Sleep Apnea
Original Editors - Ylice Bridges and Irena Tran
Top Contributors - Irena Tran, Ylice Bridges, Lucinda hampton, Venugopal Pawar, Kim Jackson, 127.0.0.1, Elaine Lonnemann, Admin, WikiSysop, Adam Vallely Farrell and Lilian Ashraf
Definition/Description[edit | edit source]
Sleep apnea is a disorder in which breathing is interrupted or paused during sleep. The pauses in breathing can last a few seconds to minutes and are long enough to:
- Disrupt sleep
- Decrease level of oxygen in the blood
- Increase level of carbon dioxide in the blood
These breathing interruptions can occur more than 30 times an hour and significantly impair the quality of sleep. Because of this, sleep apnea is a leading cause of excessive daytime sleepiness.[1]
There are three types of sleep apnea: central, obstructive and mixed. Obstructive sleep apnea is the most common and the main focus of this article.
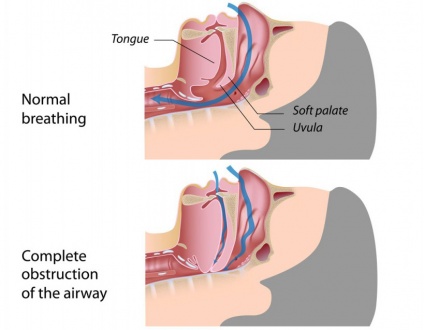
Obstructive sleep apnea (OSA) is caused by repeated partial or complete obstruction of the upper airway that diminishes or stops breathing.
Central sleep apnea occurs when the brain is less sensitive to changes in carbon dioxide levels in the blood and fails to send signals to the respiratory muscles to breathe deeper.
Mixed sleep apnea is a combination of both obstructive and central sleep apnea episodes.[1]
Prevalence[edit | edit source]
OSA is commonly seen in males; they have a 2-3x increased risk of developing OSA as compared to women. A women's risk of developing OSA increases during pregnancy.[2] [3] OSA can occur in childhood and adolescence, but typically, it is more common around middle age (40-60 years old). After 65, occurrence of OSA plateaus, and it is unclear whether this is due to increased mortality from OSA or remission of OSA.[2] Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA.[3] There appears to be a 2.5x increased occurrence of OSA among the African-American population versus the Caucasian population.[2] [3] Among other ethnicities, OSA was more prevalent in American Indians, Hispanic adults, and Pacific Islanders when obesity played a large role.[3] Also, OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.[4]
Characteristics/Clinical Presentation[edit | edit source]
Common signs and symptoms of OSA:[5]
Associated Co-morbidities[edit | edit source]
- Hypertension (HTN) *Treatment of OSA has been shown to help decrease HTN, specifically in middle-aged individuals.[6]
- Obesity *Excessive body weight affects breathing capability due to increased adipose around the airway structures.[2] [3]
- Congested Heart Failure (CHF)[4]
- Fatal and Nonfatal Cardiovascular Events[7]
- Type II Diabetes[4]
- Pulmonary Hypertension[4]
- Stroke *OSA may be present prior to CVA as suggested in studies where neurological deficits, excluding OSA, recovered[4] [7]
- Depression[8]
- Cancer *Especially breast, nasal, and prostate CA[9]
Medications[edit | edit source]
Numerous studies have shown that pharmacological interventions in the treatment and management of OSA are not as effective as the use of PAP, specifically CPAP.[4] [10] [11] Studies have focused on:
- Increasing ventilatory drive (progestogens, theophylline, acetazolamide)
- Increasing upper airway tone (serotonergics, cholinergic)
- Decreasing REM sleep (antidepressants, clonidine)
- Increasing arousal threshold (eszopiclone)
- Increasing cross-sectional area or reducing surface tension of upper airway (topical therapy- fluticasone, lubricant)
These drugs may be useful, but more research is needed to determine long-term viability and overall effectiveness.[12]
Studies have noted positive findings on other medications and its applicability to OSA:
| Drug | Use | Effect | Notes |
|---|---|---|---|
| Qsymia (Phentermine with extended release Topiramate)[10] | Weight loss |
Decreased AHI, decreased weight |
More research needed |
| Modafinil[10] [11] | Wakefulness | Increased daily functioning, relieved daytime sleepiness |
Use as adjunct therapy; long-term cardiovascular effects unclear; more research needed |
| Leukotriene Antagonists[11] |
Allergies | Decreased RDI (respiratory disturbance index), decreased adenoid size *in children | More research needed |
| Donepezil[11] | Alzheimer's | Decreased AHI, improved REM sleep, improved O2 saturation | More research needed |
| Mirtazapine[11] | Antidepressant | Decreased upper airway collapse | May cause weight gain & sedation; more research needed |
| Inhaled corticosteroids[11] | Asthma | Decreased AHI, decreased nasal airway resistance, improved daytime wakefulness | No indication of improved breathing in sleep; not recommended at this time; more research needed |
| Lansoprazole (proton pump inhibitor)[12] |
GI (ex: GERD) | Decreased AHI | No change in O2 saturation or sleep efficiency; more research needed |
Certain medications have been found to worsen OSA and should not be prescribed:
- CNS Depressants (ex: opiates, benzodiazepines, barbiturates)
- Beta Blockers (ex: Propranolol)
- Erectile Dysfunction Medications (ex: Sildenafil)[11]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Individuals suspected of OSA undergo a pretest assessment: a history, a clinical examination, and sleep questionnaires.[13]
- History: possible risk factors, co-morbidities, snoring, and what a normal night of sleep is like to him/her.[14]
- Indices: AHI (apnea-hypopnea index), RDI (respiratory disturbance index)[15]
- Clinical Examination: nose, tonsils, palate, tongue, neck circumference, upper airways.[14] [8] Findings are predominantly inconclusive and requires training for proper assessment.[14]
- Questionnaires: Epworth Sleepiness Score (ESS) for daytime sleepiness; Berlin questionnaire for common OSA risk factors and symptoms.[14]
- Oximetry: analyze oxygen saturation of hemoglobin to help identify individuals unlikely to have OSA.[8]
For the diagnosis of sleep disorders, including OSA, the standard test is Level 1 polysomnography. Individual spends the night in asleep laboratory, where a sleep technician is present, and 7 to 16+ channels are monitored. These channels track the cardiovascular system, respiratory system, and neurologic system. It can also monitor sleep duration, sleep arousals, and sleep stages.[13]
For those with a high probability of moderate to severe OSA, a good diagnostic test is Level 3 portable device (polygraph). Portable monitors are brought into the individual’s home or preferred location. These monitors look at at least 3 channels: oximetry, airflow, and respiratory effort in sleep. It does not record sleep duration, arousals, sleep stages, or non respiratory sleep disorders.[13]
Etiology/Causes[edit | edit source]
Relaxation of the throat and tongue muscles during sleep obstructs the airway and can decrease or stop breathing.
Factors that contribute to airway obstruction are:[15]
- Obesity
- Large neck circumference
- Large tongue or tonsils
- Narrow airway due to bony structures of head and neck
- Taking sedative medication
- Drinking alcohol
- Smoking
- Nasal congestion
Systemic Involvement[edit | edit source]
Cardiovascular System
OSA causes the level of oxygen in the blood to decrease and the level of carbon dioxide to increase. This leads to a sympathetic activity, vasoconstriction and inflammation. In some OSA episodes, blood pressure can rise as high as 240/130 mm Hg[16].
Some complications of the changing hemodynamics are[16]:
- Hypertension
- Heart Failure
- Arrhythmias
- Stroke
- Myocardial Infarction
- Renal Disease
Metabolic Dysfunction
The increased sympathetic activity, increased catecholamines and other metabolic disturbances can lead to[16]:
- Diabetes Mellitus
- Insulin Resistance
- Glucose Intolerance
- Metabolic Syndrome
Psychological Problems
Although the exact relationship between OSA and depression is not yet clearly understood, some studies have shown a decrease in the symptoms of depression after treatment of OSA[8].
Medical Management[edit | edit source]
A variety of methods are utilized to treat individuals with OSA:
- Weight reduction (diet, exercise, medications)[4] [11]
- Sleep positioning (avoid supine with positional devices)[4]
- Pharmacological treatments (topical nasal corticosteroids as an adjunct, refer to Medications for more information)[4]
- Oral applicances (Dental applicances)[4]
- Upper air reconstructive or bypass surgeries[4]
Oral Appliances
- Mandibular repositioning appliances (MRA): holds the mandible in an advanced position
- Tongue retaining devices (TRD): holds the tongue forward
These attempt to avoid blockage of the upper airways while sleeping, and are commonly used for mild to moderate OSA and for those who do not benefit from CPAP.[4]
Positive airway pressure (PAP)
PAP, especially CPAP, is the most common method of treatment for mild, moderate, and severe OSA. PAP provides pneumatic splinting to maintain the opening of the upper airway and effectively decreases AHI (Apnea Hypopnea Index= number of apnea or hypopnea episodes per hour of sleep).[4] [10] Normal AHI is less than 5 per hour.[10] PAP can be provided in several ways: continuous (CPAP, the gold standard), bilevel (BPAP), and autotitrating (APAP) and via three interfaces: nasal, oral, or nasoral.[4]
Surgical Interventions
These try to improve the airway passages via nasal, oral, oropharyngeal, nasopharyngeal, hypopharyngeal, laryngeal, and global airways. Possible surgeries include:
- Maxillomandibular Advancement (MMA): moves top and lower jaw to increase upper airway[10]
- Uvulopalatopharyngoplasty: removes excess tissue at back of throat (ex: uvula) to increase airway[10]
Surgical procedures are beneficial for those with severely obstructive anatomy and unsuccessful treatments with CPAPs or OAs.[4]
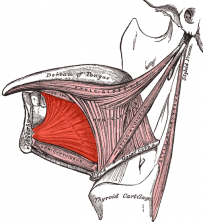
Hypoglossal Nerve-Stimulating System (HGNS)
This treatment, the insertion of the Hypoglossal Nerve-Stimulating System (HGNS), is currently being studied. The Hypoglossal Nerve is the cranial nerve that innervates the tongue, especially the genioglossus muscle, and it plays a large role in maintaining airway patency. The genioglossus "protrudes the tongue, dilates the pharynx, and mitigates airflow obstruction during sleep."[17]
This method has been studied via submental transcutaneous stimulation, direct fine wire stimulation, and direct hypoglossal stimulation.
- Submental transcutaneous stimulation: aroused patients from sleep without clear improvements in the airflow, but may increase lingual muscle tone and improve airway patency.
- Direct fine wire stimulation: produced effective contractions of the genioglossus to improve pharyngeal patency.
- Direct hypoglossal stimulation: implantation of hypoglossal cuff electrodes around the proximal and distal nerve trunk can increase pharyngeal patency and decrease pharyngeal collapsibility without arousing the patients. The development of a fully implantable HGNS is currently being studied.[17]
Physical Therapy Management[edit | edit source]
Although there is little research providing sound evidence based physical therapy interventions for OSA at this time, it often goes undiagnosed providing opportunities for physical therapists to identify, educate and refer patients who present with signs and symptoms of OSA. Undiagnosed OSA is associated with increased risk of hypertension, cardiovascular disease, motor vehicle accidents and reduced quality of life[2].
Physical Therapists can educate patients on OSA:
- Signs and symptoms
- Risk factors
- Associated co-morbidities
- How to get diagnosed/tested
- Risks of undiagnosed OSA
Exercises For Obstructive Sleep Apnea[edit | edit source]
EXERCISES FOR THE TONGUE
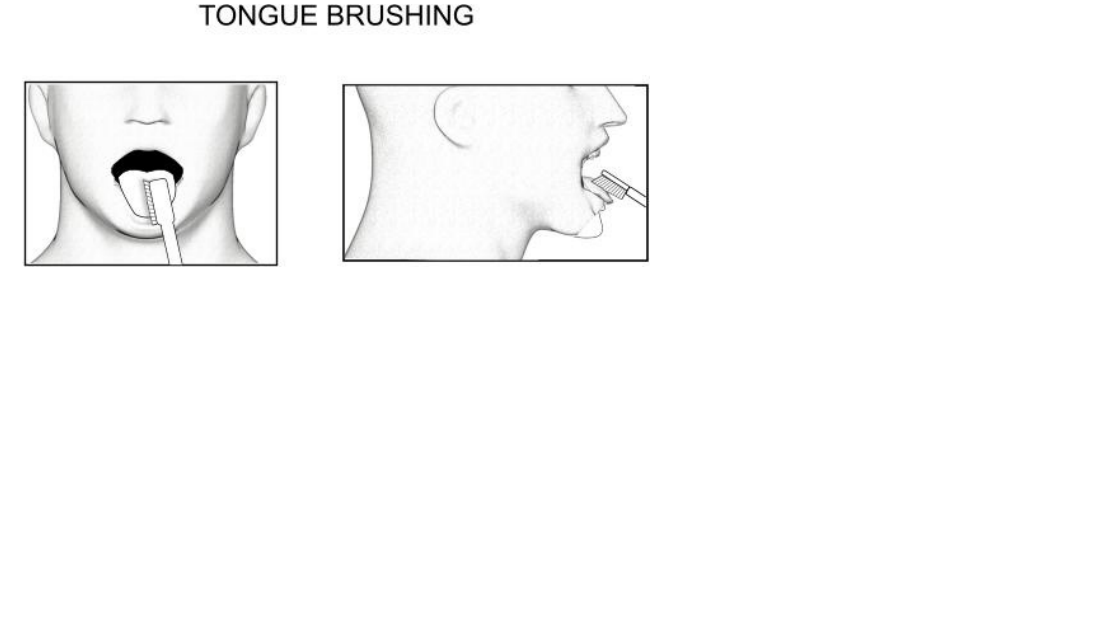
TONGUE BRUSHING
Method:
1. With your toothbrush brush the top and sides of your tongue, while your tongue is sitting on the floor of your mouth.
2. Repeat the individual sections 5 times each.
3. Complete the exercise three times daily.
Purpose – to strengthen the tongue muscles-with the added advantage of maintaining great oral hygiene!
TONGUE SLIDE
Method:
1. Looking straight ahead, position the tip of your tongue against the back of your top, front teeth.
2. Slide your tongue backward.
3. Repeat 10 times.
Purpose – to tone and strengthen the tongue and throat muscles. 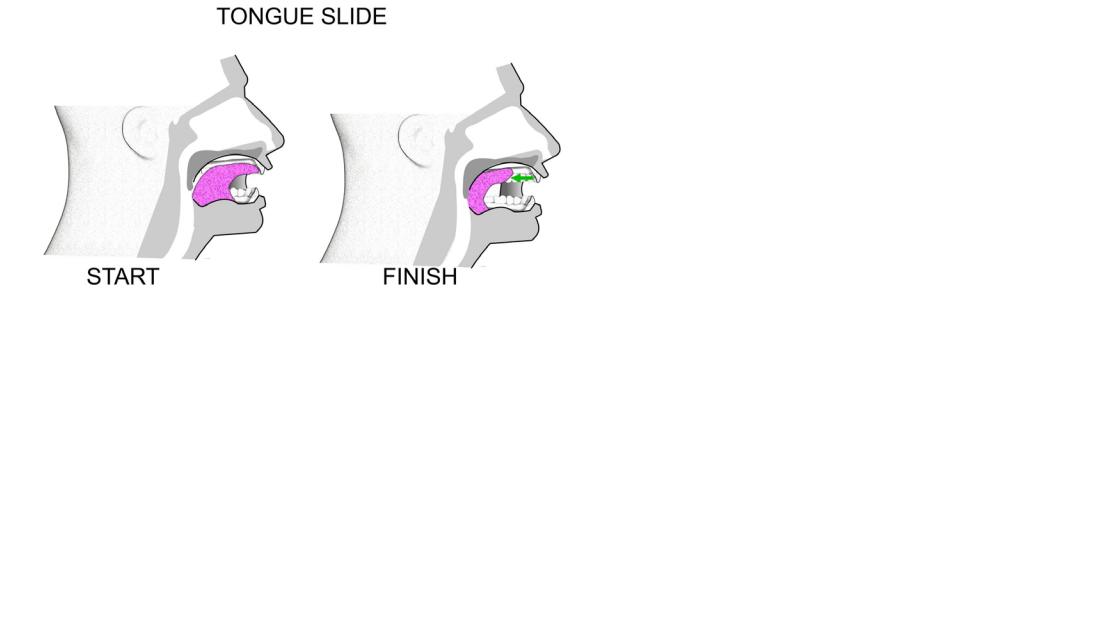 TONGUE FORCES
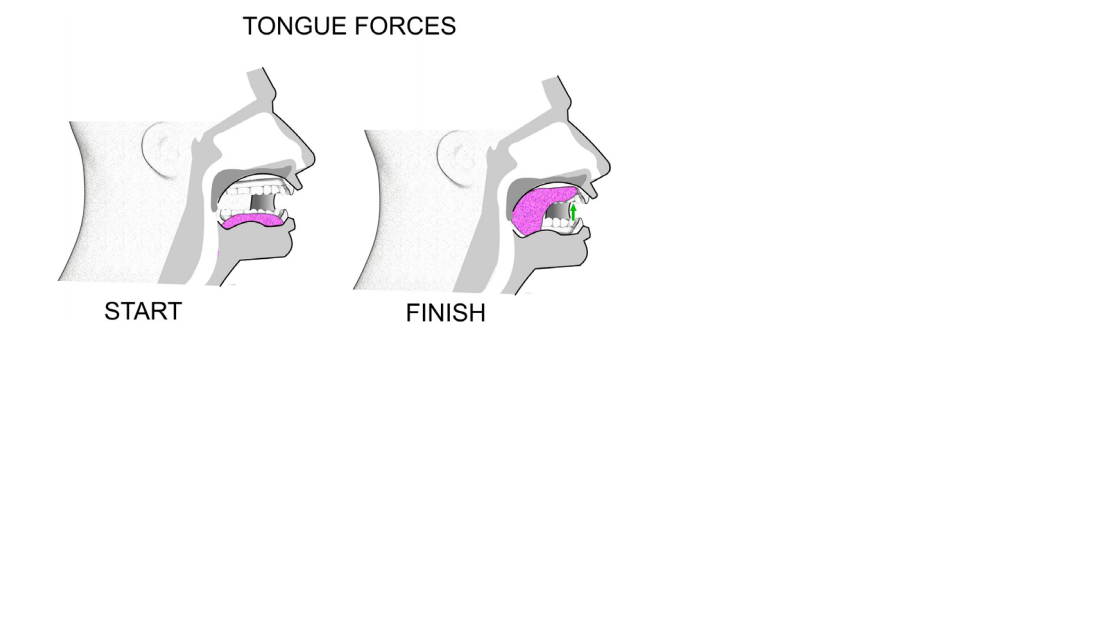
TONGUE FORCES
Method:
1. Forcibly suck your tongue upward until the whole tongue is against your palate.
2. Hold this position for 4 seconds.
3. Repeat 5 times.
Method:
1. Force the back of your tongue downward until the whole tongue is resting on the floor of your mouth.
2. Keep the tip of your tongue touching the back of your lower teeth.
3. Hold for 4 seconds.
4. Repeat 5 times.
Purpose - both of these exercises strengthen the tongue and tone your soft palate.
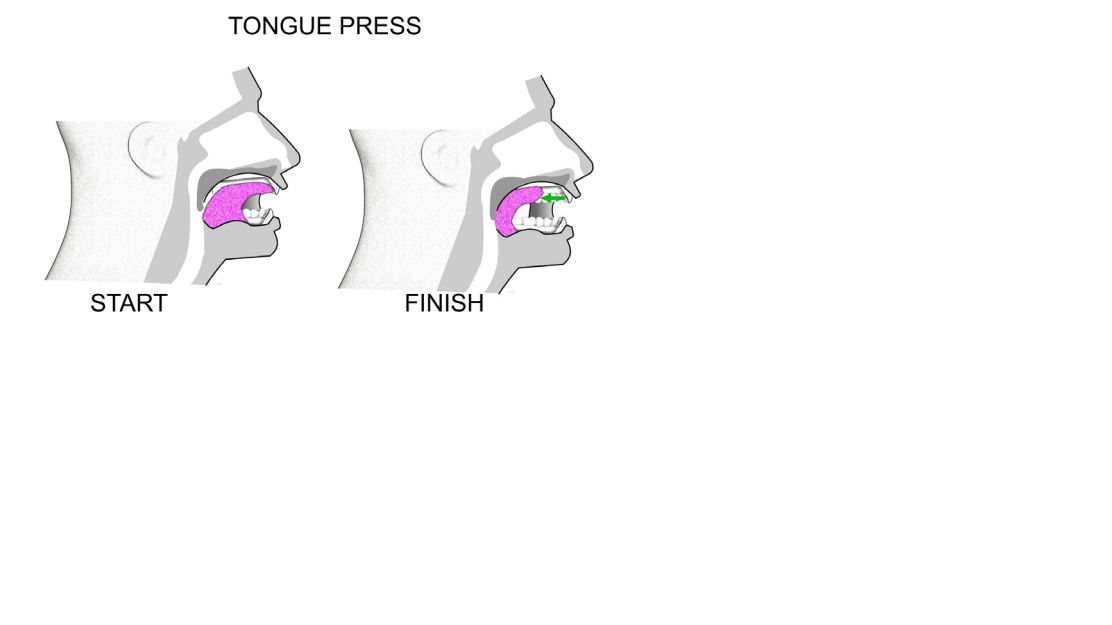
 TONGUE PRESS
TONGUE PRESS
Method:
1. Push your tongue against your hard palate (the top and front of your mouth).
2. Do this for 5 seconds.
3. Slide your tongue backward to the back of your mouth.
4. The initial third of your tongue should be against your hard palate, not just the tip.
5. Keep your jaw open throughout the exercise.
6. Refrain from biting down - keep your teeth apart.
7. Repeat this movement 10 times.
8. Repeat 4 times a day.
Purpose – to strengthen the genioglossus (the main muscle used for sticking your tongue out), and to increase the strength in the hyoid muscles and bone. The hyoid bone is located in the centre of the neck. It sits between the chin and thyroid cartilage.
The exercise assists by putting the hyoid bone in the correct position and keeping it there1.
The hyoid bone is a free moving, u-shaped bone in the neck. The volume of the tongue should reduce too.
Differential Diagnosis[edit | edit source]
Other diagnoses, especially other sleep disorders, may present as OSA due to similar symptoms (ex: fatigue, excessive sleepiness, HTN, sleep disturbance).[18] Alternative diagonses include:
- Nocturnal Frontal Lobe Epilepsy[19]
- REM Behaviour Disorder[10]
- Periodic Limb Movement Disorder[10] [15]
- Central Sleep Apnea[10] [15]
- Insomnia[8]
- Aging and Age-Related Changes (sleeping less, tiredness, nocturia)[8]
- Medications (side effects, multiple prescriptions)[8]
- Hypothyroidism[8] [15]
- Narcolepsy[20] [15]
- Shift Work Sleep Disorder (SWSD)[20]
- Idiopathic Hypersomnia[20]
- Asthma[15]
- Gastroesophageal Reflux Disease (GERD)[15]
- Chronic Obstructive Pulmmonary Disease (COPD)[15]
- Depression[8] [15]
Case Reports/ Case Studies[edit | edit source]
1. Daoulah A, Ocheltree S, Al-Faifi S, Ahmed W, Asrar F, Lotfi A. Sleep apnea and severe bradyarrhythmia – an alternative treatment option: a case report. J Med Case Reports 2015; 9(1): 113-117.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437673/ (OSA and Bradyarrhythmia)
2. Guimarães T, Colen S, Cunali P, Rossi R, Dal-Fabbro C, Ferraz O, et al. Treatment of obstructive sleep apnea with mandibular advancement appliance over prostheses: A case report. Sleep Science 2015;8(2):103-106.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608885/ (Treatment of OSA with Mandibular Appliance)
3. Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of Cancer in Patients with Insomnia, Parasomnia, and Obstructive Sleep Apnea: A Nationwide Nested Case-Control Study. J Cancer 2015;6(11):1140-1147.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615350/ (OSA and Cancer)
4. Cadby G, McArdle N, Briffa T, Hillman D, Simpson L, Knuiman M, et al. Severity of OSA Is an Independent Predictor of Incident Atrial Fibrillation Hospitalization in a Large Sleep-Clinic Cohort Chest. 2015;148(4):945-952.
http://www.sciencedirect.com/science/article/pii/S0012369215502833 (OSA and A-fib)
5. Meuleners L, Fraser M, Govorko M, Stevenson M. Obstructive Sleep Apnea, Health-Related Factors, and Long Distance Heavy Vehicle Crashes in Western Australia: A Case Control Study. Journal of Clinical Sleep Medicine 2015; 11(4): 413-418.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365454/ (OSA and MVA)
Resources[edit | edit source]
American Sleep Apnea Association
American Sleep Association (ASA)
References[edit | edit source]
- ↑ 1.0 1.1 Strohl KP. Sleep Apnea [Internet]. Kenilworth (NJ): Merck & Co., Inc.; c2016 [cited 2016 Mar 30]. Available from: http://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea
- ↑ 2.0 2.1 2.2 2.3 2.4 Young T, Peppard P, Gottlieb D. Epidemiology of Obstructive Sleep Apnea. Am J Respir Crit Care Med 2002;165(9):1217-1239. http://www.atsjournals.org/doi/full/10.1164/rccm.2109080#.Vu73OZMrKYU (accessed 20 March 2016).
- ↑ 3.0 3.1 3.2 3.3 3.4 Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Epstein L, Kristo D, Strollo Jr. P, Friedman N, Malhotra A, Patil S, et al. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Journal of Clinical Sleep Medication 2009; 5(3): 263-276. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ Patil SP, Schneider H, Schwartz AR, Smith, PL. Adult Obstructive Sleep Apnea: Pathophysiology and Diagnosis. Chest [Internet]. 2007 Jul [cited 2016 Mar 30];132(1):325-337. Available from: http://journal.publications.chestnet.org/article.aspx?articleid=1085264#t1
- ↑ Nieto F, Young T, Lind B, Shahar E, Samet J, Redline S, et al. Association of Sleep-Disordered Breathing, Sleep Apnea, and Hypertension in a Large Community-Based Study. JAMA 2000; 283(14): 1829-1836. http://jama.jamanetwork.com/article.aspx?articleid=192578&resultclick=1 (accessed 20 March 2016).
- ↑ 7.0 7.1 Yaggi H, Concato J, Kernan W, Lichtman J, Brass L, Mohsenin V. Obstructive Sleep Apnoea as a Risk Factor for Stroke and Death. The New England Journal of Medicine 2005; 353:2034-2041. http://www.nejm.org/doi/full/10.1056/NEJMoa043104#t=article (accessed 20 March 2016).
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016)
- ↑ Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of cancer in patients with insomnia, parasomnia, and obstructive sleep apnea: a nationwide nested case-control study. J Cancer 2015; 6(11): 1140-1147. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615350/ (accessed 9 April 2016).
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 10.8 10.9 Booth A, Djavadkhani Y, Marshall N. A critical review of the treatment options available for obstructive sleep apnoea: an overview of the current literature available on treatment methods for obstructive sleep apnoea and future research directions. Bioscience Horizons 2014;7(0):1-8. http://biohorizons.oxfordjournals.org/content/7/hzu011.full.pdf (accessed 4 April 2016).
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 Tackett K, DeBellis H. Pharmacotherapy Options in the Treatment of Obstructive Sleep Apnea. US Pharm 2012;37(7):23-26 http://www.uspharmacist.com/content/d/feature/c/35564/ (accessed 5 April 5 2016).
- ↑ 12.0 12.1 Weaver T, Calik M, Farabi S, Fink A, Galang-Boquiren M, Kapella M, et al. Innovative treatments for adults with obstructive sleep apnea. Nat Sci Sleep 2014; 6: 137-147.
- ↑ 13.0 13.1 13.2 Shayeb M, Topfer L, Stafinski T, Pawluk L, Menon D. Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Canadian Medical Association Journal 2013; 186(1):E25-E51. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3883848/pdf/18600e25.pdf (accessed 7 April 2016).
- ↑ 14.0 14.1 14.2 14.3 Maurer J. Early diagnosis of sleep related breathing disorders. GMS Current Topics in Otorhinolaryngology- Head and Neck Surgery 2010; 7(3): 1-20. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834/ (accessed 7 April 2016).
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 15.9 Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.
- ↑ 16.0 16.1 16.2 Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T. Sleep Apnea and Cardiovascular Disease: An American Heart Association/American College of Cardiology Foundation Scientific Statement From the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing In Collaboration With the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). J Am Coll Cardiol [Internet]. 2008 Aug [cited 2016 Mar 30];52(8):686-717. Available from: http://content.onlinejacc.org/article.aspx?articleid=1139136#tab1
- ↑ 17.0 17.1 Schwartz A, Smith P, Oliven A. Electrical stimulation of the hypoglossal nerve: a potential therapy. Journal of Applied Physiology 2013;116(3):337-344. http://jap.physiology.org/content/116/3/337.full (accessed 3 April 2016).
- ↑ Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016).
- ↑ Cho J, Kim D, Noh K, Kim S, Lee J, Kim J. Nocturnal frontal lobe epilepsy presenting as obstructive type sleep apnea. J Epilepsy Res 2011; 1(2): 74-76. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3952334/ (accessed 8 April 2016)
- ↑ 20.0 20.1 20.2 McWhirter D, Bae C, Budur K. The assessment, diagnosis, and treatment of excessive sleepiness: practical considerations for the psychiatrist. Psychiatry (Edgmont) 2007;4(9): 26-35. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880940/ (accessed 9 April 2016).