Postural Instability
Original Editor - Lucinda hampton
Top Contributors - Ayodeji Mark-Adewunmi and Lucinda hampton
Introduction[edit | edit source]
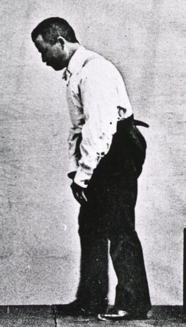
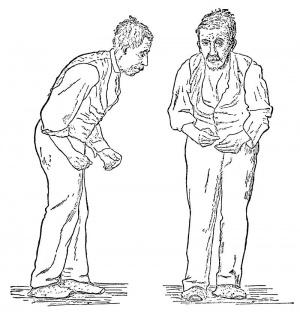
Postural instability (PI) is the inability able to maintain equilibrium under dynamic and static conditions, for example preparation of movements, perturbations, and quiet stance.
Postural instability is seen in a diverse group of conditions, most notably parkinson's and extrapyramidal diseases (eg parkinsonism, chorea, athetosis).[1] [2]
The exact pathways needed to control and maintain postural stability are not known in detail, likely involving a complex interplay of networks ranging from the spinal cord through the brainstem and cerebellum to frontal and basal ganglia circuits. Maintaining postural stability is an extraordinarily complex task, and it is therefore not surprising that cognitive impairment correlates with postural instability and falls[3]
Postural instability often leads to falls, often requiring medical assistance[4].
Etiology[edit | edit source]
Postural instability can be caused by a variety of factors, including neurological disorders such as Parkinson's disease, multiple sclerosis, and cerebellar ataxia. Other causes include musculoskeletal disorders, vestibular disorders, and medication side effects.[5]
Posture balance control is a multifactorial activity that is dependent on the integration of motor, sensory, visual, cognitive, and vestibular neural networks. A disruption in any of these circuits can lead to postural instability. The specific etiology of postural instability is difficult to identify because it is a heterogeneous disorder, and there is much ground left to uncover regarding knowledge of the pathogenesis of the disease.
In a healthy individual, balance control relies on visual, somatosensory, and vestibular information. The central nervous system aggregates sensory signals, and subsequently, a corrective motor response is produced. Slower visual processing speed, disturbances in visuospatial orientation, and decreased visual acuity, as seen in Parkinson disease, can create impediments in motor function and the ability to stabilize posture. Along with visual inputs, vestibular and proprioceptive cues are necessary to maintain an upright stance. Vestibular receptors detect deviations and accelerations in head orientation. In Parkinson disease, tilting reactions are impaired, which suggests that labyrinthine postural reactions are centrally integrated with the basal ganglia. Vestibular dysfunction, however, does not appear to fully explain postural deficits in patients with a mild to moderate degree of Parkinson disease.[6]
Somatosensory system input for postural stability involves the conscious perception of passive or active motion and direction of movements, and the processing of proprioceptive information from muscle spindles and cutaneous and joint receptors. The basal ganglia are known to be involved in the integration of proprioceptive signals for the coordination of posture and movement. Proprioception is significant in controlling postural reactions induced by unexpected stimuli.[7]
Epidemiology[edit | edit source]
Postural instability is more common in the elderly population, with an estimated 30% of adults over the age of 65 experiencing falls each year. The incidence of falls increases with age, and women are more likely to experience falls than men.
Postural instability is generally associated with Parkinson disease, which is the most common neurodegenerative disease following Alzheimer disease. The prevalence of Parkinson disease in the general population is 0.3% and 1% in people older than 65 years of age. Postural instability occurs in approximately 16% of Parkinson disease patients. Falls resulting from postural instability occur in approximately 60% of patients with Parkinson disease. Internationally, falls and fractures are the reason for about 75% of the total hospitalizations in patients with Parkinson disease.
Clinical Signs and Symptoms[edit | edit source]
The clinical signs and symptoms of postural instability include poor balance, unsteady gait, difficulty standing or walking, frequent falls, and fear of falling. Patients may also experience dizziness, vertigo, or disorientation. These symptoms can significantly impact the patient's quality of life and lead to social isolation, depression, and decreased physical activity.
Differential Diagnosis[edit | edit source]
Postural instability has a limited diagnostic specificity, given that it can result from a variety of issues in afferent pathways, efferent pathways, musculoskeletal function, and central processing. In addition to Parkinson disease which is usually linked with postural instability, the differential diagnosis should include lower motor neuron syndromes, severe spasticity, normal pressure hydrocephalus, vestibular dysfunction, atypical parkinsonian disorders, and orthostatic hypotension.
Distinguishing postural instability from orthostatic hypotension takes into account symptomatology and changes in blood pressure with the latter. Dizziness from orthostatic hypotension is usually related directly to changes in position and is associated with fainting or lightheadedness. In contrast, dizziness from postural instability usually occurs when a patient reaches, bends, or turns. Many patients with frequent falls due to postural instability may have no subjective complaints of dizziness.[8]
Progressive supranuclear palsy (PSP) is the most common atypical parkinsonian disorder. Characteristic features of PSP include vertical supranuclear gaze palsy (patient unable to look down), postural instability with unexplained falls, dysarthria, dysphagia, and frontal cognitive dysfunction. However, Postural instability is the most frequent symptom presentation in PSP. Both postural instability and falls are the most common initial symptoms of PSP, and the two are required for the diagnosis of the disease. While postural instability is a late symptom of Parkinson disease and may sometimes indicate severe parkinsonism, it is generally an early symptom of PSP.[9]
Corticobasal degeneration presents with an asymmetrical akinetic–rigid syndrome that is similar to Parkinson disease, the positional or postural limb instability, however, is usually present upon initial evaluation.
Dementia with Lewy bodies may present with postural instability similar to Parkinson disease. However, visual hallucinations and fluctuations in a patient's attention and awareness are significant features in the diagnosis of this disease.[10]
Vertigo can also present with postural instability. However, these patients are more likely to complain of dizziness. Severe postural instability with frequent falling and other neurological signs such as ataxia, dysarthria, dysphagia, or diplopia suggests central vertigo (central nervous system etiology). Unidirectional instability preserved walking, and possible tinnitus or deafness would suggest peripheral vertigo.
Testing Postural Instability[edit | edit source]
The Retropulsion Test is the gold standard to evaluate postural instability. The test involves a rapid balance perturbation in the backward direction. The number of balance correcting steps (or total absence of) is used to rate the degree of postural instability. Taking three or more steps is generally considered to be abnormal, and taking more than five steps is regarded as being clearly abnormal.
Response to backward perturbation
- Healthy subjects correct such perturbations with either one or two large steps, or without taking any steps, hinging rapidly at the hips while swinging the arms forward as a counterweight.
- Patients with postural instability, balance correcting steps are often too small, patients then need to take more than two steps.
- Noticeably affected patients continue to step backward never regaining their balance and must be caught by the examiner.
- Most markedly affected patients fail to correct, and fall backward like a dummy, without taking any corrective steps.[11]
Physiotherapy Management[edit | edit source]
Physiotherapy interventions are effective in improving balance in patients, when used in combination, not as a stand alone intervention. A combination of the below proves effective.
- Balance training (highly challenging balance training should be included)
- Muscle strengthening
- Range of movement exercises
- Gait training (incremental speed-dependent treadmill training if appropriate)[12]See Gait Re-education in Parkinson's
See Parkinson's - Physiotherapy Management and Interventions
References[edit | edit source]
- ↑ Medical Dictionary Extrapyramidal Syndrome Available:https://medical-dictionary.thefreedictionary.com/extrapyramidal+syndrome (accessed 4.11.2022)
- ↑ Djaldetti R, Lorberboym M, Melamed E. Primary postural instability: a cause of recurrent sudden falls in the elderly. Neurological sciences. 2006 Dec;27(6):412-6. Available:https://pubmed.ncbi.nlm.nih.gov/17205226/ (accessed 4.11.2022)
- ↑ Becker D, Maric A, Schreiner SJ, Büchele F, Baumann CR, Waldvogel D. Onset of Postural Instability in Parkinson’s Disease Depends on Age rather than Disease Duration. Parkinson’s Disease. 2022 Dec 2;2022.
- ↑ Appeadu M, Gupta V. Postural Instability. 2020 Available:https://www.ncbi.nlm.nih.gov/books/NBK560906/ (accessed 4.11.2022)
- ↑ Palakurthi B, Burugupally SP. Postural instability in Parkinson’s disease: a review. Brain sciences. 2019 Sep 18;9(9):239.
- ↑ Appeadu MK, Gupta V. Postural Instability.
- ↑ Rinalduzzi S, Trompetto C, Marinelli L, Alibardi A, Missori P, Fattapposta F, Pierelli F, Currà A. Balance dysfunction in Parkinson’s disease. BioMed research international. 2015 Oct;2015.
- ↑ Hillen ME, Wagner ML, Sage JI. “Subclinical” orthostatic hypotension is associated with dizziness in elderly patients with Parkinson disease. Archives of physical medicine and rehabilitation. 1996 Jul 1;77(7):710-2.
- ↑ Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Archives of neurology. 1999 Jan 1;56(1):33-9.
- ↑ Ali K, Morris HR. Parkinson's disease: chameleons and mimics. Practical neurology. 2015 Feb 1;15(1):14-25.
- ↑ NIH Postural Instability Available:https://www.ncbi.nlm.nih.gov/medgen/334529 (accessed 4.11.2022)
- ↑ Yitayeh A, Teshome A. The effectiveness of physiotherapy treatment on balance dysfunction and postural instability in persons with Parkinson’s disease: a systematic review and meta-analysis. BMC sports science, medicine and rehabilitation. 2016 Dec;8(1):1-0. Available:https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-016-0042-0 (accessed 4.11.2022)