Spinal Osteoarthritis
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson and Cindy John-Chu
Introduction[edit | edit source]
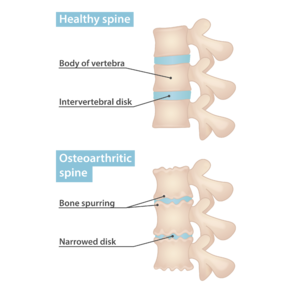
Osteoarthritis (OA) of the vertebral column is common and usually merely referred to as spinal "degenerative change". Complications such as spinal stenosis are important to recognise[1].
- Degeneration causes vertebral osteophytes, facet joint osteoarthritis (FJ OA), and disc space narrowing. FJ OA and degenerative disc disease are both thought to be common causes of back and neck pain, which in turn have an enormous impact on the health-care systems and economies of developed countries[2][3]
- Osteoarthritis is more likely to affect weight-bearing joints, including the joints of the spinal column.
- The intervertebral disc and FJs are not identical, but their composition and process of degeneration are remarkably similar. Intervertebral disc degeneration and FJ OA both follow a vicious cycle of degeneration, eventually resulting in destruction of the intervertebral disc and articular joint, respectively[4].
Anatomy and Pathophysiology[edit | edit source]
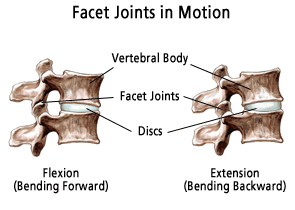
The spinal cord is composed of a three-joint complex (ie a spinal motion segment) consisting of of two facet joints (zygapophyseal joints), and one intervertebral disc, all of which are potential origins for back pain.[3]
As patients age, the functional integrity of their spines deteriorates and predisposes patients to degenerative changes as a result of the alterations in load-bearing forces. This cascade begins with age-related intervertebral disc degeneration.
- In a healthy spine, the facet joints carry approximately 33% of the load.
- As facet joint and intervertebral disc degeneration develop, this load-bearing increases to 70%.
As the posterior spine bears an increased load, the subchondral bone density increases along with osteophyte formation. This leads to synovial hypertrophy, cartilage necrosis, ulceration, fibrillation, eburnation, instability, and bony overgrowth (can contribute to spinal stenosis).
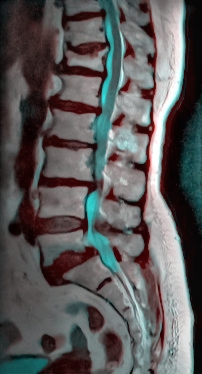
- Image 2: Lumbar Spine MRI, T12 Compression fracture, L5-S1 spondylolisthesis, OA at other levels.[3]
Presentation[edit | edit source]
The typical presentation of patients with symptomatic osteoarthritis of the spine is pain, stiffness, and motion restriction, which is commonly accompanied by referred pain. The distribution of a patient's pain depends on the location of the pathology.
- The clinical syndrome related to painful facet joints is usually localized neck pain or back pain with some degree of radiation into the upper or lower limbs[2].
- Mid-cervical and lower-cervical facet joints refer pain to the posterior scapular and shoulder regions. The upper cervical complex produces pain in the occipital region and is often associated with headaches.
- The lumbar spine provides pain located in the buttock and thigh region. Lumbar spine osteoarthritis can be associated with radicular pain above the knee.
- If radicular symptoms move below the knee, nerve root compression or irritation is likely. Nerve root compression is associated with motor, sensory, and reflex deficits.
- Clinically, the prevalence of facet-mediated pain increases with increasing age, which suggests FJ OA might have an important role in the ageing population with spinal pain.[2]
Assessment[edit | edit source]
See Lumbar Thoracic and Cervical Examination links.
Management[edit | edit source]
Treatment of spine osteoarthritis includes conservative management, pharmacological interventions, and invasive procedures. The various treatment modalities get determined by the etiology of the osteoarthritis, duration of the patient's pain, neurological symptoms, and physical exam findings.
The American College of Physicians Clinical Guidelines Committee (ACPCGC) recommends:
- Superficial heat, massage, acupuncture, or spinal manipulation as first-line therapy for acute or subacute non-radicular low back pain. Acute back pain lasts under four weeks, subacute four to 12 weeks, and chronic back pain longer than 12 weeks in duration.
- Conservative management should be the initial treatment for chronic, mechanical low back pain.
Other conservative treatments include:
- Diet and nutritional supplements also play a role in managing osteoarthritis and should be combined with exercise therapy.
- Obesity is a risk factor for osteoarthritis. For every five kilograms of weight gain, there is a 36 percent increased risk for developing osteoarthritis.
- Patients with chronic low back pain associated with osteoarthritis should be screened for depression and treated appropriately with cognitive behavioral therapy or antidepressants
- Acetaminophen is a first-line treatment for low back pain. NSAIDs had small to moderate effects on pain and minimal impact on function NSAIDs are first-line pharmacological therapy for chronic low back pain. If ineffective, tramadol or duloxetine are second-line therapy. Skeletal muscle relaxants are adjunct treatments for acute and subacute low back pain.[3]
Physiotherapy[edit | edit source]
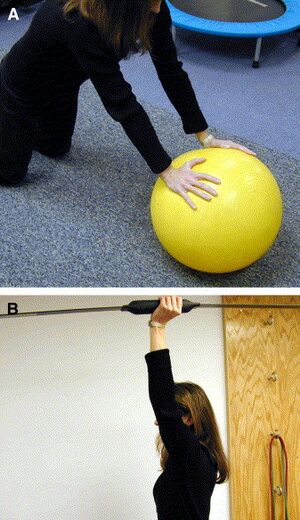
- One of the most beneficial traditional therapy techniques is exercise therapy. Weight bearing exercises are of the most significant benefit in increasing lumbar spine bone mineral density.
- A home-based exercise program (highly effective option in patients with both acute and chronic spinal pain). Create patient-specific treatment regimens and provide supervised exercise sessions to ensure adequate exercise intensity and alleviate the fear associated with mobility.
- Core stability exercises to reduce stress on joints of spine. Image 5: Core Plank Exercise
- Aerobics and Yoga
- Weight-bearing and resistance exercise.
- Abdominal muscle strengthening
- Yoga has also proven to be an effective treatment modality for chronic low back pain.
- Spinal mobilisation and manipulation is an option for those with acute and chronic back pain.
- Traction therapy and transcutaneous electrical nerve stimulation (TENS unit) are adjunctive treatment options. Evidence is lacking to support their efficacy. However, one meta-analysis demonstrated that TENS was useful in pain reduction for patients with chronic low back pain if treated for less than five weeks. This treatment modality may reduce the number and amount of pain medications needed for pain control.
Note: The combination of exercise and psychological treatment may be of greater efficacy for chronic low back pain than any single intervention[3]
Invasive Techniques[edit | edit source]
Invasive techniques in treating spine osteoarthritis include
- Facet joint injections, epidural injections, acupuncture, medial branch nerve ablation, and surgical intervention. Some studies suggest that epidural injections show short-term improvements in pain and quality of life for up to two weeks.
- Surgical intervention is reserved for clearly identifiable structural pathologies that are amenable to surgical intervention, neurological symptoms secondary to the spinal cord or nerve root compression, or when non-operative intervention has failed. Surgical intervention is recommended for cauda equina syndrome and spinal stenosis with progressive or severe neurological deficits.
References[edit | edit source]
- ↑ Radiopedia Spinal OA Available: https://radiopaedia.org/articles/osteoarthritis-of-the-vertebral-column
- ↑ 2.0 2.1 2.2 Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nature Reviews Rheumatology. 2013 Apr;9(4):216-24.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4012322/(accessed 12.6.2021)
- ↑ 3.0 3.1 3.2 3.3 3.4 Lindsey T, Dydyk AM. Spinal osteoarthritis. StatPearls [Internet]. 2020 Jan 7. Available: https://www.ncbi.nlm.nih.gov/books/NBK553190/ (accessed 11.6.2021)
- ↑ Rustenburg CM, Emanuel KS, Peeters M, Lems WF, Vergroesen PP, Smit TH. Osteoarthritis and intervertebral disc degeneration: Quite different, quite similar. JOR spine. 2018 Dec;1(4):e1033.Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6686805/ (accessed 12.6.2021)