combination of both generalized and local tetanus.[4] The characteristics of this type of tetanus are facial spasms and paralysis as a result of involvement of the cranial nerves. Head wounds are the main cause with occasional occurrence found with ear infections (otitis media) associated with a head wound.[3][4][5][6] Cehalic tetanus can progress to generalized tetanus and can be associated with a high fatality rate.[4]
Neonatal tetanus
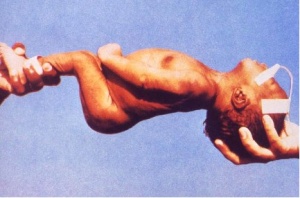
Neonatal tetanus (which is found in newborn babies) is a form of generalized tetanus which also has a high fatality rate.[4] The diagnosis is determined from the symptoms that present. When the baby is born they are able to suck and swallow normally for 2-3 days and then they lose that ability. The symptoms of neonatal tetanus are muscle rigidity and spasms which appear around "4-14 days after birth”.[5][7] The most common way neonatal tetanus occurs is due to non- immune mothers and poor hygiene during the delivery process.[4] Most of the cases of infected infants is a result of infection of the unhealed stump of the umbilical cord especially if the cord has been cut with unsterile instruments. Neonatal tetanus is very common in third world countries.[5]
Images: http://phil.cdc.gov/phil/quicksearch.asp
Associated Co-morbidities[edit | edit source]
- Laryngospasm: Spasms in the muscles of respiration which can interfere with breathing[5]
- Fractures: As a result of spasms, most frequently affect the spine and long bones[5]
- Hypertension or abnormal heart rhythm: Due to hyperactivity of the ANS[5]
- Nosocomial infections: Due to prolonged hospitalization[5]
- Pulmonary Embolism: Mostly seen in the elderly and drug users[5]
- Aspiration pneumonia: Found in the elderly and late stages of tetanus[5]
Medications[edit | edit source]
If an individual has contracted tetanus the drugs of choice and most commonly used to help remove the infection are Penicillin and Metronidazole. Other alternatives are Erthromycin, Tetracycline, Chloramphenicol, and Clindamycin.[6][8][9]
- Penicillin: Has been used for many years but it is a GABA antagonist and is associated with convulsions.[9]
- Metronidazole: Has recently been discovered and is the best option for treating and preventing anaerobic bacterial diseases.[9]
Vaccinations:
Tetanus can be prevented through vaccinations. The vaccination consists of being injected with the tetanus toxoid. The toxoid is available in two different forms: absorbed toxoid and fluid toxoid. The toxoids work by producing specific antitoxins that will neutralize the bacteria. The toxoid is inactivated and does not contain any live organisms. Therefore, the toxoids can not replicate themselves once injected which is why it requires several doses to prevent immunity.[6][9][1] The tetanus vaccine has been combined with pertussis and diptheria to make the DTP vaccine for infants.[7] The vaccination is started in infants 2 months of age in a series of four injections on monthly intervals. The next injections are given at 4, 6, and 15-18 months of age. A booster shot is given to the child between ages 4-6. For adolescents and adults the Tdap vaccine is used which is a combination of tetanus and diphtheria toxin with acellular pertussis.[4][5][1] It is recommended to get a booster shot every 10 years.[10]
- DTaP(dipteria and tetnus toxoid and acellular pertussis): Given to infants 6 weeks to 6 years of age.[5][1]
- DT(diptheria and tetanus toxoid) : Given to infants 6 weeks to 6 years who have a contraindication for perussis.[5][1]
- Tdap (tetanus and diptheria toxoid and acellular perrussis): Given as a one time does to adolescents and adults.[5][1]
- Td(tetanus and diphtheria toxoid): Given to children and adults 7 years and older. Contains smaller dosages of diptheria.[5][1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
There are no specific laboratory or diagnostic tests used to diagnosis tetanus. The diagnosis is made based on clinical signs and symptoms and not on the confirmation of the bacteria C. tetani in the body. [5][6]“C. tetani is recovered from the wound in only 30% of cases and can be isolated from patients who do not have tetanus.”[5]
Etiology/Causes[edit | edit source]
Once the bacteria C. tetani enters the body the spores multiply and germinate due to the anaerobic environment. In the body, two toxins are released: tetanospamin and tetenolysin.[2][6] It is not certain the exact role of tetanolysin but it is believed that it works together with the toxin tetanospamin.[2][5] Tetanospamin reaches the peripheral nerves by retrograde neuronal transport through the blood or lymphatic system.[2][6] “The length of the peripheral nerves determines how long it takes for the neurotoxins to reach the CNS and cause symtoms. The toxin tetanospamin disrupts the release of the inhibitory neurotransmitters glycine and GABA throughout the CNS but most commonly at the motor end plates, spinal cord, brain, and sympathetic nervous system”.[2] “The disinhibition allows for unopposed muscular contraction followed by muscular rigidity and spasms”.[2] Once the bacteria has entered the body the incubation period may range from days to months. The average incubation period is around 4-14 days. The incubation period is shorter the closer the injury site is to the CNS.[2][3][5] A shorter incubation period usually correlates with poor prognosis due to a more severe disease.[3]
Systemic Involvement[edit | edit source]
Cardiovascular:[3]
- Hyperkinetic circulation is a result of elevated basal sympathetic and muscle activity.[8]
- Tachycardia with hypertension
- Increased stroke volume
- Thromboembolus
Respiratory:[8]
- Muscular spasms: chest wall, diaphragm, abdomen, pharyngeal, and laryngeal tract (can lead to an obstructed airway which can be life threatening)
- Atelectasis, pneumonia, and aspiration: inability to cough secondary to muscular rigidity, spasms, and being sedated.
- Hyperventilation: common because of fear and autonomic disturbances.
Renal:[8]
Renal involvement is only found in severe cases of tetanus.
- Dehydration
- Urinary stasis and infection
- Renal failure
- Altered renal blood flow secondary to catecholamine surges
Gasto-intestinal:[8]
- Gastric statis
- Illeus
- Diarrhea
- Hemorrhage
- Weight loss: As a result of the inability to swallow
Neuromuscular:[3]
- Autonomic dysfunction: Leads to excess sympathetic activation and catecholamine levels
- Muscle rigidity and spasms
- Lock-jaw (trismus)
- Risus sardonicus
- Opisthotonos (reactions of the head)
- Tendon avulsions: a result of spasms
- Fractures: a result of spasms
Medical Management (current best evidence)[edit | edit source]
The management of tetanus is categorized into three steps. First the organism in the body needs to be destroyed to prevent further release of the toxin. Next the toxin in the body outside of the CNS needs to be neutralized and finally the effects of the toxin in the CNS need to be minimized.[6][8] Wound debridement, if possible, should be done to help remove the toxin from the body.[6] The general medical management consists of controlling the spasms, prevent other infections, control fluid and electrolyte balance, and respiratory support.[6][9][1] The primary way to control muscle spasms is sedation and muscle relaxants.[9] The prognosis of individuals with tetanus depends on the supportive care and ventilatory access.[6]
Physical Therapy Management (current best evidence)[edit | edit source]
Currently research is limited on the Physical therapy management of individuals with tetanus. Cardiopulmonary physical therapy can be used to help in the prevention of respiratory complications.[8] Physical therapy can also be used to help with muscle rigidity and spasms.
Differential Diagnosis[edit | edit source]
- Orofacial infection[6][8]
- Dystonic drug reactions[6][8]
- Hypocalcaemia[6][8]
- Strychnine poisoning[6][8]
- Seizures[6][8]
- Infections of the head, neck, and central nervous system[6][8]
Case Reports/ Case Studies
[edit | edit source]
- Katz K, Walmsley S. Postoperative tetanus: a case report. CMAJ 200: 163(5):571-3. http://canadianmedicaljournal.ca/cgi/reprint/163/5/571
- Grunau B, Olson J. An interesting presentation of pediatric tetanus. CJEM: Canadian Journal Of Emergency Medical Care = JCMU: Journal Canadien De Soins Médicaux D'urgence. January 2010;12(1):69-72. Available from: MEDLINE, Ipswich, MA. Accessed March 16, 2011. http://www.cjem-online.ca/v12/n1/p69
- Quackenbush P, Tuorinsky S, Rabb R. Tetanus Diagnosis Sometimes Elusive. Nurse Practitioner. November 2003;28(11):50-53. http://web.ebscohost.com.libproxy.bellarmine.edu/ehost/pdfviewer/pdfviewer?sid=8b4e7522-592e-4f01-9971-d7d388843320%40sessionmgr14&vid=5&hid=10
Resources
[edit | edit source]
CDC: http://www.cdc.gov/vaccines/vpd-vac/tetanus/default.htm
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14I4jFUaJ8_ce_WWgfrGngd: Error parsing XML for RSS
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Parker J. Managing tetanus. (Cover story). Emergency Nurse. July 2006;14(4):14-17. Available from: Academic Search Premier, Ipswich, MA. Accessed March 16, 2011
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Wakim N, Henderson S. Tetanus. Topics in Emergency Medicine. July 2003;25(3):256-261.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Linnenbrink T, McMichael M. Tetanus: pathophysiology, clinical signs, diagnosis, and update on new treatment modalities. Journal of Veterinary Emergency & Critical Care. September 2006;16(3):199-207.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Ewcombe P. Treating and preventing tetanus in A&E. Emergency Nurse. October 2004;12(6):23-29.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 5.24 5.25 5.26 CDC. Tetanus: Questions and Answers. November 2010.www.immunize.org.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 Grunau B, Olson J. An interesting presentation of pediatric tetanus. CJEM: Canadian Journal Of Emergency Medical Care = JCMU: Journal Canadien De Soins Médicaux D'urgence. January 2010;12(1):69-72. Available from: MEDLINE, Ipswich, MA. Accessed March 16, 2011.
- ↑ 7.0 7.1 Tetanus vaccine. Relevé Épidémiologique Hebdomadaire / Section D'hygiène Du Secrétariat De La Société Des Nations = Weekly Epidemiological Record / Health Section Of The Secretariat Of The League Of Nations. May 19, 2006;81(20):198-208. Available from: MEDLINE, Ipswich, MA. Accessed March 16, 2011.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 Cook T, Protheroe R, Handel J. Tetanus: a review of the literature. British Journal Of Anaesthesia. September 2001;87(3):477-487. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2011.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Ahmadsyah I, Salim A. Research from the South: Treatment of tetanus: an open study to compare the efficacy to procaine penicillin and metronidazole. British Medical Journal (Clin Res Ed). September 7, 1985;291(6496):648. Available from: Academic Search Premier, Ipswich, MA. Accessed April 2, 2011.
- ↑ . Fraser D. Preventing Tetanus in Patients with Wounds. Annals of Internal Medicine. January 1976:95. Available from: Academic Search Premier, Ipswich, MA. Accessed April 2, 2011.