Angiotensin Inhibitors and Blockers for Treating Hypertension
Introduction[edit | edit source]
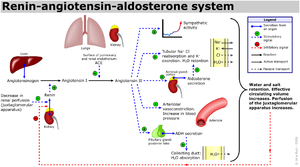
Renin-angiotensin-aldosterone system (RAAS) inhibitors are a group of drugs that act by inhibiting the renin-angiotensin-aldosterone system (RAAS) and include angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs), and direct renin inhibitors.
They are used frequently in the treatment of various conditions including hypertension and are of particular importance in hypertensive diabetic patients, as they prevent the development of diabetic nephropathy.[1]
Historic perspective[edit | edit source]
Drugs that inhibit the renin-angiotensin system, such as angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor antagonists, have proven value for the treatment of hypertension, heart failure and renal disease. ACE inhibitors being invented first then ARBs were invented to prevent the side effects of ACE inhibitors. They reduce the rates of death, myocardial infarction and stroke in a broad range of patients at high risk, but do not control the blood pressure in all cases. This led to research into inhibiting the renin-angiotensin system at its first step – the production of angiotensin and the newest type (direct renin inhibitors) that still require their direct comparison in clinical outcome studies.[2]
Pharmacodynamics:[edit | edit source]
Renin-Angiotensin System Inhibitors are valuable drugs in the treatment of hypertension due to their low side effect profile as compared to other drugs.This article will only discuss ACE inhibitors and ARBs. Angiotensin-converting enzyme inhibitors target the angiotensin converting enzyme that is responsible for converting angiotensin I to angiotensin II.[3] Angiotensin-converting enzyme inhibitors (ACE-Inhibitors) modulate the amount of angiotensin II entering the circulation. Angiotensin II is a vasoconstrictor, therefore by blocking the enzyme that produces it, vasodilation occurs in small arteries and the total peripheral resistance is reduced. Due to their strong affinity for tissue ACE, ACE-inhibitors are very potent vasodilators. Vasodilation occurs and blood pressure is lowered, yet cardiac output and heart rate remain the same.[4] Inhibition of ACE also promotes the accumulation of bradykinins that leads to an increase in vasodilator activity, thereby increasing the overall effect of the drug.[3] A common criticism of ACE-Inhibitors is that they fail to suppress angiotensin II alternative enzymatic pathways that counteract therapeutic effects.[4] As a result, Angiotensin II receptor blockers were introduced. Angiotensin II receptor blockers (ARB’s) are an angiotensin II antagonist at the type 1 receptor (AT1). ARB’s have a very high affinity for AT1 and these receptors are highly concentrated in tissues such as smooth muscle cells, kidneys, and the heart.[3]
Pharmacokinetics:[edit | edit source]
The half-lives of ACE-Inhibitors and ARB’s depends on the specific drug. ACE-Inhibitors range from 2.2 to 15 hours. ACE-Inhibitors bind to tissues and plasma protein, which means that plasma concentrations are longer lasting and have a longer elimination phase.[3] ACE-Inhibitors are primarily excreted via the kidneys. Some ACE-Inhibitors are prodrugs, which means the compound is inactive until metabolized in the liver into the active substance allowing for increased absorption from the GI tract and prevention of the first-pass effect. Certain ACE-Inhibitors, as well as ARB’s, have been shown to be cardioprotective and cardioreparative via prevention and reversal of cardiac fibrosis.[5] ARB’s have a high absorption rate with oral administration, but their metabolism varies, some are active metabolites, and some are prodrugs.[3] Newer ARB’s are more potent with a slow dissociation, therefore they have longer half-lives and only require one daily dose as opposed to older ARB’s that require two doses to maintain BP levels.[4][6]
Adverse Effects:[edit | edit source]
Overall, ACE-Inhibitors and ARB’s are well-tolerated drugs. Some side effects of ACE-Inhibitors include a dry, non-productive cough, anemia, and functional renal insufficiency.[4] Non-productive cough occurs in about 15% of people due to the accumulation of bradykinin in the system. If the patient does not tolerate the cough well, then ARB’s are indicated.[3] Although rare, angioneurotic edema and hyperkalemia are potentially life-threatening adverse effects of ACE-Inhibitors.[4] Hyperkalemia may develop as a result of potassium retention that is mediated by the reduction of aldosterone.[3] The most common side effect of ARB’s is renal insufficiency.[4] ACE-Inhibitors and ARB’s are not recommended for patients who are pregnant, or have a history of angioneurotic edema, hyperkalemia, or bilateral renal artery stenosis.[4]
See Also Pharmacological Management of Hypertension
References:[edit | edit source]
- ↑ Amboss RAAS inhibitors Available from: https://www.amboss.com/us/knowledge/Renin-angiotensin-aldosterone_system_inhibitors (last accessed 20.6.2019)
- ↑ Australian Prescriber Renin inhibitors - mechanisms of action Available from: https://www.nps.org.au/australian-prescriber/articles/renin-inhibitors-mechanisms-of-action#conclusion (last accessed 20.6.2019)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Therapeutics. British and Irish Hypertension Society. Retrieved from https://bihsoc.org/resources/therapeutics/. Accessed November 29, 2018.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Laurent, S. Antihypertensive drugs. Pharmacological Research. October, 2017;124; 116-125. doi:10.1016/j.phrs.2017.07.026. Accessed November 29, 2018.
- ↑ Kirsten, R, Nelson, K, Kirsten, D, Heintz, B. Clinical pharmacokinetics of vasodilators. Part I. Clinical Pharmacokinetics. June, 1998;34(6), 457–482. Retrieved from https://courseinfo.wssu.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=9646008&site=ehost-live. Accessed November 29, 2018.
- ↑ Barreras, A, Gurk-Turner, C. Angiotensin II receptor blockers. Proceedings Baylor University Medical Center. January, 2003; 16(1), 123–126. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1200815/. Accessed November 29, 2018.