Rupture of the Triceps Brachii muscle
Introduction[edit | edit source]
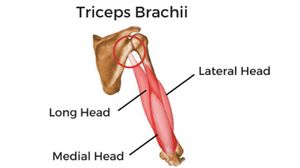
Triceps brachii, the only muscle of the posterior compartment of the arm, is extensor of the forearm.It consists of three muscle bellies or heads: the long head origins from the infra-glenoid tubercle of the scapula;the lateral head from the posterior side of the humerus, proximal to the radial nerve groove; the medial head from the posterior side of the humerus, distal to the radial nerve groove and from the intermuscular medial septum. All the muscle heads converge to a single tendon, which inserts onto the proximal surface of the olecranon process[1].
Definition & Etiology[edit | edit source]
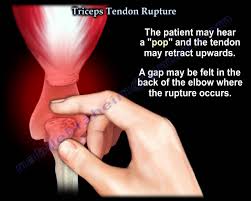
Triceps tendon tear is a relatively rare injury and the rupture of the distal triceps is the most uncommon rupture in the upper extremity.Namely less than 1% of all the upper extremity tendon injuries.[2][3].Rupture is often associated with pre-existing systemic conditions or drug treatments, including the local or systemic of steroids or systematic endocrine disorders, renal failure, anabolic steroid use, local steroid injection.Patients tend to be men who practice sports and are from 30 to 50 years of age. Injury is commonly caused by falls on an outstretched hand, direct trauma on the elbow,lifting against resistance[4] or sometimes it occurs after a surgical procedure where the triceps was reattached. For example some case reports confirm triceps ruptures after following total elbow arthroplasty.The clinical examination may detect pain, a palpable tendon gap, and extension weakness, while a pathognomonic flake sign may be seen on radiographs.The patient describes often an unexpected “pop” or giving way. Subsequently the patient has pain and weakness in the extremity. [2] Magnetic resonance imaging is widely accepted as the gold standard to evaluate the size and extension of the tear: triceps lesions often occur at the tendon insertion and result in either partial or total tears.[5]
Clinical Presentation[edit | edit source]
The presenting signs and symptoms are correlated with three different aspects:
- The type of the lesions (tendinous, tendon avulsion or inside the muscle belly),
- The degree of the extension (partial or total).
- The time (acute or chronic).
In general, the triceps lesions are characterised by spontaneous and evoked pain on palpation at the indicated site of the lesion,a patient with a triceps rupture can have posterior elbow pain, triceps weakness, a swelling There will usually be tenderness and a palpable defect in the tendon that can be seen proximal to the olecranon[6][7]. When the patient is unable to extend his arm against gravity, you can expect a complete triceps rupture. A palpable defect is not always present, but sometimes can be found in the posterior arm. Swelling and echymosis are other nonspecific findings. [8]
Examination[edit | edit source]
A patient with a triceps rupture can have posterior elbow pain, triceps weakness, a swelling and a palpable defect in the tendon. [3] When the patient is unable to extend his arm against gravity, you can expect a complete triceps rupture. A palpable defect is not always present, but sometimes can be found in the posterior arm.Discerning between partial and complete ruptures can be a diagnostic challenge[6].The test to evaluate the triceps function is performed by the therapist with the patient in the prone position with the elbow flexed to 90°, the upper arm supported and the forearm hanging free. A partial tendon lesion is manifested by weakness, and the ability to actively extend the elbow is limited against the gravity but not against resistance. This finding is likely secondary to an intact lateral expansion or a compensating anconeus muscle. A total tendon tear is manifested by loss of extension strength against gravity, and the elbow extension against resistance is impossible. Also, the triceps extension tests can be performed observing the ability of the patient to extend the elbow over his\her head, against gravity. We have defined a test for triceps insertion tendon rupture called “fall down triceps test.” This test assesses the inability of the patient to keep the forearm in extension against gravity. The patient stands up with the shoulder at 90° of abduction, and the examiner stays behind and keeps the forearm in full extension. The forearm falls down when the examiner leaves the forearm, if the triceps tendon presents a complete rupture the forearm drops to 90° of flexion, for partial ruptures the patient is able to keep the forearm at 40°–50° of extension[6].
Imaging Studies[edit | edit source]
The imaging studies help to identify the level of lesion (olecranon insertion, myotendinous junction or intramuscular), discriminate partial from complete tear
, estimate the amount of the tendon retraction and also exclude any associated osseous injuries. he lateral X-rays of the elbow are useful in confirming the diagnosis if a small extra-articular avulsion fracture of the olecranon (flake sign) is present The X-rays (antero-posterior and lateral) and computer tomography (CT) are also helpful to aid the diagnosis of injuries associated with triceps rupture, such as ipsilateral radial head and capitellum fractures. Ultrasonography may be used, but it provides limited anatomical details. MRI is the best technique for assessment of the tendon lesions because it provides more details on distinguishing: the degree of the lesion and of the tendon retraction[9] [10] Triceps tendinitis is an uncommon
Differential Diagnosis[edit | edit source]
- Fracture[2]
- Joint dislocation[2]
- Intramuscular tear[2],Weakness due to the neurological radial nerve problems and Triceps tendinitis but it is an uncommon condition reported in literature[6] [11]
Surgical Management[edit | edit source]
Surgical interventions are recommended in triceps rupture cases,the surgical intervention is recommended in acute complete ruptures, and non-operative treatment is reserved for patients with major comorbidities, as well as for partial ruptures with little functional disability and in low demanding patients. Various techniques and approaches as the direct repair to bone, the tendon augmentation, the anconeus rotation flap and the Achilles tendon allograft have been proposed for the management of these challenging injuries. The goal of surgical management should be an anatomical repair of the injured tendon by selection of a procedure with a low complication rate and one that allows early mobilization[6],
Non-surgical Management[edit | edit source]
Conservative management plays a role in partial triceps injuries involving the muscle belly or muscular–tendinous junction or in the partial rupture of the distal tendon insertion when there is no significant loss of the extension power against gravity and resistance according to the patient’s age and lifestyle[6]. Although some patients will experience persistent weakness. [2][3]
When the patient has a partial rupture it’s often treated conservative by splinting the elbow for four to six weeks. The immobilization was followed by range of motion exercises. Six months after the injury, the full strength and ROM was achieved.[12]
Physical therapy Mangement:[edit | edit source]
The treatment after triceps surgery contains several steps :
A) Protected phase :
1) Splinting following triceps repair:
After the repair of the triceps due to surgery, the elbow is immobilized in a long arm splint initially, thereby the elbow is placed in 30 – 45° elbow flexion with the forearm in neutral position and the wrist is often supported. There is a huge variability in recommendations for management after the operation. But the postoperative position is decided by the surgeon, based on tension and quality of the tendon repair, other injuries and the medical history of the patient. This position is also unique to each patient. [2][13]
A hinged splint can be used after triceps repair if early controlled motion is desired. This splint blocks elbow flexion on the one hand, on the other hand it allows dynamic/gravity assisted elbow extension. The goal is a progressive elbow flexion by weekly advancing the range of motion block. So this splint allows passive elbow flexion and active elbow flexion through a range which is defined. When the patient is not exercising , the splint is locked in one position. In this phase patient education is also very important. The patient must be aware of the prohibition for active elbow extension, because this could lead to avulsion or rupture of the repaired tendon. For example : pushing himself out of a chair may not be performed by his operated arm.[2][14]

When the patient has difficulties with relaxing the repaired muscle or when he is untrustworthy during the performances of the exercises out of a protective splint, in this cases we use a dynamic traction splint.[2]
2) Therapy program
In this phase we can start with early controlled motion, whether the patient uses a static, hinged or dynamic splint.
When the patient has a static splint it’s an absolute must that the patient is reliable, in other words the patient may not cross the limitations for range of motion or may not actively contract the repaired muscle. When the patient not obeys those rules, this might result in tendon rerupture. We can prevent this problem by using a hinged splint, because then there are blocks placed to limit end range and it also assists dynamic motion.[2]
There is not really a consensus in literature about the optimum time frame to begin early controlled motion. In this article the ECM starts from day 10 to day 14 postoperatively. This has some advantages such as : the reduction of pain and edema. As you can see on the photos below, the ECM program contains four exercises namely[2] :
A) full passive elbow extension
B) active and/or passive elbow flexion to 30 °
C) the use of a template splint, to block degree of active flexion
D) passive forearm rotation with the elbow held in extension
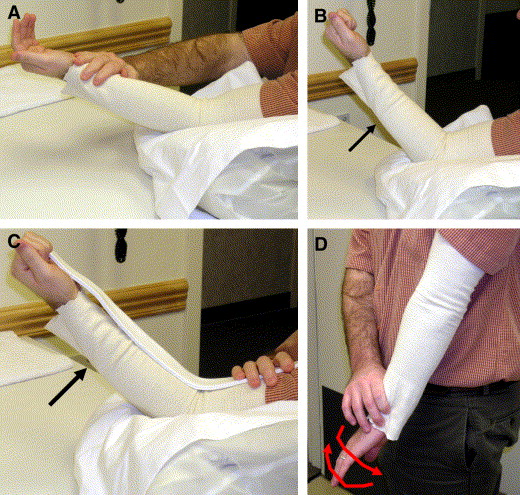
The motion performance during the home program can be assisted by the gravity. Increased flexion is allowed with each successive week. The full active elbow and forearm range motion is allowed at week 6. After the operation the patient has often edema in the hand. We can explain this by the fact that the hand is in a dependant position for much of the day caused by the immobilization of the elbow in extended position. Therefore it’s highly recommended to start immediately after the surgery with some exercises like : hand pomping, elevation above the heart level, the use of compressive glove or wrap. [2]
Additional therapy interventions include :
* thermal agents
* therapist assisted motion within range limits
* edema control
* pain management
* scar mobilization
If it is necessary :
* isometric strengthening for the hand and shoulder rotation, abduction and adduction.[2]It’s very important to be carefully with an elbow flexion combined with end range of shoulder elevation because this will stress the triceps repair. Full-time immobilization is used for three to four weeks, if the patient follows not the ECM program because more protection for the repair is necessary .[2]
B) Progressive motion phase:
Six weeks after the operation , the patient begins with active contraction of the triceps. Elbow extension against gravity is definitely emphasized to encourage active motor recruitment rather then using the gravity to assist the extension.
There are some techniques to restore end range of active motion such as [2]:
* place and hold exercises at available end range
* PNF = Proprioceptive neuromuscular facilitation patterns of exercise
* neuromuscular electrical stimulation
It’s possible that treatment is demanded for capsular tightness or joint contractures. This treatment contains[2] :
* thermal agents
* joint mobilization
* sustained positioning
* splints to increase range of motion
C) Strengthening phase:
This phase begins 10-12 weeks postoperatively. It may take several months before the strength is returned. It’s highly important that the active range of motion is equal to passive range of motion when starting this phase. Passive limitations can be treated as long as there are still improvements. The fact that this phase starts after 10 – 12 weeks guarantees that the tendon is adequately healed so that it can tolerate the stress exerted by the strengthening exercises. [2]
The strengthening starts with up to 50 % effort isometric contraction of the muscle tendon unit. The effort is determinated by measuring the maximal voluntary contraction (MVC) of the not- operated side with a hand held dynamometer and having the patient exercise up to 50% of MVC. We start the contraction in midrange and later we progress to the end range of motion. If the patient doesn’t develop pain, the effort is increased to the maximum.
These are the exercises for the triceps strengthening :
* positioning the forearm in supination, neutral and pronation to address all three heads of the triceps.[2]
The strengthening program is finally advanced to :
* Isotonic concentric exercises , using :
• Free weights
• Elastic bands
• PNF diagonal patterns
*eventually advanced to eccentric muscle contraction
These two photos demonstrate exercises to complete the stabilization and mobilization exercises.
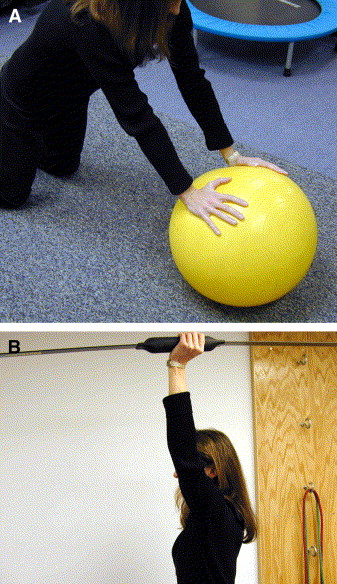
A : Demonstration of weight-bearing and scapular control exercise to facilitate full limb reconditioning
B: Demonstration of the Body Blade
If there’s a development of pain at the surgical site, the intensity of the strengthening program is immediately reduced.
Sixteen weeks after the operation , sports-specific and work -specific activities begin.[2][15]
References[edit | edit source]
- ↑ Williams PL, Bannister LH, BERY M, Collins P, DYSON M, DUSSEK J. MWJ Gray’’s Anatomy.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 Blackmore S.M. et al, Management of distal biceps and triceps ruptures. Journal of hand therapy, 2006; 19 : 154-169. Level B
- ↑ 3.0 3.1 3.2 Rineer C.A. et al., Elbow tendinopathy and tendon ruptures : Epicondylitis, biceps and triceps ruptures. Journal of hand surgery, 2009 ; 34 A : 566 – 576 Level B
- ↑ Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. Journal of shoulder and elbow surgery. 1998 Mar 1;7(2):151-3.
- ↑ Giannicola G., Bullitta G., Sacchetti F.M., Polimanti D., Scacchi M. (2018) Triceps Ruptures. In: Porcellini G., Rotini R., Stignani Kantar S., Di Giacomo S. (eds) The Elbow. Springer, Cham
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Celli A. Triceps tendon rupture: the knowledge acquired from the anatomy to the surgical repair. Musculoskeletal surgery. 2015 Sep 1;99(1):57-66.
- ↑ Rineer C.A. et al., Elbow tendinopathy and tendon ruptures : Epicondylitis, biceps and triceps ruptures. Journal of hand surgery, 2009 ; 34 A : 566 – 576 Level B
- ↑ Blackmore S.M. et al, Management of distal biceps and triceps ruptures. Journal of hand therapy, 2006; 19 : 154-169. Level B
- ↑ Gaines ST, Durbin RA, Marsalka DS (1990) The use of magnetic resonance imaging in the diagnosis of triceps tendon ruptures. Contemp Orthop 20:607–611
- ↑ Kaempffe FA, Lerner RM (1996) Ultrasound diagnosis of triceps tendon rupture: a report of 2 cases. Clin Orthop Relat Res 332:138–142
- ↑ Kapandji IA (1970) The elbow. In: The physiology of the joints, vol 1. Churchill Livingstone, London, pp 78–121
- ↑ Morrey BF. Morrey BF, Sanchez-Sotelo J. Functional evaluation of the elbow. The Elbow and Its Disorders. 2009.
- ↑ Blackmore SM, Jander RM, Culp RW. Management of distal biceps and triceps ruptures. Journal of Hand Therapy. 2006 Apr 1;19(2):154-69.
- ↑ (1) MacInnes SJ, Crawford LA, Shahane SA. Disorders of the biceps and triceps tendons at the elbow. Orthopaedics and Trauma 2016 August 2016;30(4):346-354
- ↑ Monasterio M, Longsworth KA, Viegas S. Dynamic hinged orthosis following a surgical reattachment and therapy protocol of a distal triceps tendon avulsion. Journal of Hand Therapy. 2014 Oct 1;27(4):330-4.