Respiratory Management in Spinal Cord Injury
Introduction[edit | edit source]
Respiratory dysfunction is one of the most common medical complications, as well as the leading cause in reduced Quality of Life (QoL) and mortality among individuals with Spinal Cord Injuries (SCIs)[1][2][3]. The SCI level and whether or not the SCI is complete or incomplete is directly associated with the extent of the respiratory dysfunction. A universal classification tool used to assess the level and the completeness is known as the American Spinal Injury Association (ASIA) scale. Cervical and higher thoracic SCIs are more prevalent to develop respiratory complications[1]. This is due to the diaphragm impairment. The diaphragm is accountable for 65% of forced vital capacity and therefore plays a large role in ventilation[3]. Literature indicates that 67% of individuals with SCI, present with respiratory complications in the acute stage, of which higher cervical SCI are far more common[4].
Pathophysiology[edit | edit source]
In order to understand how respiratory functioning is affected among individuals with SCI, it is important to understand how normal ventilation occurs. The video below explains the mechanisms of breathing in healthy individuals;
SCI that involves the innervation of the diaphragm, intercostal muscles and the abdominal muscles directly affects the mechanics of breathing. The following table illustrates the level of neurological injury relevant to impairment[1][2];
| Neurological level | Impairment |
|---|---|
| C1-3 | Full ventilator dependent |
| C3-4 | Periods of unassisted ventilation
Diaphragm impaired - ↓ tidal volume & vital capacity |
| C5 | Independent ventilation
Initial ventilatory support Diaphragm intact Intercostals and abdominal muscles impaired - ↓ lung volumes and forced expiration for effective secretion clearance |
| C6-8 | Independent ventilation
Diaphragm intact Intercostals and abdominal muscles impaired - ↓ lung volumes and forced expiration for effective secretion clearance Uses accessory muscles to generate an effective cough |
| T1-4 | Independent ventilation
Diaphragm intact Intercostals intact - normal lung volumes Abdominal muscles impaired - ↓ forced expiration for effective secretion clearance |
| T5-12 | Ventilation near equal or equal to individuals without SCI |
Another common complication that occurs among acute quadriplegia is the excessive bronchial mucus production. The cause of this is still uncertain but is thought to be due to reduced vagal activity. This leads to a parasympathetic imbalance which causes;
- Bronchial spasm
- Increased vascular congestion, and
- Decreased mucociliary activity (related to mechanical ventilation)[1]
After the shock phase, abnormal spinal reflexes may lead to spastic contraction of abdominal muscles. This increases the work of breathing in these individuals and may lead to dyspnea[1].
It is also important to know that erect positions negatively affects ventilation due to a flattened diaphragm and the forward movement of abdominal content which is related to impaired breathing mechanisms. It is therefore important to consider abdominal binders etc to assist with breathing in erect positions[1].
Possible complications[edit | edit source]
- Hypoventilation,
- Reduced surfactant production,
- Mucus plugging,
- Atelectasis,
- Pneumonia
- Pulmonary Oedema
- Pulmonary Embolism
- Sleep-disordered breathing and sleep apnoea syndrome[1][2]
Medical Management[edit | edit source]
The standard medical practice involves early surgical stabilisation of the spine and close monitoring in intensive-care units.[1][2]
Monitoring[edit | edit source]
The entire multidisciplinary team is responsible for monitoring the;
- diaphragmatic function
- pulse oximetry and arterial gasometry
Markers that indicate the need for intubation are;
- VC below 15mL/kg
- Maximum inspiratory pressure below -20cmH2O
- Increased pCO2[2]
Ventilation, Weaning and Extubation[edit | edit source]
Intubation is important when individuals require ventilatory support, which is in 100% of cases with complete C5 and above SCIs. Different ventilation methods and settings are used to the specific respiratory needs of each individual.
Evidence supporting the optimal weaning protocols are limited. However, literature indicates a regime of starting with bidaily trails, 3 to 4 hours rest in between and progressing onwards. Progressive ventilator-free breathing (PVFB), T-tube with pressure support (PS), and synchronized intermittent mandatory ventilation (SIMV) are the most common methods used of weaning. It's important to note however those individuals on SIMV generally take longer to wean successfully.
The decision to extubate has to be made by the entire multidisciplinary team, while closely monitoring and chest physiotherapy should follow. Requirements before extubation include;
- No surgical or diagnostic procedures on the day of extubation
- No sedation
- Stable vital signs as arterial gas levels
- Normal fluid balances
- SATS > 95%, pCO2 < 40-45mmHg
- FiO2 < 25%, PEEP < 5cmH2O
- Inspiratory pressure < -20cmH2O
- VC > 10-15mL/kg of ideal body weight
- Normal Chest X-rays
- Few secretions
- No contra-indications for physiotherapy intervention[1]
Tracheostomy and Decannulation[edit | edit source]
Reasons for tracheostomy include; upper-airway obstruction relieve, preventing upper-airway damage, enabling frequent suctioning and enables long-term ventilatory support. Benefits include patient comfort, reduced work of breathing, improved safety, improved oral hygiene, accelerated weaning and lower risk of ventilator-associated pneumonia[6]. Many individuals with SCI who develop respiratory complications or have high complete SCIs are likely to receive a tracheostomy. When decannulation is considered it is important for the entire multidisciplinary team to assess the airway patency, cough and swallowing effectiveness. As well as oxygen requirements, medical stability, patient co-operation, oxygen dependence and infection markers[1][2].
Physiotherapy Management[edit | edit source]
Secretion Clearance Techniques[edit | edit source]
Assisted Coughing Techniques[edit | edit source]
A synchronized inward and upward manual force under the diaphragm or compression of the rib cage, in order to create intra-abdominal pressure for an effective forceful cough. Ultimately the physiotherapist's manual force will facilitate the intercostal and abdominal muscles to increase the intra-abdominal pressure necessary for an effective cough[1][2].
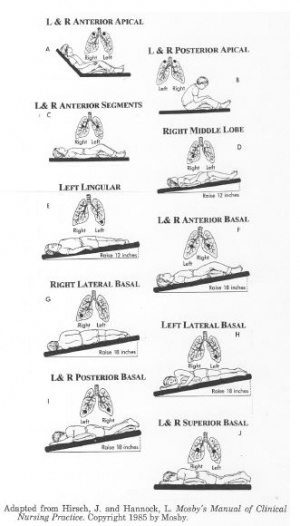
Postural Drainage[edit | edit source]
This will allow gravity to assist the movement of secretions towards the upper airway for removal via coughing or suctioning. Duration of postural drainage can vary from 5 to 10 minutes[1].
Percussions and Vibrations[edit | edit source]
Percussions and vibrations are used as a manual technique by physiotherapists in order to loosen secretions by causing vibrations in the chest wall. Important precautions and contraindications need to be taken into account prior to execution.
Contraindications include;
- Cardiovascular instability
- Tension pneumothorax
- Active pulmonary Tuberculosis (TB)
- Pulmonary embolism (PE)
- Severe pleural effusion
- Unstable spinal - and cranial fractures
- Fractured ribs
- Chest wounds
- Acute hemoptysis
- Increased intracranial pressure (ICP)[1]
Breath stacking[edit | edit source]
Two or more inspiratory breaths before exhalation. This technique can be conduction by the individual actively performing breath stacking (respiratory sniff or inspiratory hold techniques) as well as through using a resuscitation bag with a mouthpiece or facemask[2].
Improve Ventilation[edit | edit source]
Respiratory Muscle Training[edit | edit source]
Respiratory muscle training (RMT) involves one-way valves to target either inspiratory or expiratory muscles[9]. An example is spirometry training.
For more information regarding RMT see this page.
Non-Invasive Ventilatory (NIV) Support[edit | edit source]
This technique applies positive pressure in the airways and is known as positive-pressure support. Examples of positive-pressure support devices are; CPAP, BPAP and IPPB. Individuals should be cooperative and the preferred technique should be conducted during day-time via a mouthpiece and at night-time, via a nosepiece. NIV support are also known to be used for initial ventilatory support or weaning and as night-support.
Mobilization[edit | edit source]
Mobilization is also an effective technique in secretion clearance and improving ventilation. Physiotherapists can assist individuals with SCI to sit out in a chair once the spinal fractures are surgically stabilized. Early mobilization has proven to accelerate recovery and reduce hospital stay. It is however extremely important for physiotherapists to consider using abdominal binders and slow progressive elevation during the spinal shock phase, as an individual with SCI may struggle with hypotension and increased work of breathing in the upright position. Antihypotensive medication can also be administered by the medical team if indicated[2].
Long-Term Ventilation[edit | edit source]
Individuals with SCIs of C5 and higher often require long-term ventilatory support. Caregiver education and extensive training must be conducted by the entire multidisciplinary team. Frequent medical and physiotherapy assessments are advised in order to monitor the individual's condition.
Conclusion[edit | edit source]
Respiratory management is often neglected in the management process of individuals with spinal cord injuries. Physiotherapists are most often primarily responsible for the respiratory management of patients with SCIs. Therefore, it is essential for therapists to ensure they have the necessary knowledge and treatment techniques in order to do so effectively. We are also responsible to educate and inform other healthcare workers if necessary.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Galeiras Vázquez R, Rascado Sedes P, Mourelo Fariña M, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. BioMed research international. 2013;2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe. 2016 Dec 1;12(4):328-40.
- ↑ 3.0 3.1 Zakrasek EC, Nielson JL, Kosarchuk JJ, Crew JD, Ferguson AR, McKenna SL. Pulmonary outcomes following specialized respiratory management for acute cervical spinal cord injury: a retrospective analysis. Spinal cord. 2017 Jun;55(6):559-65.
- ↑ Hagen EM. Acute complications of spinal cord injuries. World journal of orthopedics. 2015 Jan 18;6(1):17.
- ↑ Armando Hasudungan. Mechanism of Breathing. Available from: https://www.youtube.com/watch?v=GD-HPx_ZG8I [last accessed 3/9/2020]
- ↑ Durbin CG. Tracheostomy: why, when, and how?. Respiratory care. 2010 Aug 1;55(8):1056-68.
- ↑ SpinalHub. How to assist cough a person with spinal cord injury. Available from: https://www.youtube.com/watch?v=lp-LBgD5Y5M [last accessed 3/10/2020]
- ↑ Jack Thompson. Percussion, vibration and shaking for clearing secretions. Available from: https://www.youtube.com/watch?v=qr-FJ3RdGuQ [last accessed 3/10/2020]
- ↑ Tamplin J, Berlowitz DJ. A systematic review and meta-analysis of the effects of respiratory muscle training on pulmonary function in tetraplegia. Spinal Cord. 2014 Mar;52(3):175-80.
- ↑ Jimmy McKanna - RT Clinic. RT Clinic : CPAP vs. BiPAP What is the difference. Available from: https://www.youtube.com/watch?v=jmQ-B40_8NU [last accessed 3/10/2020]