Straight Leg Raise Test
Background[edit | edit source]
The Straight Leg Raise (SLR) test is commonly used to identify disc pathology or nerve root irritation, as it mechanically stresses lumbosacral nerve roots. It also has specific importance in detecting disc herniation and neural compression.[1] [2][3]It is also classified as a neurodynamic evaluation test as it can detect excessive nerve root tension[4] or compression[5]. This test is attributed to Dr. Charles Laseague, and referred to as Laseagues test. However, it is believed that Dr. Lazar Lazarevic was the first to establish this test[6].
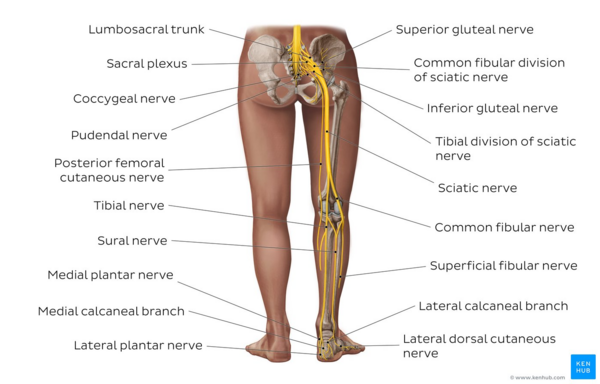
This test places tensile stresses on the sciatic nerve and of traction at the lumbosacral nerve roots primarily from L4 to S2. During the SLR, these nerve roots are pushed anteriorly and inferiorly, pulling the dura mater caudally, laterally and anteriorly. Tension in the sciatic nerve occurs sequentially as it pulls the sciatic foramen, then the sacrum and then the nerves that cross over the pedicles and finally the intervertebral foramen. Pain or tenderness is often localised in the vicinity of the greater sciatic notch. [7][8][9]
Image: Overview of the sciatic nerve and its branches[10]
Clinical Application[edit | edit source]
Most clinical practice guidelines suggest the SLR test as an assessment to identify radicular pain or radiculopathy[11]. However, there is low level evidence that the SLR test can detect radiculopathy [12]. The SLR test is more sensitive than specific, hence useful for ruling out lumbo-sacral radiculopathy [13]. Adding structural differentiation (e.g., neck flexion, ankle dorsiflexion, hip adduction) improves the reliability of the SLR test to at least a moderate level, and is recommended in clinical practice[11].
Technique[edit | edit source]
The classic straight leg raise is performed passively. Each leg is tested individually with the unaffected leg being tested first.[2] When performing the SLR test, the patient is positioned in supine without a pillow under their head, the clinician stands at the tested side with their distal hand around the patient's heel and proximal hand on patient's distal thigh(anterior) to maintain knee extension. The clinician lifts the patient's leg by the posterior ankle while keeping the knee in a fully extended position. The clinician continues to lift the patient's leg slowly through flexing at the hip, until the patient's symptoms are replicated, or they experience tightness in the back or posterior thigh.[2][14]
When pain occurs, examiner ceases hip flexion and notes the ROM and the area of pain[5]. The ROM for the affected leg can be compared to the unaffected leg and used as an outcome measure. It should however be noted that the inter-rater reliability for this is low[11].
Straight Leg Raise Test video provided by Clinically Relevant
Interpretation & Reasoning[edit | edit source]
- A true positive SLR test should include[5]:
- Radicular leg pain (symptoms below the knee).
- Pain occurs when hip is flexed at 30 and 60 or 70 degrees from horizontal. Neurological pain which is reproduced in the leg and lower back between 30-70 degrees of hip flexion is suggestive of lumbar disc herniation at the L4-S1 nerve roots[15]
- Pain at greater than 70 degrees of hip flexion might indicate tightness of the hamstrings, gluteus maximus, or hip capsule, or pathology of the hip or sacroiliac joints[5].
- If symptoms are primarily back pain, it is most likely the result of a disc herniation applying pressure on the anterior theca of the spinal cord, or the pathology causing the pressure is more central. "Back pain only" patients who have a disc prolapse have smaller, more central prolapses.[2]
- If pain is primarily in the leg, it is more likely that the pathology causing the pressure on neurological tissue(s) is more lateral.[2]
- Disc herniations or pathology causing pressure between the two extremes are more likely to cause pain in both areas.[2]
- Nerve root irritation such as facet joint cysts or hypertrophy can also cause the SLR test to be positive[6]. Other causes of a positive SLR test include intraspinal tumor and inflammatory radiculopathy[16].
Sensitising Maneuvers[edit | edit source]
Sensitising maneuvers are performed to confirm neural tissue as the source of patient's symptoms, by increasing load on neural tissue without changing load on non-neural tissue. After the elicitation of symptoms, the examiner can slowly and carefully lower the leg until the patient no longer feels pain or tightness. Next, either the patient is asked to bring his or her chin to the chest, or the examiner may passively dorsiflex the patient's foot, or both actions may be done simultaneously; however, foot dorsiflexion is most commonly performed first. Both maneuvers are considered to be provocative or sensitising tests for neurological tissue.
Pain that increases with neck flexion or foot dorsiflexion or both indicates stretching of the dura mater of the spinal cord or a lesion within the spinal cord (e.g. disc herniation, tumor, or meningitis) [2]
Pain that does not increase with neck flexion may indicate a lesion in the hamstring area (tight hamstrings) or in the lumbosacral or sacro-iliac joint.
- Inclusion of neck flexion in the SLR is documented as Hyndman's sign, Brudzinski's Sign, Linder's Sign, or the Soto-Hall test.
- Inclusion of ankle dorsiflexion in the SLR is documented as Lasegue's test or Bragard's test.
- Inclusion of great toe extension in the SLR (instead of ankle dorsiflexion) is documented as Sicard's Test.
Modifications[edit | edit source]
Modifications to the Straight Leg Raise test can be used to stress different peripheral nerves to a greater degree; these are referred to as SLR tests with a particular nerve bias.
| SLR (BASIC) | SLR2 | SLR3 | SLR4 |
CROSS LEG SLR 5 | |
|---|---|---|---|---|---|
| HIP | Flexion and adduction | Flexion | Flexion | Flexion and medial Rotation | Flexion |
| KNEE | Extension | Extension | Extension | Extension | Extension |
| ANKLE | Dorsiflexion | Dorsiflexion | Dorsiflexion | Plantar flexion | Dorsiflexion |
| FOOT | ------ | Eversion | Inversion | Inversion | ------- |
| TOES | ------ | Extension | ----- | ------ | ------ |
| NERVE BIAS | Sciatic Nerve and Tibial Nerve | Tibial Nerve | Sural Nerve | Common Peroneal Nerve | Nerve Root (Disc Prolapse) |
SLR for hamstrings length assessments:[edit | edit source]
Subject is positioned in supine. Therapist grasps the ankle and lifts the leg straight up, using the other hand to stabilise the same side anterior superior iliac spine. If the leg cannot be raised beyond 80 degrees, the hamstrings are considered tight.
Evidence[edit | edit source]
- A cross-sectional study by Boyd and Villa (2012) [18]examined normal asymmetries between limbs in healthy, asymptomatic individuals during SLR testing and the relationship of various demographic characteristics. The authors concluded that overall range of motion during SLR was related to sex, weight, BMI and activity level, which is likely reflected in the high variability documented. We can be 95% confident that inter-limb differences during SLR neurodynamic testing fall below 11 degrees in 90% of the general population of healthy individuals. In addition, inter-limb differences were not affected by demographic factors and thus may be a more valuable comparison for test interpretation.
- Rabin et al. has shown sensitivity of the SLR test to be .67[19], while Deville et al. found the specificity to be .26 [20].
- A systematic review of the clinical utility of SLR by Scaia V, Baxter D and Cook C (2012) investigated the diagnostic accuracy of a finding of pain during the straight leg raise test for lumbar disc herniation, lumbar radiculopathy, and/or sciatica. The authors concluded that variability in reference standard may partly explain the inconsistencies in the diagnostic accuracy findings. Further, pain that is not specific to lumbar radiculopathy, such as that associated with hamstring tightness, may also lead to false positives for the SLR; and may inflate the sensitivity of the test.
- Diagnostic Test accuracy review (Cochrane Meta analysis) [21] assessed the performance of tests performed during physical examination (alone or in combination) to identify radiculopathy due to lower lumbar disc herniation in patients with low-back pain and sciatica. The review included 16 cohort studies (median N = 126, range 71 to 2504) and three case control studies (38 to100 cases). Only one study was carried out in a primary care population. Most studies assessed the Straight Leg Raising (SLR) test. In surgical populations, characterized by a high prevalence of disc herniation (58% to 98%), the SLR showed high sensitivity (pooled estimate 0.92, 95% CI: 0.87 to 0.95) with widely varying specificity (0.10 to 1.00, pooled estimate 0.28, 95% CI: 0.18 to 0.40). Results of studies using imaging showed more heterogeneity and poorer sensitivity. The crossed SLR showed high specificity (pooled estimate 0.90, 95% CI: 0.85 to 0.94) with consistently low sensitivity (pooled estimate 0.28, 95% CI: 0.22 to 0.35). Combining positive test results increased the specificity of physical tests, but few studies presented data on test combinations. The authors of the meta analysis conclude that when used in isolation, current evidence indicates poor diagnostic performance of most physical tests used to identify lumbar disc herniation. However, most findings arise from surgical populations and may not apply to primary care or non-selected populations. Better performance may be obtained when tests are combined.
Resources[edit | edit source]
This 14 minute video is a good summary of the sciatic nerves and its branches.[22]
References[edit | edit source]
- ↑ Pesonen J, Shacklock M, Rantanen P, Mäki J, Karttunen L, Kankaanpää M, Airaksinen O, Rade M. Extending the straight leg raise test for improved clinical evaluation of sciatica: reliability of hip internal rotation or ankle dorsiflexion. BMC Musculoskeletal Disorders. 2021 Dec;22(1):1-8.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 David J. Magee;Orthopaedic Physical Assessment; Chapter 9-Lumbar Spine;Fifth Edition: Pg 558-564.
- ↑ Dutton, M. (2008). Orthopaedic: Examination, evaluation, and intervention (2nd ed.). New York: The McGraw-Hill Companies, Inc.
- ↑ Kamath SU, Kamath SS. Lasègue's Sign. J Clin Diagn Res. 2017;11(5):RG01-RG02.
- ↑ 5.0 5.1 5.2 5.3 Das JM, Nadi M. Lasegue Sign. StatPearls [Internet]. 2020 May 24.
- ↑ 6.0 6.1 Camino GO, Piuzzi NS. Straight Leg Raise Test [Internet]. Nih.gov. StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539717/
- ↑ Shah S,Wang TW. Piriformis syndrome. eMedicine specialities :Sports medicine : hip 2009fckLRhttp://emedicine.medscape.com/article/87545-overview
- ↑ Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve Jul 2009 ; 40(1) : 10-18
- ↑ Lori A, Boyajian- O’ Neill et al. Diagnosis and Management of Piriformis syndrome : an osteopathic approach. The journal of the American and osteopathic association Nov 2008; 108(11): 657-664.
- ↑ Overview of the sciatic nerve and its branches image - © Kenhub https://www.kenhub.com/en/library/anatomy/the-sciatic-nerve
- ↑ 11.0 11.1 11.2 Nee RJ, Coppieters MW, Boyd BS. Reliability of the straight leg raise test for suspected lumbar radicular pain: A systematic review with meta-analysis. Musculoskeletal science & practice. 2022;59:102529–102529. https://link.springer.com/article/10.1007/s00586-018-5673-2?utm_source=getftr&utm_medium=getftr&utm_campaign=getftr_pilot
- ↑ Mistry J, Heneghan NR, Noblet T, Falla D, Rushton A. Diagnostic utility of patient history, clinical examination and screening tool data to identify neuropathic pain in low back related leg pain: A systematic review and narrative synthesis. BMC musculoskeletal disorders. 2020;21(1):532–532. https://link.springer.com/content/pdf/10.1186/s12891-020-03436-6.pdf
- ↑ Tawa N, Rhoda A, Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: A systematic literature review. BMC musculoskeletal disorders. 2017;18(1):93–93. http://link.springer.com/content/pdf/10.1186/s12891-016-1383-2.pdf
- ↑ Surendra UK, Shaila SK. Lasegue sign. Journal of Clinical and Diagnostic Research. 2017, VOL-11(5): RG01-RG02.72(12):959-66.
- ↑ Ropper AH, Zafonte RD. Sciatica. The New England journal of medicine. 2015;372(13):1240–8. https://www.nejm.org/doi/10.1056/NEJMra1410151
- ↑ M; MDJN. Lasegue sign [Internet]. National Center for Biotechnology Information. U.S. National Library of Medicine; 2022 [cited 2022Nov30]. Available from: https://pubmed.ncbi.nlm.nih.gov/31424883/
- ↑ Butler DA: Mobilisation of the nervous system, Melbourne,1991,Churchill Livingstone.
- ↑ Boyd BS, Villa PS. Normal inter-limb differences during the straight leg raise neurodynamic test: a cross sectional study. BMC Musculoskeletal Disorders. 2012;13:245. doi:10.1186/1471-2474-13-245.
- ↑ Rabin A, Gerszten PC, Karausky P, et al. The Sensitivity of the Seated Straight-Leg Raise Test Compared With the Supine Straight-Leg Raise Test in Patients Presenting With Magnetic Resonance Imaging Evidence of Lumbar Nerve Root Compression. Arch Phys Med Rehabil. 2007;(88):840-843.
- ↑ Deville WL, van der Windt DA, Dzaferagic A, et al. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine 2000;25:1140-7.
- ↑ Daniëlle AWM van der Windt,Emmanuel Simons, Ingrid I Riphagen,Carlo Ammendolia, Arianne P Verhagen,Mark Laslett,Walter Devillé,Rick A Deyo,Lex M Bouter,Henrica CW de Vet,Bert Aertgeerts ;Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain;Diagnostic Test Accuracy Review;Published Online: 17 FEB 2010;Assessed as up-to-date: 28 OCT 2008fckLRDOI: 10.1002/14651858.CD007431.pub2
- ↑ Sciatic nerve and its branches video - © Kenhub https://www.kenhub.com/en/library/anatomy/the-sciatic-nerve