Scapular Dyskinesia
Introduction[edit | edit source]
The word "Dys" in the term Scapular Dyskinesia refers to the loss of normal scapular mechanics, motion and physiology. Scapular winging is however a clinical observation wherein any part of the scapular departs excessively from the thorax soon after movement is initiated and persists in its disconnect fashion throughout the arm movement. Scapular dyskinesia is considered impairment with a causative origin, hence it isn't a considered to be a condition on its own.
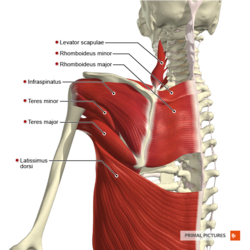
Clinically Relevant Anatomy[edit | edit source]
Typical movement of the scapula occurs in the sagittal, coronal, and transverse planes. The primary movements consist of two translations: superior/inferior, and protraction/ retraction, as well as three rotations: upward/downward, internal/external, and anterior/posterior. Upward rotation is primary and posterior tilt secondary during normal overhead UE elevation with internal/external rotation being minimal until 100°. [1],[2]
Review of the normal ratio of glenohumeral (GH) to scapulothoracic (ST) motion analysed by Doody et al[3] under three-dimensional analysis found that the ratio of GH to ST motion changes from 7.3: 1 in the first 30° of elevation to 0.78: 1 between 90 and 150°. Bagg and Forrest found a ratio of 4.4:1 during early phase, and 1.7:1 within 80 to 140° of shoulder elevation.[4]
Burkhart et al [5] has used the acronym SICK to refer to the syndrome associated with scapular dyskinesia. “SICK” Scapula Syndrome refers to Scapular Malpositioning, Inferior medial border prominence, Coracoid pain and malposition and DysKinesis of scapular movement. It’s an overuse Syndrome. The scapula is protracted and is in anteriorly tilted position secondary to tight pec minor or short head of the biceps at the insertion to the coracoid process. Coracoid tenderness is an important sign of scapular dysfunction, which is secondary to constant traction from tightness at the tendon’s insertion. Dysrhythmia is defined as early or excessive scapular elevation or shrugging on arm elevation and/or a rapid downward rotation during arm lowering, or a non-smooth or stuttering motion during these actions.
Clinical Presentation[edit | edit source]
Overhead athletes have higher prevalence of scapular dyskinesia of about 61% as compared with non-overhead athletes. [6]
Symptoms of isolated SICK scapula: anterior shoulder pain (most common), posterior superior scapular pain, superior shoulder pain, proximal lateral arm pain or any combination of above. Posterosuperior scapular pain may radiate into the ipsilateral paraspinous cervical region or patient may complain of radicular/TOS type symptoms. The onset is almost always insidious.
Kibler classification of scapular dysfunction. [7]
- Type I or Inferior dysfunction. The primary external visual feature is the prominence of the inferior angle as a result of anterior tilting of the scapula in the sagittal plane. Inferior pattern presentation is better visualised while in the hands-on-hips position or during eccentric lowering from overhead elevation. According to Kibler, Type 1 pattern is most commonly found in patients with rotator cuff dysfunction.
- Type 2 or Medial dysfunction. The primary external visual feature is the prominence of the entire medial scapular border due to internal rotation of the scapula in the transverse plane. As with Type 1, the Type 2 presentation becomes more evident in the hands-on-hips position and during active eccentric lowering from overhead. Medial pattern dysfunction most often occurs in patients with glenohumeral joint instability.
- Type 3 or Superior dysfunction. Characterised by excessive and early elevation of the scapula during UE elevation. This pattern has been referred to as compensatory shoulder hiking or shrug and is most often seen in patients with rotator cuff dysfunction and deltoid-rotator cuff force couple imbalances.[8]
Diagnostic Procedures[edit | edit source]
Current tests and measures, while proven to be reliable, have not altogether shown strong validity by demonstrating correlation with biomechanical motion, symptoms, pathology, or outcomes.[9]
Recommendations for appropriate clinical measures include:
1. Determining the presence or absence of dyskinesia
Kibler classification of dysfunction Type 1, 2, or 3 (see video above) or Scapular Dyskinesis Test (SDT) recommended by McClure et al. It is recommended that to perform forward flexion/arm elevation with maximum elevation 3-5 times to reproduce dyskinesia. If the examiner isn't sure about the presence of dyskinesia a 3-5 pound weight is added in each hand and the subject is asked to perform 10 reps of arm elevation inflexion.[10][11]Scapular dyskinesia is more observable in the descent phase of arm motion, prominence of the medial border indicated a positive dyskinesis test.
2. Symptom altering tests.
Scapular retraction test'.[12]This test evaluated the rotator cuff strength in scapular dyskinesia. Baseline AROM and pain are evaluated. This test is positive if the pain is reduced as the therapist assists active elevation by applying a posterior tilt and external rotation motion to the scapula. This application may be used in conjunction with other tests such as Neer's, Hawkin's-Kennedy, and Jobe's relocation.
Scapular assistance test'.[13] This test helps to evaluate scapular contributions to the existing shoulder pain based on alterations in motion. The baseline AROM and pain are evaluated. The therapist then applies an assist to scapular dynamics. This test is positive if ROM is increased or pain is reduced as the therapist manually assists scapular upward rotation during active UE elevation.
Lateral scapular Slide test (LSST) [14]: Measurements are taken from the spine of scapulae to T2/T3, Inferior angle of scapulae to T7/T9 and superior angle of scapulae to T2. The measurements are taken in 3 positions, (A) sitting/standing with arms resting on the side, (B) Hands on the waist, Thumbs Posteriorly (45 abduction), (C) 90 degrees abduction and maximal internal rotation. Measurement should not vary more than 1 to 1.5 cm, more the 1.5 cm difference is significant.
Isometric Scapular Pinch test: The patient in a standing position and is asked to actively squeeze or retract the scapulae together as hard as possible. Normal Response: An individual able to hold the squeeze for 15 to 20 sec without any burning pain or noticeable weakness. Positive: Burning pain present. Watch for: the patient relaxing the contraction.
Scapular Load test: As in position (2) for LSST, Manual load is applied in the anterior, posterior, inferior or superior direction to the arm, and the scapula should not move more than 1.5 cm.
Wall pushup test: The patient performs wall pushups 15 to 20 times. Weakness of scapular muscles (mainly serratus anterior) or winging usually shows up with 5 to 10 pushups. For stronger or younger populations, perform the test on the floor.
3. Manual muscle testing.
MMT for the middle and lower trapezius(manual resistance at 130-150degrees) and serratus anterior (manual resistance of the arm at 130degrees of flexion)
4. Pectoralis minor muscle tightness.
Current measures examine mm length at resting positions, not at maximal length. Unfortunately, there are no validated clinical measures to identify a patient as having a tight pectoralis minor muscle.
5. Static Measurements
Static measurements consist (1) infera: difference in vertical height of the superomedial scapular angle of the dropped scapula compared to contralateral angle. (2) Lateral displacement: difference of superomedial scapular angle from the midline (3) abduction: difference in angular degrees of medial scapular margin from plumb line.
6. Core Evaluation
The examiner stands behind the subject and asks the subject to contract the gluteal muscles while performing the low row test. The subject is asked to keep the shoulder extended and is asked to resist the anterior force offered by the therapist. If the strength of resistance the subject offers the therapist increases, it indicates that core and gluteal strengthening will aid scapular motion and strengthening of the core is hence indicated.[15]
Outcome Measures[edit | edit source]
Management / Interventions[edit | edit source]
Intervention is aimed at reducing posterior capsule[16] and pectoralis minor restriction[17] and restoring periscapular mm balance through exercises promoting early and increased serratus anterior, lower, and middle trapezius activation while minimising upper trapezius activity.[18]
- Manual grade 4 mobilization to reduce posterior capsule tension, cross-body stretch.[16]
- Manual stretching and soft tissue mobilization to decrease pec minor tension (cadaveric studies imply that a position of 150 degrees elevation with 30 degrees scapular retraction is optimal).[17]
- Exercises of sidelying forward flexion, external rotation, prone extension, and prone horizontal abduction to strengthen middle and lower trapezius over upper trapezius.[19],[20]
- Quadruped and variable push-up positions to activate serratus anterior.[18]
Rehab Protocol
Phase I
Flexibility
1. Soft tissue Release: Pec Release, Posterior RTC release, Posterior capsule Release, Upper traps and levator scapulae release (Manual/self-release techniques)
2. Tspine Mobility (manual Mobs/Manips)
3. Tspine Extension Ex
4. Pec Stretch
5. Sleeper’s stretch
6. Genie Stretch
7. Upper traps stretch
Isometrics
1. Scapular Pinches
2. Robbery Pinches
3. Low Row Wall isometrics
4. Shoulder ER isometrics
5. Scapular Depressor isometrics
Isotonics
1. Scapular Pinches w/ Theraband
2. Low Row w/ Theraband
3. Shoulder ER/IR in standing
4. Dynamic Hug
5. Scapular punches
6. Cheerleader Exercises.
Phase II
1. Seated Rows
2. High Rows
3. Prone Rows
4. Standing Robbery w/ theraband
5. Prone Y, I, T and W
6. Lawnmower/Standing D2 Cocking
7. Side lying ER
8. PNF D1/D2
9. Lats Pull downs
10. Scapular clocks
11. Wall washes
12. Thrower’s 10
13. Manually Resisted scapular strengthening
14. Stretches
Phase III
CKC exercises and advanced exercises.
1. Super 6: Upright Row, Dynamic Hug, Cocking/Decelaration, Cocking/acceleration, B/L D2, B/L pullovers
2. Standing cable column punches
3. Bear crawl on Swiss ball
4. Plyoball Decelaration
5. Seated Pike lift
6. Push Plus/Scapular Pushups
7. Standing Snow Angels
8. Wall ball Scours
9. Stretches
Resources[edit | edit source]
An example of a home exercise program in the management of scapular dyskinesis.
Presentations[edit | edit source]
 |
Advanced Exercises for the Upper Quarter: A How To Guide for Scapular Motor Control Rehabilitation
This presentation, created by Stephanie Pascoe as part of the OMPT Fellowship in 2010, describes a how to guide for scapulothoracic rehabilitation. It includes some great animations! |
References[edit | edit source]
- ↑ Ludewig PM et al. Motion of the shoulder complex during multiplaner humeral elevation. J Bone Joint Surg. Am.2009;91:378-389.
- ↑ McClure PW et al. Direct 3-dimentional measurement of scapular kinematics during dynamic movements in vivo.J Shoulder Elbow Surg.2001:10:269-277.
- ↑ Doody SG et al.Shoulder movements during abduction in the scapular plane.Arch Phys Med Rehab.1970:595-604.
- ↑ Bagg SD, Forrest Wj. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane.Arch Phys Med Rehabil.1988:238-245.
- ↑ The disabled throwing shoulder: spectrum of pathology part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitationfckLRBurkhart, Stephen S et al.fckLRArthroscopy , Volume 19 , Issue 6 , 641 - 661
- ↑ Matthew B. Burn, Patrick C. McCulloch, David M. Lintner, Shari R. Liberman, and Joshua D. Harris Prevalence of Scapular Dyskinesis in Overhead and Nonoverhead Athletes: A Systematic Review Orthopaedic Journal of Sports Medicine February 2016 vol. 4 no. 2
- ↑ Kibler WB et al.Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg.2002;11:550-556.
- ↑ Inman VT et al.Observation on the function of the shoulder joint.J Bone Joint Surg.1944;26:1-30.
- ↑ Kuhn JE.Physical examination of the scapula -a systematic review.JOSPT.2009;39:A11.
- ↑ McClure PW, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis: Part 1: Reliability. J Athl Train. 2009;44(2):160-164.
- ↑ Tate AR, McClure PW, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis: Part 2: Validity. J Athl Train. 2009;44(2):165-173.
- ↑ Tate AR et al. Effect of the scapular repositioning test on shoulder impingement symptoms and elevation strength in overhead athletes.JOSPT.2008;38:4-11.
- ↑ Rabin et al. The intertester reliability of the scapular assistance test.JOSPT.2006;36:653-660.
- ↑ Odom CJ, Taylor AB, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: a reliability and validity study. Physical therapy. 2001 Feb 1;81(2):799-809.
- ↑ Sciascia A, Kibler WB. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. International Journal of Sports Physical Therapy. 2022;17(2):117.
- ↑ 16.0 16.1 McClure P et al.A randomized controlled comparison of stretching procedures for posterior shoulder tightness.JOSPT.2007;37:108-114.
- ↑ 17.0 17.1 Muraki T et al.Lengthening of the pectoralis minor muscle during passive shoulder motions and stretching techniques: a cadaveric biomechanical study.Phys Ther.2009;89:333-341.
- ↑ 18.0 18.1 Ludewig PM et al. Relative balance of serratus anterior and upper trapezius muscle activity during push-up exercises.Am J Sports Med.2004;32:484-493.
- ↑ Cools AM et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med.2007;35:1744-1751.
- ↑ de Mey K et al. Trapezius muscle timing during selected shoulder rehabilitation exercises.JOSPT.2009;39:743-752.