Should I receive manual therapy and exercise for my neck pain?: A patient decision aid
Introduction[edit | edit source]
This decision aid is for you if:
- You are 16 years of age or older
- You have simple mechanical neck pain
What is simple mechanical neck pain?[edit | edit source]
- Neck pain is an unpleasant sensory and emotional experience that the brain uses to protect the neck against a perceived threat
- The perceived threat may be associated with injury to the muscles, ligaments, discs, nerves, or joints, but most neck pain is non-specific meaning there is no known cause
- Pain is one protective mechanism that the brain uses to protect the neck against a perceived threat. Other examples of protective mechanisms that your brain might use to protect you from potential threat are: muscle spasm, weakness, or moving out of the painful position
- ‘Mechanical neck pain’ is neck pain that gets better or worse with certain positions or movements
What will happen with your neck pain if you decide not to get treatment?[edit | edit source]
- Every person’s experience with neck pain is different
- Most people with non-specific neck pain experience a large decrease in pain and disability during the first 6-7 weeks after first noticing the pain[1]
- Average decrease in pain intensity: from 62/100 at the start to 34/100 after 6-7 weeks
- Average decrease in disability: from 30/100 at the start to 17/100 6-7 weeks later
- In neck pain from a whiplash injury, pain and disability will usually improve during the first 12 weeks[2]
- Average decrease in pain intensity: from 41/100 at the start to 24/100 6 months later
- Average decrease in disability: from 41/100 at the start to 24/100 after 6 months
- The majority of people who experience whiplash have recovered or have only mild symptoms remaining at 3-6 months after injury[3][4][5]
- 5 out of every 10 people who experience whiplash recover within 3-6 months
- 3-4 out of every 10 people have mild to moderate pain at 3-6 months
- 1-2 out of 10 people continue to have more severe pain at 3-6 months
What are your options?[edit | edit source]
- Option #1: Exercise
- Option #2: Manual therapy
- Option #3: A combination of manual therapy and exercise
- Option #4: Discuss other options with your physiotherapist or physician
- Option #5: Do nothing or continue with current strategy
Note: As mentioned above, most people get better without seeking help. Only a small number of people with neck pain need to seek help. The majority of those that do seek help are treated conservatively and manual therapy and exercise are frequently used treatment options. Other treatments for neck pain that could be discussed with your physiotherapist or physician include: medicine, heat or cold, acupuncture, TENS, laser, education, cognitive behavioural therapy, and psychological supportive care.
What types of exercise can be used to help your neck pain?[edit | edit source]
- Range of motion or stretching exercises
- Strengthening exercises
- Endurance exercises
What types of manual therapy can be used to help mechanical neck pain?[edit | edit source]
- Mobilization of the neck
- Passive movements to the joints in the neck that are applied at lower speeds and varying amplitudes
- Manipulation of the neck
- A passive, high velocity, low amplitude thrust applied to joints in the neck. This movement may or may not be associated with a ‘popping noise’
- Manipulation of the upper back
- A passive, high velocity, low amplitude thrust applied to joints in the upper back
- Massage
- A passive force applied to soft-tissues including skin, muscles, and connective tissue
- This option is not discussed in this decision aid, but could be discussed with your physiotherapist or doctor
What are some factors that may influence your decision?[edit | edit source]
The following are conditions that may impact whether manual therapy and exercise are safe and effective treatment options. Be sure to discuss the presence of any of these conditions with your physiotherapist before beginning treatment.
- Broken bone or fracture
- Osteoporosis
- Rheumatoid arthritis
- Vertebral fusion
- Cancer
- Infections (example: tuberculosis)
- Neurological deficits (example: stroke or spinal cord injury)
- Blood-flow or vascular problems (example: anticoagulation or carotid artery dissection)
- Endocrine system dysfunction
- Osteomyelitis
- Dislocation or instability
- Down’s Syndrome
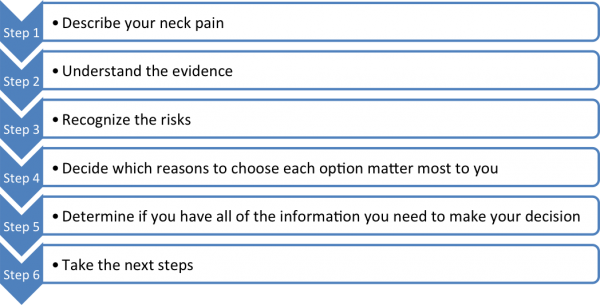
The following steps may help you decide what treatment option is best for you:[edit | edit source]
Access the decision aid[edit | edit source]
Each Step of the tool-kit can be accessed through the following links:
Step 1 – Describe your neck pain[edit | edit source]
Step 2 – Understand the evidence[edit | edit source]
Step 3 – Recognize the risks[edit | edit source]
Step 4 – Decide which reasons to choose each option matter most to you[edit | edit source]
Step 5 – Determine if you have all of the information you need to make your decision[edit | edit source]
Step 6 – Take the next steps[edit | edit source]
Sponsors[edit | edit source]
References[edit | edit source]
- ↑ Hush JM et al. Prognosis of Acute Idiopathic Neck Pain is Poor: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil 2011;92:824-9.
- ↑ Kamper SJ, Rebbeck TJ, Maher CG, McAuley JH, Sterling M. Course and prognostic factors of whiplash: a systematic review and meta-analysis. Pain 2008;138:617-29.
- ↑ Carroll L, Holm L, Hogg-Johnson S, Cote P, Cassidy J, Haldeman S, et al.. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD).. Spine 2008;33(4S):S83-92.
- ↑ Sterling M, Jull G, Kenardy J.. Physical and psychological factors maintain long term predictive capacity following whiplash injury. Pain 2006;122(1-2):102-108.
- ↑ Sterling M, Hendrikz J, Kenardy J.. Compensation claim lodgement and health outcome developmental trajectories following whiplash: A prospective study.. Pain 2010;150(1):22-8.