Supraspinatus Tear
Original Editor - Brecht Haex
Top Contributors - Kim Jackson, Leana Louw, Mats Vandervelde, Brecht Haex, Fasuba Ayobami, Vidya Acharya, Habibu Salisu Badamasi, Wendy Walker, Naomi O'Reilly, Saimat Lachinova, Simisola Ajeyalemi, Wout Van Hees, Joao Costa, Shreya Pavaskar, Rachael Lowe, Anthony Mertens and Wanda van Niekerk
Definition/Description[edit | edit source]
A supraspinatus tear is a tear or rupture of the tendonof the supraspinatus muscle. The supraspinatus is part of the rotator cuff of the shoulder. The rotator cuff consists of M. Supraspinatus, M. Infraspinatus, M. Subscapularis and M. Teres minor (<R> http://www.physio-pedia.com/Rotator_Cuff). Most of the time it is accompanied with another rotator cuff muscle tear (<R> http://www.physio-pedia.com/Rotator_Cuff_Tears ). This tear can occur in 2 ways. Due to a trauma or due repeated micro-trauma. The supraspinatus tear can be partial or full thickness tear [1]. A partial tear means that the soft tissue (the muscle fibers) will not be completely disrupted. A complete tear on the other hand means that all the muscle fibers are disrupted. It is common that disrupted tendons begin by fraying and when the damage progresses the partial tear evolves into a complete tear[1]. Most of the time the tear occurs in the tendon or as an avulsion from the greater tuberosity[2]. The supraspinatus muscle is responsible for the abduction of the upper limb[1].
Clinical Relevant Anatomy[edit | edit source]
The shoulder joint is made up of three bones: the humerus (the upper arm), the scapula (shoulder blade) and the clavicle (collarbone). The head of the humerus fits into a fordable socket in the scapula so it is a ball-and-socket joint[1]. The supraspinatus muscle is located on the back of the shoulder. This muscle arises from the supraspinous fossa of the scapula and inserts on the greater tubercle of the humerus. The supraspinatus muscle is innervated by the nervus supraspinatus (C5-C6)[3].
The supraspinatus muscle is part of the rotator cuff. The rotator cuff is a group of muscles[1]. It consists of the supraspinatus muscle, the infraspinatus muscle, the teres minor and the subscapularis. These muscles with their tendons stabilize, control and move the shoulder[4]. It also prevents subluxation of the shoulder.
The rotator cuff covers the head of the humerus and keeps it into place. The muscles help to lift and rotate the arm. Position of the arm to be able to palpate the tendon to apply deep transverse friction or Ultrasound to the full width of the tendon: the shoulder should be rotated internally (forearm behind the back) so the supraspinatus tendon appears more in the frontal plane of the shoulder.
Joints[edit | edit source]
Epidemiology/Etiology[edit | edit source]
The etiology is multifactorial consisting of age-related degeneration , microtrauma and macrotrauma. The incidence increases with the age. The half of individuals have a supraspinatus tear in their 80s. Smoking, hypercholesterolemia, and genetics affect the development of tearing. Substantial full-thickness tears progress and enlarge with time. Pain, or worsening pain, usually signals tear progression in asymptomatic and symptomatic tears and should warrant further investigation if the tear is treated conservatively. Smaller symptomatic full-thickness tears ( < 1 cm ) and partial – thickniss tears have a slower rate of progression and can be treated with a nonoperative treatment. In both cases increasing pain should alert physicians to obtain further imaging as it can signal tear progression. Larger symptomatic full-thickness tears ( > 1cm -1,50 cm )have a high rate of progression and should be considered for earlier surgical repair in younger patients if the tear is reparable and the muscle degeneration is limited. This is important to avoid irreversible changes to the cuff. A nonoperative treatment can be used in older patients ( older than 70 years ) who have a chronic tear , in patients with irreparable tears with irreversible changes , in patients of any age with small (<1 cm) full-thickness tears or in patients without a full-thickness tear. An operative treatment can be used in acute tears (>1 cm-1.5 cm) or young patients with full-thickness tears who have a significant risk for the development of irreparable rotator cuff changes[5].
Rotator cuff tears were associated with older patients, males, a history of trauma and affected the dominant arm. Patients have also a reduced forward elevation , external rotation and abduction. We can conclude that the risk factors for a tear consist of a history of trauma, dominant arm and age.[6]
Injury and degeneration are the two main causes of rotator cuff tears.
An acute tear can be get when you fall down on your outstretched arm or when you lift something too heavy. This type of tear can occur with other shoulder injuries, such as a broken collarbone or dislocated shoulder.
Most of the cases are the result of a wearing down of the tendon that occurs slowly over time. That is called a degenerative tear. This degeneration increases with the age and are more common in the dominant arm. When you have a degenerative tear in one shoulder , you have a greater risk for a tear in the opposite shoulder, even if you have no pain in the opposite shoulder.
There are several factors that contribute to degenerative or chronic tears.
• Repetitive stress
• Lack of blook supply
• Bone spurs ( bone overgrowth )
Risk Factors[edit | edit source]
- Older than 40 years old have a greater risk
- Body Mass Index
- Height
- Repetitive Lifting
- Overhead Activities and other people who do overhead work have a greater risk
- Tennis Players
- Baseball Pitchers
- Painters
- Carpenters
- Plumbers
- Traumatic Injury e.g. a fall, more common cause in younger individuals[1]
So we can conclude that rotator cuff tears are associated with older patients, a history of trauma and affected the dominant arm. Patients have also a reduced forward elevation, external rotation and abduction. The most common risk factors for a tear consist of a history of trauma, dominant arm and age.
Characteristics/Clinical Presentation[edit | edit source]
The most common symptoms of a rotator cuff tear include:
- Pain when lifting and lowering your arm or with specific movements
- Pain at rest
- Pain at night, predominantly when you lie on the affected shoulder
- Weakness when rotating or lifting your arm
- Crepitus
- Clicking
- Stiffness
- Limitation of Motion
- Instability[1][7]
Sudden, traumatic tears that usually cause intense pain, often accompanied by a snapping sensation and immediate weakness in your upper arm.
A rotator cuff injury can make it painful to lift your arm out to the side.
Tears that are developed slowly due to overuse cause also pain and weakness in the upper arm. You may have pain in the shoulder when you lift your arm to the side , or pain that moves down your arm. The pain is usually located anterolaterally and superiorly and referred to the level of the deltoid insertion with full-thickness tears. In the beginning the pain may be mild and only present when lifting your arm. But over time the pain can become more noticeable at rest. You can have pain when you lie on the affected shoulder at night. The pain and weakness in the shoulder and upper arm can make routine activities (combing your hair or reaching behind your back ) or overhead activities/movements (racket sports) more difficult or impossible. So the pain is aggravated in activities where the arm must be in an overhead or a forward-flexed position.
When the tear is acute, the pain is suddenly arised after a fall or after lifting a heavy object or even after a trivial amount of force.
So we can conclude that pain is the most common symptom. The next most common symptoms of a rotator cuff tear are following pain, limitation of motion and weakness[1].
Differential Diagnosis[edit | edit source]
- Acromioclavicular Joint Injury
- Brachial Plexus Injury[8][9]
- Bicipital Tendinopathy[8]
- Cervical Radiculopathy[8][9]
- Cervical Spine Sprain[8]
- Cervical Strain Injuries[8]
- Cervical Disc Injuries[8]
- Cervical Nerve Root Injury
- Cervical Spondylosis
- Cervical Discogenic Pain Syndrome[8]
- Clavicular Fracture [8]
- Sternoclavicular Joint Disorders [8]
- Infraspinatus Syndrome[8]
- Contusions[8]
- Rotator Cuff Tear[8]
- Shoulder Dislocation[8]
- Myofascial Pain[8]
- Shoulder Impingement Syndrome[8]
- Superior Labrum Lesions[8]
- Shoulder Subluxation [8]
- Angina Pectoris[9]
- Myocardial Infarction[9]
- Subacromial Impingement
- Osteoarthritis
- Rheumatoid Arthritis
- Subscapular Nerve Entrapment
- Shoulder Instability
Diagnostic Procedures[edit | edit source]
Diagnostic Procedures should be based on
History[edit | edit source]
- Duration of Pain
- Pain Provocation
- Night Rest
- Same problems in the past?
X-Rays[edit | edit source]
- X-rays can be used as an extra test to exclude sclerosis and osteophyte-formation on the acromion.
- X-rays can also measure the size of the subacromial space.
- On the x-ray itself you can’t see the tendon, therefore you need to use a MRI or CT-scan.
MRI[edit | edit source]
- MRI can show partial tears or full tears in the tendons of the rotator cuff , inflammation to weak structures and cracks in the capsule.
Clinical examination
Outcome Measures[edit | edit source]
A wide variety of outcome measures have been used to evaluate the efficacy of Rotator Cuff (RC) treatments by assessing changes in patient function over the study period. The majority of scales used in the RC literature are disease-specific questionnaires developed for the assessment of the shoulder; however, generic scales (e.g., SF-36=non specific; QoL measre?) have also been used. The scales can broadly be classified into health-related quality of life and functional outcome measures. Health-related quality scales are developed with the intent of assessing patients‘ perception of the impact of their condition on their physical, social, psychological/emotional, and cognitive state. Functional outcome measures evaluate a patient‘s ability to perform activities of daily living and frequently incorporate clinically assessed components, such as range-of-motion or strength.[10]
Three health-related quality of life measures were used in the studies reviewed in this report: the Rotator Cuff Quality of Life (RC-QOL) scale, the Short-Form-36 (SF-36) and the Western Ontario Rotator Cuff (WORC) index. These self-reported scales assess similar domains, such as pain, physical symptoms, social and emotional functioning. The RC-QOL and SF-36 are scored on a scale of 0 to 100 points, where higher scores indicate better quality of life, while the WORC Index provides a score of up to 2,100 points with higher scores indicating poorer outcomes. There is evidence to support the reliability and convergent validity of each of the scales.[10]
About the DASH
The Disabilities of the Arm, Shoulder and Hand (DASH) Outcome Measure is a 30-item, self-report questionnaire designed to measure physical function and symptoms in patients with any or several musculoskeletal disorders of the upper limb.The questionnaire was designed to help describe the disability experienced by people with upper-limb disorders and also to monitor changes in symptoms and function over time. Testing has shown that the DASH performs well in both these roles.It gives clinicians and researchers the advantage of having a single, reliable instrument that can be used to assess any or all joints in the upper extremity.The DASH Outcome Measure contains two optional, four-item modules intended to measure symptoms and function in athletes, performing artists and other workers whose jobs require a high degree of physical performance. Because they may be having difficulties only at high performance levels–which are beyond the scope of the 30-item DASH Outcome Measure–clinicians may find the modules, which are scored separately from the DASH, useful in assessing these special patients.
DASH and QuickDASH Scoring Formula = ([(sum of n responses)/n] -1)(25) where n represents the number of completed items.
• DASH cannot be computed if greater than three items are missing[1].
• QuickDASH cannot be computed if greater than 1 item is missing.[1]
Level of Disability
In both the DASH and QuickDASH a higher scores indicate a greater level of disability and severity, whereas, lower scores indicate a lower level of disability. The score on both test ranges from 0 (no disability) to 100 (most severe disability). The Minimal Detectable Change (MDC= the smallest amount of change that has to occur before the change can be considered a true change and not error) for the DASH is 12,75-17,23%.
The Minimal Clinical Important Difference (MCID= the amount of change in the score that has to occur before it signifies an important or beneficial difference in the patient’s condition) is 10.83 points for the DASH[11].
DASH (http://www.dash.iwh.on.ca/scoring)[12]
ICC: 0.96 [13] Cronbach alpha: 0.97
- Quick DASH (http://www.dash.iwh.on.ca/scoring)
ICC: 0.94 [13] Cronbach alpha: 0.94
- Penn Shoulder Score: to measure outcome of patients with various shoulder disorders
ICC: 0.94 [14] Cronbach alpha: 0.93 ]
- Global Rating of Change Scale: to measure improvement
ICC: 0.74
Clinical Examination[edit | edit source]
Physical examination starts with inspection. Atrophy of the shoulder muscles is a common finding in patients with rotator cuff tears. The position and motion of the scapula is also important. The scapula rotates upward and downward during arm elevation/depression. This smooth movement of the scapula on the thorax may have deteriorated because of subacromial impingement or rotator cuff defect. For the purpose of identifying which tendon is ruptured, various location-specific physical examinations have been reported. A tear of the supraspinatus tendon can be detected by several tests.[13]
The drop-arm test, active shoulder abduction to 90°, then return – dropping the arm down with pain indicates a positive test, produced a positive likelihood ratio above 10 or a negative likelihood ratio below 0,1 in two evaluations, but other studies are doubting the test.[14]
The empty can test (also know as the supraspinatus test or Jobe test), resisted shoulder abduction in internal rotation, demonstrated diagnostic accuracy only once in 21 evaluations across six studies. Kim et al. reported a negative likelihood ratio of 0,03 using pain or weakness as a criterion, with full or partial thickness tears. [14]
The full can test, resisted shoulder abduction in external rotation, demonstrated a lack of diagnostic accuracy, using pain and/or weakness as criteria.
Investigating palpation of the supraspinatus tendon for a tendon rupture reportd high sensivity values (and specifity) thus producing the most accurate result reported in the review. With a LR+of 29,91 and a LR- of 0,04.[14]
Another test is the subacromial grind test, With the patient standing and examiner standing facing the patient, the examiner grasps the patient's flexed elbow. The shoulder is passively abducted in the scapular plane to 90° (Hawkins-Kennedy test position) The examiner's other hand is placed over the patient's shoulder overlying the anterior acromion and greater tuberosity. The examiner passively internally and externally rotates the shoulder detecting the presence of palpable crepitus. The test was considered positive if resulted in palpable crepitus.[15]
Medical Management[edit | edit source]
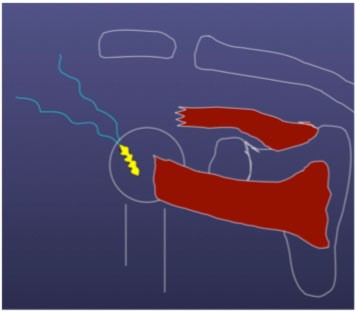
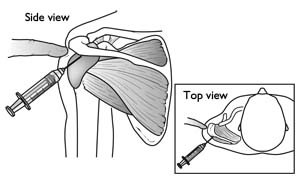
This consists of NSAID’s like ibuprofen, injections with corticosteroids and a surgical treatment. The corticosteroid injections cannot heal the tear but in some cases it can make the tear painless for a period of time in which the patient is capable of undergoing physical therapy more easily. However the tendon tissue can be weakened by these injections which would have an adverse effect on the outcome of a possible surgery, therefore one should not get more than 2 injections.[16] When an injection is chosen it will be placed in the sub-acromial space as seen below.
Bjorkenheim J.M. et al. Surgical repair of the rotator cuff and surrounding tissues. Factors influencing the results
These treatments are conservative medical treatments, if these and physical therapy (see below) don’t work the patient will have to undergo surgery.
The operative treatment is done mostly arthroscopically which is less invasive (than open/mini-open surgery) and leaves only a few small scars. Being less invasive the patients need to use less painkillers and will be able to start rehabilitation sooner. With time and development of better techniques the arthroscopic approach of rotator cuff tendon repair now even has a higher(20%) long term success rate. This was measured with the American Shoulder and Elbow Surgeons scores an reoccurrence of the supraspinatus tears.[17]
Depending on the severity of the tear (partial/complete) a different approach will be used.
If there is just a partial repair necessary the tendon and surrounding bone will be smoothed to avoid further damage and therefor allowing the tendon to heal mostly on its own.[18]In case of a complete tear in the middle of the tendon the surgeon will have to suture the two parts of the tendon back together. When the tear has occurred close or on its point of attachment on the head of the humerus another approach will be taken. This will be the case most of the times. The surgeon will attach the tendon back to its original place by way of an anchor(sometimes two). This anchor actually consists of a small screw that is bored into the head of the humerus with on the back surgical wires with witch to hold the tendon in place.[19]
Physical Therapy Management[edit | edit source]
There are more opnions about what is the right management. It depends of how sincere the tear is. Most of the time a combination of surgery and physicacal therapy is recommend.
In case of a complete tear of the supraspinatus muscle, significant pain and dysfuction after six months of treatment or repeated dislocations surgery will be preferred as treatment. However if it is only a partial tear in most cases a conservative treatment will reduce pain(2-6weeks) and over time even allow the patient to regain function (up to three months).[20] (LoE 5) The reduced pain is not just the direct effect of the pain reducing abilities of NSAID’s. The long term effects will mostly be attributable to a well preformed physical therapy. This will consist of different parts: reduce pain, manipulate blood flow (control inflammation and speed up healing), increase range of motion, increase control of muscles and their strength. Massage can be used to reduce pain, cryotherapy is useful to reduce pain, but only in the first 48 hours after injury. Corticosteroid injection may be useful to reduce pain as well, but only works on short term.
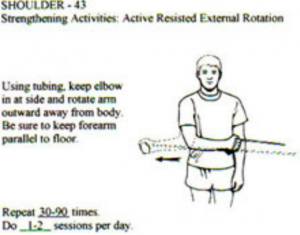
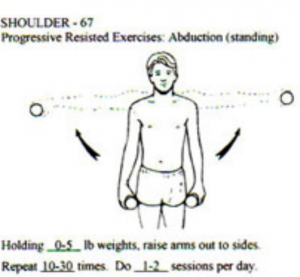
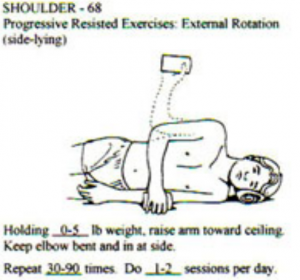
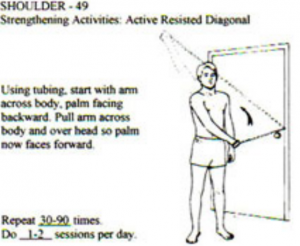
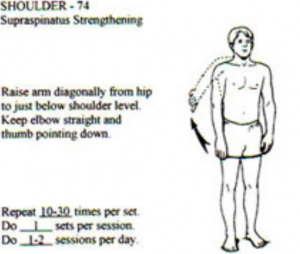
To increase range of motion one can use stretching exercises of the ruptured muscle (not to soon in recovery since premature stretching might aggravate the injury)(see below), passive- and active range of motion exercises such as pendulum exercises and symptom limited active-assisted range of motion exercises(see below). To increase control and strength the patient will also be prescribed strengthening exercises for the rotator cuff specifically the functions of the supraspinatus muscle (abduction and exorotation) explain SS and external rotation[13](LoE 5) [21] (LoE 1B) (see below for a few examples).
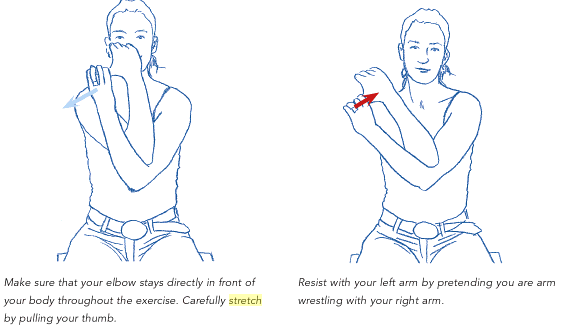
Kristian Berg. Prescriptive stretching; Human Kinetics [22]
Kristian Berg. Prescriptive stretching; Human Kinetics [22]
Dr. Romanski C., Schuldt J. Conservative Treatment of Rotator Cuff Injuries to Avoid Surgical Repair.[20] (LoE 5)
Home exercises consisting of stretching and strengthening exercises prove to be effective, no matter what type of injury (partial defects, full thickness tears of the supraspinatus tendon or massive rotator cuff defects). Patients with rotator cuff defects do benefit from simple home exercises independent from the size of the defect. There is an improvement in range of motion and a downward trend for impingement[23](LoE 2B)
Stretching[edit | edit source]
- Pendulum exercise: lean forward and place one hand on a counter or table for support. The other arm hang freely. Gently swing your arm forward and back. Repeat the exercise moving the arm side-to-side, repeat again in a circular motion. Do not round the back or lock the knees. 2 sets of 10 a day, 5-6days/week.[24] (LoE 5)
- Crossover arm stretch: relax the shoulder and gently pull one arm across your chest as far as possible (adduction of the upper arm) During the stretching of 12 seconds the shoulder is held in active depression. Do not pull or put pressure on you elbow. You move the arm until you feel the stretch the most, this position (around the horizontal position) is held for 12 seconds, 5 times a day; 5-6days/week.[25] (LoE 1A) Performed in a corner or door jamb. Each stretch should be held for 30 seconds and repeat 5 times, with 10 second rest between each stretch.[25] (LoE 1A)
Strengthening[edit | edit source]
- Prone Horizontal Abduction: Lie on stomach with arm hanging over side of table and the thumb facing forward. Slowly raise arm straight out to the side and stop when arm is parallel to the body (going higher can cause excessive strain to the front of the shoulder).[26] (LoE 5)
- Prone Row with External Rotation: Begin in the same position as above, except rotate your hand so the thumb is facing towards the body. Perform a rowing motion with the elbow in the same plane as the shoulder, and stop when the elbow is even with the shoulder. After achieving this position, rotate the arm upwards until the forearm is just below parallel with the body. Next, rotate the forearm back down to the previous position, and then lower the arm back down to the starting position.[26] (LoE 5)
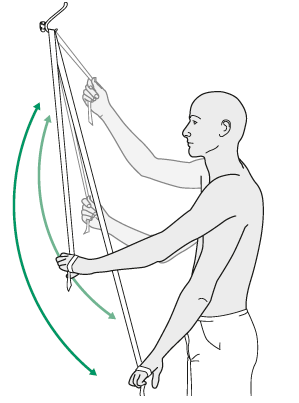
- Horizontal Abduction with Thera-tubing
Stand facing toward the attachment site of the tubing (attached to the door or wall at the height of the chest), with the arm extended straight out in front of you. Slowly pull arm backwards and out to the side, keeping the arm at shoulder height. As you perform this motion, try to pinch the shoulder blade backwards/inwards.[26] (LoE 5)
Key Research[edit | edit source]
- Kuhn JE, Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Sug. 2009 Jan-Feb; 18(1):138-60.
- Orthop J. Rotator cuff tear: physical examination and conservative treatment (2013) Department of Orthopaedic Surgery, Tohoku University, 18, 197–204.
- Hughers PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008; 54(3):159-70.
- Franchigoni F. et al, Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). Journal of Orthopaedic & sports physical therapy. 2014, 44(1):30-39.
Resources[edit | edit source]
- Hughers PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008; 54(3):159-70. (LoE 1A)
- Medscape , Supraspinatus tendonitis differential diagnoses, http://emedicine.medscape.com/article/93095-differential ( Accessed on October 20 , 2015)
- Eiji Itoi. Rotator cuff tear: phyical examination and conservative treatment. J of Orthopaedic Science. March 2013: 8(2):197-204. Level of Evidence: 2B
- Medscape , Rotator cuff injuries clinical presentation. http://emedicine.medscape.com/article/827841-clinical ( Accessed on April 21 , 2014 ).
- Medscape , Rotator cuff injury clinical presentation. http://emedicine.medscape.com/article/92814-clinical (Accessed on March 25 , 2015 ).
- Sportsinjuryclinic , Rotator cuff tear. http://www.sportsinjuryclinic.net/sport-injuries/shoulder-pain/rotator-cuff-strain.
Clinical Bottom Line[edit | edit source]
Timing of Surgical Intervention: Evidence is too limited to draw conclusions about the comparative effectiveness of early surgical repair when compared to late surgical repair following nonoperative interventions.
Operative vs. Nonoperative Interventions*: Significant improvements were seen in all study groups regardless of the intervention. Although there was a trend for better outcomes with surgery, results were too limited to permit conclusions.
Nonoperative Interventions: The variety of interventions and the low quality of studies precludes any conclusions about the most effective nonoperative patient-management strategy.
Operative Interventions: Functional outcomes were similar for open vs. mini-open repair; mini-open vs. arthroscopic repair; open or mini-open vs. arthroscopic repair; and arthroscopic repair with or without acromioplasty. However, exceptions were:
Mini-open vs. open repair: Patients may return to work or sports approximately 1 month earlier if they have a mini-open repair (p < 0.00001).
Open repair vs. open or arthroscopic debridement: Open repair results in greater improvement in functional outcomes than does debridement (p ≤ 0.03).
Postoperative Rehabilitation: Overall, patients improved over the course of postoperative followup. However, there was not enough quality evidence to determine the optimal postoperative rehabilitation protocol.
Adverse Events: In general, complication rates were low for clinically important complications such as re-tears, stiffness, infection, and neurological injury.
Nonoperative comparators included shock-wave therapy, steroid injection, physical therapy, modified activity, oral medication, passive stretching, and strengthening. Operative interventions included mini-open, open, arthroscopic debridement, or open repair with acromioplasty.
Nonoperative interventions included stretching and strengthening, steroid injections, and oral medications.
Postoperative rehabilitation interventions usually included an unspecified physical therapy component; however, the comparisons varied across studies.
Recent Related Research ( from Pubmed )[edit | edit source]
- http://www.ncbi.nlm.nih.gov/pubmed/23306597
- http://www.ncbi.nlm.nih.gov/pubmed/18721119
- http://www.ncbi.nlm.nih.gov/pubmed/25937713
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Orthoinfo American Academy of Orthopedic Surgeons, Rotator cuff tears, http://orthoinfo.aaos.org/topic.cfm?topic=a00064 (accessed on April 29 2015). Level of Evidence: 5
- ↑ Francesco Benazzo, Matteo Marullo, Luigi Pietrobono, Supraspinatus rupture at the musculotendinous junction in a young woman: a case report, J Orthopaed Traumatol (2014) 15:231–234
- ↑ Michael Schünke, Erik Schulte, Udo Schumacher, Markus Voll, Karl Wesker, 2010. Prometheus: Algemene anatomie en bewegingsapparaat, 600p
- ↑ Rotator Cuff Tear, Physioworks, http://physioworks.com.au/injuries-conditions-1/rotator-cuff-tears,
- ↑ Tashjian RZ. Epidemiology , natural history , and indications for treatment of rotator cuff tears . Clinics in Sports Medicine. 2012 October, 31(4):589-604
- ↑ Yamamoto A , Takagishi K , Osawa T , Yanagawa T , Nakajima D , Shitara H , Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population . Journal of shoulder and elbow surgery. 2010 January , 19(1):116-20.
- ↑ Mayoclinic , Rotator cuff injury. http://www.mayoclinic.org/diseases-conditions/rotator-cuff-injury/symptoms-causes/dxc-20126923
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 8.15 8.16 Medscape , Supraspinatus tendonitis differential diagnoses, http://emedicine.medscape.com/article/93095-differential ( Accessed on March 20 , 2015 )
- ↑ 9.0 9.1 9.2 9.3 Medscape , Rotator cuff injury differential diagnoses, http://emedicine.medscape.com/article/92814-differential, (Accessed on March 25 , 2015 )
- ↑ 10.0 10.1 Seida JC, Schouten JR, Mousavi SS, et al. AHRQ Comparative Effectiveness Reviews. Rockville MD 2010 July, and internetlink: http://www.ncbi.nlm.nih.gov/books/NBK47309/table/ch1.t1/?report=objectonly (accessed on April 20, 2015)
- ↑ Franchigoni F. et al, Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). Journal of Orthopaedic & sports physical therapy. 2014, 44(1):30-39
- ↑ Leggin B.J. et al. The Penn Shoulder Score: Reliability and Validity. (2006) from: http://www.jospt.org/issues/articleID.1021,type.14/article_detail.asp
- ↑ 13.0 13.1 Orthop J. Rotator cuff tear: physical examination and conservative treatment (2013) Department of Orthopaedic Surgery, Tohoku University, 18, 197–204. (level of evidence 5)
- ↑ 14.0 14.1 14.2 Hughers PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008; 54(3):159-70.
- ↑ Seif Sawalha, Jochen Fischer. The accuracy of “subacromial grind test” in diagnosis of supraspinatus rotator cuff tears. Int J Shoulder Surg. 2015 Apr-Jun; 9(2):43-46
- ↑ Bjorkenheim J.M. et al. Surgical repair of the rotator cuff and surrounding tissues. Factors influencing the results. (1988) Clinical Orthopaedic Relations, 236.
- ↑ Millar N.L. et al. Open versus two forms of arthroscopic rotator cuff repair. (2009) Clinical Orthopaedics and Related Research, 467, 966-78.
- ↑ American Academy of Orthopedic Surgeons. Rotator Cuff Tears: Surgical Treatment Options (2011)
- ↑ Akpinar S. et al. Prospective evaluation of the functional and anatomical results of arthroscopic repair in small and medium-sized full-thickness tears of the supraspinatus tendon.(2011) Acta Orthop Traumatol Turc 45, 248-253
- ↑ 20.0 20.1 Dr. Romanski C., Schuldt J. Conservative Treatment of Rotator Cuff Injuries to Avoid Surgical Repair. (2009). (level of evidence 5)
- ↑ Tanaka M. et al. Factors related to successful outcome of conservative treatment for rotator cuff tears. (2010) Journal of Medical Sciences, Upsala, 115, 193–200 (level of evidence 1B)
- ↑ 22.0 22.1 Kristian Berg. Prescriptive stretching; Human Kinetics; 2011
- ↑ Heers G. et al. Efficacy of home exercises for symptomatic rotator cuff tears in correlation to the size of the defect. (2005) Klinik für Orthopädie der Universität Regensburg, Bad Abbach. (level of evidence 2B)
- ↑ Dr. Joseph Berman MD, Tag: Supraspinatus tear, http://www.josephbermanmd.com/diagnosis-treatament-of-the-shoulder/rotator-cuff-tear/ (accessed on April 29 2015) (level of evidence 5)
- ↑ 25.0 25.1 Kuhn JE, Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Sug. 2009 Jan-Feb; 18(1):138-60. (level of evidence 1A)
- ↑ 26.0 26.1 26.2 Exercises to Strengthen the Rotator Cuff Muscles in the Shoulder, http://www.physioroom.com/experts/asktheexperts/answers/qa_mb_20050225.php (accessed on June 6) (level of evidence 5)