Sciatica
Description[edit | edit source]
Sciatica is a debilitating condition in which the patient experiences pain and/or paresthesias in the distribution of the sciatic nerve or an associated lumbosacral nerve root.
- A common mistake is referring to any low back pain or radicular leg pain as sciatica.
- Sciatica is specific to the pain that is a direct result of sciatic nerve or sciatic nerve root pathology.
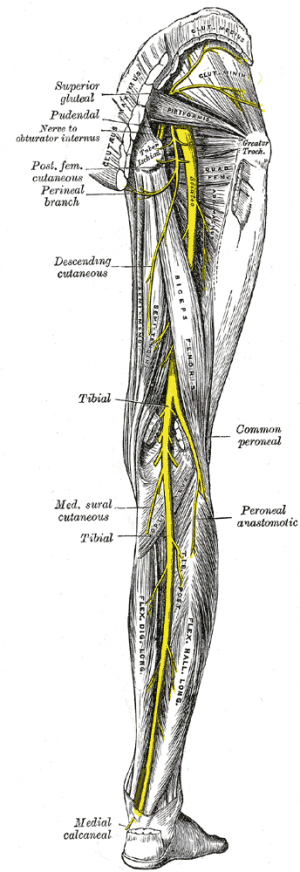
The sciatic nerve is made up of the L4 through S2 nerve roots which coalesce at the pelvis to form the sciatic nerve. At up to 2 cm in diameter, the sciatic nerve is easily the largest nerve in the body.
- Sciatica pain often is worsened with flexion of the lumbar spine, twisting, bending, or coughing.
- The sciatic nerve provides direct motor function to the hamstrings, lower extremity adductors, and indirect motor function to the calf muscles, anterior lower leg muscles, and some intrinsic foot muscles.
- Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot.
Most cases of sciatica result from an inflammatory condition leading to an irritation of the sciatic nerve. [1]
Etiology[edit | edit source]
Any condition that may structurally impact or compress the sciatic nerve may cause sciatica symptoms.
- The most common cause of sciatica is a herniated or bulging lumbar intervertebral disc.
- In the older persons, lumbar spinal stenosis may cause these symptoms as well.
- Spondylolisthesis or a relative misalignment of one vertebra relative to another may also result in sciatic symptoms.
- Lumbar or pelvic muscular spasm and/or inflammation may impinge a lumbar or sacral nerve root causing sciatic symptoms.
- A spinal or paraspinal mass including malignancy, epidural hematoma, or epidural abscess may also cause a mass-like effect and sciatica symptoms[1]
Epidemiology[edit | edit source]
- No gender predominance
- Peak incidence occurs in patients in their fourth decade
- Lifetime incidence reported between 10% to 40%
- Annual incidence of 1% to 5%
- No association with body height has been established except in the age 50 to 60 group.
- Rarely occurs before age 20 (unless traumatic)
- Physical activity increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms.
- Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions[1].
Clinical Presentation[edit | edit source]
Patient with sciatica can present with neurological symptoms such as:
- Pain (intense pain in the buttock)
- Lumbosacral radicular leg pain
- Numbness
- Muscular weakness
- Gait dysfunction
- Sensory impairment/disturbance
- Hot and cold or tingling/ burning sensations in the legs
- Reflex impairment
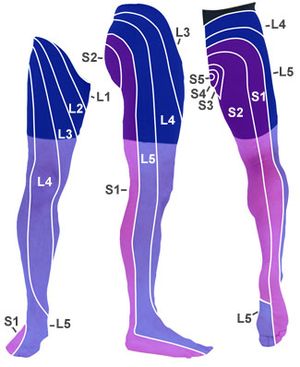
- Paresthesias or dysesthesias and oedema in the lower extremity that can be caused by the irritation of the sciatic nerves (the lumbar nerve L4 and L5 and the sacral nerves S1,S2 and S3).[2][3][4]
Sciatica symptoms can also differ, depending on which nerve is affected.
- L4: When the L4 nerve is compressed or irritated, the patient feels pain, tingling and numbness in the thigh. The patient also feels weak when straightening the leg and may have a diminished knee jerk reflex.
- L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes.
- S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished.
Differential Diagnosis[edit | edit source]
A thorough differential list is important in considering a diagnosis of sciatica and should include.
- Herniated lumbosacral disc
- Muscle spasm
- Nerve root impingement
- Epidural abscess
- Epidural hematoma
- Tumor
- Potts Disease, also known as spinal tuberculosis
- Piriformis syndrome[1]
Evaluation[edit | edit source]
Sciatica is most commonly diagnosed by:
1. History
- Complaints of radiating pain in the leg, which follows a dermatomal pattern[5].
- Pain generally radiates below the knee, into the foot[6].
- Dermatome maps used to locate the distribution of the pain[5].
- Patients complain about low back pain, which is usually less severe than the leg pain[5].
- Patients may also report sensory symptoms.
2. Imaging (if warranted)
- Plain films of the lumbosacral spine may evaluate for fracture or spondylolisthesis.
- Noncontrast CT scan may be performed to evaluate fracture if plain films are negative. Pain that has been persistent for 6 to 8 weeks and not responding to conservative management should be imaged.
- In cases where the neurologic deficit is the present or mass effect is suspected, immediate MRI is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology[1]
Outcome Measures[edit | edit source]
Many to choose from, below are but a few, all dependant on cause and assessment
- Short Form-36 bodily pain (SF-36 BP)
- Oswestry disability index
- Roland-Morris disability index
- VAS-score: one of leg pain and one of back pain[7]
- McGill pain Questionnaire[7]: this questionnaire looks at the location, intensity, quality and pattern of the pain as well as alleviating and aggrevating factors[8].[8][8][8][12][11][11]
- VAS
- TUG
- Tampa Scale for Kinesiophobia[9]
- Pain Catastrophising Scale[9]
Examination[edit | edit source]
Clinicians should always look for and inquire about red flags when evaluating sciatica or in patients who present with any low back pain.
Medical Management[edit | edit source]
Medical Therapies
- A short course of oral NSAIDs
- Opioid and nonopioid analgesics
- Muscle relaxants
- Anticonvulsants for neurogenic pain
- Localized corticosteroid injections
- Deep tissue massage may be helpful
- Physical therapy consultation (see below)
- Surgical evaluation and correction of any structural abnormalities such as disc herniation, epidural hematoma, epidural abscess or tumor
Physical Therapy Management[edit | edit source]
In most cases of sciatica, conservative treatment is favoured. The evidence does not show that one treatment is superior to the other[10]
1. Patient Education
- Use of hot or cold packs for comfort and to decreased inflammation
- Avoidance of inciting activities or prolonged sitting/standing
- Practicing good, erect posture
- Engaging in exercises to increase core strength
- Gentle stretching of the lumbar spine and hamstrings
- Regular light exercises such as walking, swimming, or aquatherapy
- Use of proper lifting techniques
For comprehensive treatment see Links below
- Disc Herniation
- Lumbar Discogenic Pain
- Spinal Stenosis
- Degenerative Disc Disease
- Spondylolisthesis
- Piriformis Syndrome
- Sacroiliac Joint Dysfunction
- Corticosteroid injections
- Acupuncture
- Massage therapy has proven to be useful with the treatment of back pain. It promotes blood circulation, muscle relaxation and the release of endorphins[11],[12],[13].
Concluding Remarks[edit | edit source]
- The key to sciatica is patient education.
- There are many causes of sciatica and the disorder is best managed with a team of healthcare professionals that includes an orthopedic surgeon, physical therapist, neurologist, rehabilitation nurse, and a pain specialist.
- Unless there is an acute compression of the spinal nerves, the majority of cases of sciatica are best managed conservatively.
- Patients should be encouraged by the clinician and nurse to lose weight, stop smoking and enroll in a physical therapy program.
- Bed rest should be limited.
- The pharmacist should caution the patient against the use of prescription-strength medications to avoid dependence and other adverse effects.
- Surgery should only be undertaken when conservative methods have failed.
- Regular exercise is essential[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Texas Medicine. 1987 Mar 1;83(3):55-6.Available from:https://www.statpearls.com/kb/viewarticle/28772/ (last accessed 12.9.2020)
- ↑ Ardman C. et al., Sciatica Solutions: Diagnosis, treatment and cure of spinal and piriformis problems, 1st edition, W.W. Norton & Company, 2007
- ↑ Jacobs W. et al., Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review (of RCT’s) (1A)
- ↑ Ailianou A. et al., Review of the principal extra spinal pathologies causing sciatica and new MRI approaches., The Britisch Journal of Radiology, 2012, 85(1014): 672-681 (2C)
- ↑ 5.0 5.1 5.2 B.W Koes, M.W Van Tulder, W.C Peul. Diagnosis and treatment of sciatica. BMJ, 23 JUNE 2007, VOLUME 334, p.1313-1314 (1A)
- ↑ Kika Konstantinou, Martyn Lewis, Kate M. Dunn. Agreement of self-reported items and clinically assessed nerve root involvement (or sciatica) in a primary care setting. Eur Spine J (2012) 21:2306–2315. (1B)
- ↑ 7.0 7.1 Brouwer, Patrick A., et al. "Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial." BMC musculoskeletal disorders 10.1 (2009)
- ↑ Ngamkham, Srisuda, et al. "The McGill Pain Questionnaire as a multidimensional measure in people with cancer: an integrative review." Pain Management Nursing 13.1 (2012)
- ↑ 9.0 9.1 Monticone M. et al., Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. (2014) Jan 23(1):87-95
- ↑ Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Pim A. J. Luijsterburg, Arianne P. Verhagen, Raymond W. J. G. Ostelo, Ton A. G. van Os, Wilco C. Peul, Bart W. Koes. European Spine Journal July 2007, Volume 16, Issue 7, pp 881-899 (1A)
- ↑ Abdelilah el Barzouhi, M.D., Carmen L.A.M. Vleggeert-Lankamp, M.D., Ph.D., Geert J. Lycklama, Nijeholt, M.D., Ph.D., Bas F. Van der Kallen, M.D.,Wilbert B. van den Hout, Ph.D., Wilco C.H. Jacobs, Ph.D.,Bart W. Koes, Ph.D., and Wilco C. Peul, M.D., Ph.D. Magnetic Resonance Imaging in Follow-up Assessment of Sciatica. New England Journal of Medicine, 368;11 nejm.org march 14, 2013, P.1000 (1B)
- ↑ Dionne CE. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. 2008
- ↑ John Barrett,Douglas Noel Golding. The practical treatment of backache and sciatica. Redwood Burn Limited. 1984.p97-103.