Renal Cancer
Original Editors -Jason Larimore & Olivia Tefera from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Olivia Tefera, Jason Larimore, Lucinda hampton, Admin, Khloud Shreif, Elaine Lonnemann, Kim Jackson, WikiSysop, Vidya Acharya, 127.0.0.1 and Wendy Walker
Introduction[edit | edit source]
Renal (Kidney) cancer is cancer that forms in tissues of the kidneys.
Renal cancer includes:
- Renal cell carcinoma - Renal cell carcinomas (RCC) are primary malignant adenocarcinomas derived from the renal tubular epithelium and are the most common malignant renal tumour[1].
- Renal pelvis carcinoma - Renal pelvis cacinoma forms in the center of the kidney where urine collects.
- Wilms tumor - a pediatric cancer that typically develops before the age of five. [2]
Kidney cancers are one of the most important cancers, due in part to the large economic burden of metastatic kidney cancer, which has been estimated to be $1.6 billion (2006 USD) in selected countries and to globally account for more than 131,000 deaths and 342,000 incident cases each year[3].
- The etiology of kidney cancer is mainly unknown, but appears to be multifactorial in nature.[3]
- There has been little or no improvement in the burden of kidney cancer over the last 28 years. There is need for renewed efforts to reduce exposure to risk factors and to improve the prevention and early detection of this disease[3].
Epidemiology[edit | edit source]
Renal cancers globally account for more than 131,000 deaths and 342,000 incident cases each year[3] Renal cell cancers represent 80-90% or these.
Renal cell carcinomas
- Thought to be the 8th most common adult malignancy
- Represent 2% of all cancers
- Account for 80-90% of primary malignant adult renal neoplasms
- Patients are typically 50-70 years of age at presentation 1,2, with a moderate male predilection of 2:1 2.[1].
The most common renal neoplasm in adults is renal cell carcinoma. RCC accounts for close to 90% of all renal neoplasms and approximately 3% of all cancers.[4]
Risk Factors[edit | edit source]
A number of different risk factors have been studied, some of which are modifiable (creating an opportunity for primary prevention).
The risk factors for kidney cancer have been categorized as:
- Life style risk factors—tobacco smoking, excess body weight, alcohol consumption, physical activity and diet
- Medical history—hypertension, chronic kidney diseases, kidney stones, dialysis-related cystic disease, treatment with cyclophosphamide (chemotherapy agent), post renal transplant [1] and diabetes mellitus[3]
- Environmental and occupational exposures—trichloroethylene and aristolochic acid
- Genetic risk factors and others
Characteristics/Clinical Presentation[edit | edit source]
Presentation is classically described as the triad of:
- Macroscopic haematuria: 60%
- Flank pain: 40%
- Palpable flank mass: 30-40%[1]
This triad is however only found in 10-15% of patients
- Increasingly the diagnosis is being made on CT for assessment of haematuria alone or as an incidental finding.
- The majority of cases are sporadic.
- In contemporary medicine, almost half of all identified renal cell carcinomas are found incidentally on imaging performed for other purposes[1].
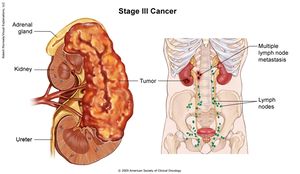
About 25-30% of patients have metastatic disease at the time of diagnosis. Renal cancer most often spreads to the lungs (75%), regional lymph nodes (65%), bones (40%), and liver (40%).[5] The patient may complain of a cough or bone pain secondary to metastasis to the lungs or bone, respectively.
The 1 minute video below outlines the presentation
Pathology[edit | edit source]
Renal cell carcinoma (RCC), or renal cancer, is categorized into four major types, determined by cellular origin:
- Clear cell : 70-80%, arises from proximal convoluted tubules
- Papillary : 13-20%, arises from distal convoluted tubules
- Chromophobe : 5%, arises from intercalated cells of collecting ducts[1]
- Collecting duct : 1% of cases [5]
Grading[edit | edit source]
Histological nuclear grading
- The most widely used and most predictive grading system for renal cell cancer is the "Fuhrman nuclear grade" which is on a scale of I-IV, where grade I carries the best prognosis and grade IV the worst.
Diagnostic Tests[edit | edit source]
The following tests and procedures may be used:
- Physical exam and health history
- Ultrasound exam
- Blood tests: An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Urinalysis
- CT scan (CAT scan): A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging) - This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Biopsy - a thin needle is inserted into the tumor and a sample of tissue is withdrawn[7].
Treatment Overview[edit | edit source]
Patients with renal cell cancer may work with a team of health care professionals to coordinate their care.eg Urologist, Surgeon, Urologic Oncologists, Medical Oncologists, Radiation Oncologists, Oncology Nurse, Registered Dietician[8]
There are different types of treatment for patients with renal cell cancer. Five types of standard treatment are used:
- Surgery
- Radiation therapy
- Chemotherapy
- Immunotherapy
- Targeted therapy[7]
RCC is primarily treated by surgical interventions. Although aggressive, a radical nephrectomy is the preferred method of treatment for both localized and metastasized diseased. This consists of the removal of:
- Kidney
- Gerota’s fascia : fibroareolar tissue surrounding the kidney and perirenal fat
- Adrenal gland
- Regional lymph nodes
Kidney cancer is rarely curable once it has spread to other organs at the time of diagnosis. Targeted agents are currently considered as the standard treatment for advanced kidney cancer that has spread to other organs. [9]
- Targeted therapies, which work by targeting the cancer at a cellular level, have expanded the options for the treatment of kidney cancer. Targeted treatments block specific abnormal signals present in kidney cancer cells that allow them to grow. These medications have shown promise in treating kidney cancer that has spread to other areas of the body. The targeted medications Axitinib (Inlyta), Bevacizumab (Avastin), Pazopanib (Votrient), Sorafenib (Nexavar) and Sunitinib (Sutent) block signals that play a role in the growth of blood vessels that provide nutrients to cancer cells and allow cancer cells to spread. Temsirolimus (Torisel) and Everolimus (Afinitor) are targeted medications that block a signal that allows cancer cells to grow and survive. Targeted therapy medications can cause serious side effects, such as: a severe rash, diarrhea, and fatigue
- Whereas targeted therapies specifically block the renal cancer cells from growing and spreading, immunotherapy works in a more general way by using the body's immune system to fight the cancer. Immunotherapy medications include Interferon and Aldesleukin (Proleukin), which are synthetic versions of chemicals made in your body. Side effects of these medications include: chills, fever, nausea, vomiting and loss of appetite.
Physical Therapy Management[edit | edit source]
Maintaining physical strength is important while undergoing renal cancer treatment and a physical therapist will be able to provide an exercise plan specifically designed for a patient’s needs.
- If a patient had surgery to remove the tumor, modest exercise can help regain muscle tone and help to rebuild the muscles that were cut, increase that patient’s range of motion, and help to prevent complications that can occur post-surgery such as: respiratory infection, pressure sores, and the formation of a deep vein thrombosis (DVT).[10]
- Exercise can have the additional benefit of reducing stress and depression, which can be common occurrences in patients undergoing cancer treatment.
- Physical therapy can also be used to combat fatigue, which is not only a common symptom of renal cancer but it can be a side effect of treatment (e.g. chemotherapy)[10]. Building up endurance can reduce the incidence and severity of fatigue. This will be an important factor in increasing a patient’s independence and ability to maintain a high quality of life.
- Educate the patient regarding his or her diet, which will play an important role throughout the treatment process.
- A systematic review and meta-analysis of randomized clinical trials suggested that intradialytic exercise protocols had positive outcomes in chronic kidney disease patients with poor cardiopulmonary function and reduced exercise tolerance and ventilatory efficiency[11].
Case Reports/ Case Studies[edit | edit source]
- Sciatica leading to the discovery of a renal cell carcinoma
- Atypical presentations and rare metastatic sites of renal cell carcinoma: a review of case reports
- Hereditary leiomyomatosis and renal cell cancer presenting as metastatic kidney cancer at 18 years of age: implications for surveillance
- Renal cancer and Wegener's granulomatosis: a case report
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Radiopedia Renal cell carcinoma Available from:https://radiopaedia.org/articles/renal-cell-carcinoma-1 (last accessed 1.9.2020)
- ↑ National Cancer Institute. Kidney Cancer. http://www.cancer.gov/cancertopics/types/kidney (accessed 11 Feb 2013).
- ↑ 3.0 3.1 3.2 3.3 3.4 Safiri S, Kolahi AA, Mansournia MA, Almasi-Hashiani A, Ashrafi-Asgarabad A, Sullman MJ, Bettampadi D, Qorbani M, Moradi-Lakeh M, Ardalan M, Mokdad A. The burden of kidney cancer and its attributable risk factors in 195 countries and territories, 1990–2017. Scientific RepoRtS. 2020 Aug 17;10(1):1-20.Available from: https://www.nature.com/articles/s41598-020-70840-2#Sec15 (last accessed 1.9.2020)
- ↑ Patel C, Ahmed A, Ellsworth P. Renal cell carcinoma. Urol Nurs 2012;32:182-190. http://www.medscape.com/viewarticle/769848 (accessed 30 Jan 2013).
- ↑ 5.0 5.1 Goodman CC, Fuller KS. Pathology: Implications for the physical therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier, 2009.
- ↑ O’Brien T. Symptoms of kidney cancer - James Whale Fund. [online video]. http://youtu.be/j63MyFqjBVE London: 2009. (accessed 30 Jan 2013).
- ↑ 7.0 7.1 NIH RCC Available from:https://www.cancer.gov/types/kidney/patient/kidney-treatment-pdq#Keypoint3 (last accessed 1.9.2020)
- ↑ National Cancer Institute. What you need to know about kidney cancer: Treatment. http://www.cancer.gov/cancertopics/wyntk/kidney/page8 (accessed 30 Jan 2013).
- ↑ Kidney cancer is rarely curable once it has spread to other organs at the time of diagnosis. Targeted agents are currently considered as the standard treatment for advanced kidney cancer that has spread to other organs. Available from:https://www.cochrane.org/CD011673/PROSTATE_immunotherapy-advanced-kidney-cancer
- ↑ 10.0 10.1 Kidney Cancer Association. Living with kidney cancer. http://www.kidneycancer.org/knowledge/live/living-with-kidney-cancer/ (accessed 8 Feb 2013).
- ↑ Andrade FP, Rezende PS, Ferreira TS, Borba GC, Müller AM, Rovedder PME. Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: systematic review and meta-analysis of randomized clinical trials. Scientific Reports. 2019 Dec 5;9(1):18470.
{{