Polycystic Kidney Disease
Original Editors - Emily Smith Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Smith, Vidya Acharya, Elaine Lonnemann, Lucinda hampton, Kim Jackson, Admin, 127.0.0.1, WikiSysop, Aminat Abolade and Wendy Walker
Definition/Description[edit | edit source]
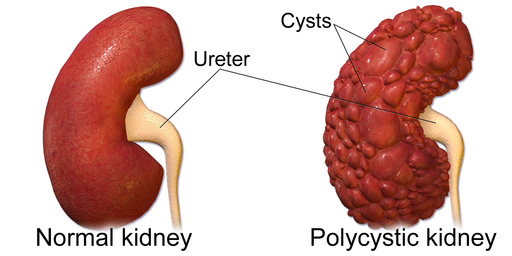
Polycystic Kidney Disease (PKD) is a genetic kidney disease which causes large benign cysts to form on the kidneys. The cysts are fluid-filled cavities that can ultimately impede kidney function leading to a degeneration of renal tissue and renal failure. Cysts can range anywhere from microscopic in size to several centimetres in diameter.[1] A cyst begins as a protrusion of the nephron and can occur anywhere along its length. Most cysts detach from the nephron, and eventually enlarge and fill with either clear fluid or fluid that contains blood or white blood cells.[2]
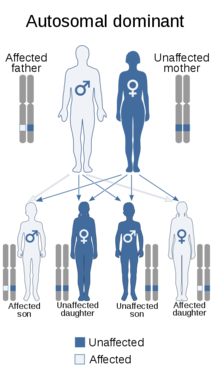
There are two types of PKD; autosomal dominant and autosomal recessive. Autosomal dominant PKD, or ADPKD, is the most common form of PKD and typically manifests itself in middle-aged adults while autosomal recessive PKD is less common and typically manifests itself in childhood. Autosomal recessive PKD is the more serious form and often leads to death in infancy or early childhood.[3] For a person to inherit ADPKD, it takes a mutated gene from only one parent, while it takes a mutated gene from both parents for a person to inherit ARPKD.[2]

|
Prevalence[edit | edit source]
ADPKD affects approximately 600,000 Americans; however, the number could actually be higher as many adults who have PKD do not yet exhibit symptoms.[4] Each child born to a parent with the gene for ADPKD has a 50% chance of inheriting the disease.[3] Approximately 10% of those in end-stage renal failure have ADPKD.[1]
Aetiology[edit | edit source]
A positive family history of PKD is reported in approximately 75% of cases. [1] ADPKD results from a genetic mutation on the short arm of chromosome 16. [1] According to the PKD Foundation website, 85% of mutations in ADPKD occur in chromosome 16 (PKD1 gene) while 15% of mutations in ADPKD occur in chromosome 4 (PKD2 gene). [5]
Image found at http://www.pkdcure.org/tabid/1354/Default.aspx.
Mutations in either the PKD1 or PKD2 gene can cause autosomal dominant polycystic kidney disease; PKD1 gene mutations cause ADPKD type 1, and PKD2 gene mutations cause ADPKD type 2. The PKD1 and PKD2 gene provide instructions for making a protein called polycystin-1 and polycystin-2, which is found in the kidneys before birth and in many adult tissues. These genes provide instructions for making proteins whose functions are not fully understood. Researchers believe that they are involved in transmitting chemical signals from outside the cell to the cell's nucleus. The two proteins work together to promote normal kidney development, organization, and function. Mutations in the PKD1 or PKD2 gene lead to the formation of thousands of cysts, which disrupt the normal functions of the kidneys and other organs. People with mutations in the PKD2 gene, particularly women, typically have a less severe form of the disease than people with PKD1 mutations. The signs and symptoms, including a decline in kidney function, tend to appear later in adulthood in people with a PKD2 mutation.
The PKHD1 gene provides instructions for making a protein called fibrocystin, which is present in fetal and adult kidney cells[6] and is also present at low levels in the liver and pancreas. Mutations in the PKHD1 gene cause autosomal recessive polycystic kidney disease. This gene provides instructions for making a protein whose exact function is unknown; however, the protein likely transmits chemical signals from outside the cell to the cell nucleus. Researchers have not determined how mutations in the PKHD1 gene lead to the formation of numerous cysts characteristic of polycystic kidney disease.
Although polycystic kidney disease is usually a genetic disorder, a small percentage of cases are not caused by gene mutations. These cases are called acquired polycystic kidney disease. This form of the disorder occurs most often in people with other types of kidney disease who have been treated for several years with hemodialysis (a procedure that filters waste products from the blood).
Systemic Involvement[edit | edit source]
PKD affects the excretory system, cardiovascular system, and digestive system[7].
Excretory system
The kidneys act as the major filters of the blood. According to the PKD Foundation website, "the kidneys filter approximately 200 quarts of blood daily, reabsorb 98% of the filtrate and regulate the composition of the blood by removing waste...".Additional kidney functions include the production of three hormones: erythropoietin, renin, and calcitriol. Renin is a very important hormone in the regulation of blood pressure.
Cardiovascular system
PKD affects the cardiovascular system, because, as previously mentioned, it puts the person at risk for hypertension, intracranial aneurysms, and MVP. The fluid filled cysts on the kidneys create a reduction in blood flow which the body attempts to correct by releasing angiotensin II. Angiotensin II causes vasoconstriction thereby increasing blood pressure to in turn increase blood flow. However, the decreased blood flow cannot be corrected due to the pathology of the kidneys, so a "broken feedback loop" ensues. Persistent, long term hypertension can lead to heart damage if left untreated. According to the PKD Foundation website, "approximately 50% of PKD patients die from the heart and vascular complications of PKD, not renal failure."
Digestive/Gastrointestinal system
The liver is the most common site for extra renal cysts to develop; however, cysts can also form on the pancreas. According to the PKD Foundation website, "Current research suggests that liver cysts form from cells lining the bile ducts or tubules of the liver rather than the liver cells themselves." These cysts displace the liver tissue but do not destroy it which is why the liver enlarges but remains relatively functional. Another gastrointestinal complication of ADPKD is diverticulosis. Diverticulosis involves a deformation of the colon and occurs more often in people with PKD who are on dialysis or have had a kidney transplant than any other kidney disease. Also, these people tend to have more complications from diverticulosis such as infection known as diverticulitis.
Associated Co-morbidities[8][edit | edit source]
High blood pressure.
Loss of kidney function.
Pregnancy complications.
Growth of cysts in the liver.
Development of aneurysm in the brain.
Heart Valve abnormalities.
Colon problems.
Chronic pain.
Characteristics/Clinical Presentation[edit | edit source]
People with ADPKD may not know they have the disease because their symptoms have not yet manifested themselves. ADPKD signs and symptoms typically begin to show themselves between the ages of 30 and 40.[4]
Symptoms/Signs for PKD include[8]:
• high blood pressure
• back or side pain related to enlarged kidneys
• headache( see Figures 4 and 5)
• blood or protein in the urine
• frequent urination
• kidney stones
• kidney failure
• urinary tract or kidney infections
Symptoms that are also associated with PKD include[3]:
• drowsiness
• joint pain
• nail abnormalities
• painful menstruation
Diagnostic Tests[edit | edit source]
A urinalysis can be used to determine if there is blood or protein in the urine. [1] If the disease has progressed the enlarged kidneys may be palpable upon examination. [1] An ultrasound or CT scan can be used to determine if a malignancy is present, and surgery may be necessary to make a definitive diagnosis. [1] Genetic testing can also be done by taking and comparing a blood sample from the person and three family members who are either known to have or not have PKD. [8]
Differential Diagnosis[edit | edit source]
Below is a list of some of the symptoms of PKD. Each symptom are listed diseases that can be associated with those symptoms but do not necessarily have a relation to PKD.
- Multiple benign simple cysts, Localised renal cystic disease, Acquired renal cystic disease, Autosomal dominant medullary cystic disease[9]
- Hypertension: heart failure, stroke, MI, arterial aneurysm, diabetes[1]
- Blood in the urine: UTI, kidney infection, kidney injury, bladder cancer, STD, haemophilia, leukaemia, tuberculosis, endocarditis.
- Protein in urine: rhabdomyolysis, diabetes, HIV, preeclampsia, eclampsia, UTI, multiple myeloma
- Increase in size of abdomen/trunk: irritable bowel syndrome, constipation[10]
- Low Back Pain: constipation, ankylosing spondylitis, ascites, endocarditis, ovarian cysts, prostate cancer, sciatica, inflammatory bowel disease.
- Headache: primary neoplasm, migraine, ischemia, cerebral vascular thrombosis, subarachnoid haemorrhage, hypertension, systemic lupus erythematosus, obstructive sleep apnea, pregnancy, dysmenorrhea, cranial neuralgia, brain abscess, side effects or overuse of medications, caffeine withdrawal, hypoglycemia, fibromyalgia.
Medications[edit | edit source]
There is no cure for PKD, so the best way to manage it is by controlling or minimizing symptoms.
Controlling blood pressure is one of the most important ways to manage PKD. While it is unsure which blood pressure medications are best for the PKD patient population, many nephrologists agree that ACE inhibitors (Angiotensin Converting Enzyme inhibitors) or ARB (Angiotensin Receptor Blockers) are good medications to start with.[5] Both of these medications work via various pathways to block or inhibit angiotensin II; an enzyme that constricts the blood vessels thereby increasing blood pressure.[11] Diet, and/or exercise is a good way to slow or prevent the progression of the PKD.[1]
As stated above, urinary infections are common in people with PKD. Prompt administration of antibiotics for the management of kidney, bladder, or urinary tract infections is important for people with PKD as well as drinking plenty of fluids to dilute blood in the urine.[8]
PKD patients should avoid using all NSAID (Non-Steroidal Anti Inflammatory Agents) products such as aspirin, Advil, Aleve, etc. unless told to do so by a physician due to the negative effects on the kidneys.[5] Patients with PKD may take acetaminophen (Tylenol) for their back and flank pain.[8] Unlike NSAIDS, acetaminophen does not have the same negative effects on kidney function; however, over time, usage of acetaminophen can have negative effects on the liver.[11]
Dialysis - Those people with PKD who reach end-stage renal failure will need to undergo dialysis treatments and, ultimately, a kidney transplant. When a person undergoes dialysis, a fluid called dialysate is injected into their bloodstream.[5] This fluid is a mixture of pure water and chemicals that are circulated throughout the blood to help filter out the toxins that the kidneys can no longer filter.[5] A semi-permeable membrane with microscopic holes separates the dialysate from the blood and allows the toxins to be removed from the blood while not removing necessary substances such as protein and blood cells from the bloodstream.[5]
There are two main types of kidney dialysis: hemodialysis and peritoneal dialysis .[5] Hemodialysis involves a person being hooked up to a machine known as a dialyzer which has a man-made semi-permeable membrane which acts as the filter for the kidneys.[5] To begin hemodialysis, a person must discuss with their physician their best options for an access site or port.[5] A person can undergo hemodialysis at a dialysis centre, nocturnal hemodialysis, or daily home hemodialysis. A person who chooses to undergo hemodialysis at a dialysis centre will come to the centre 3 days a week for 3-4 hours a day to be hooked up to the dialyzer machine to have their blood filtered.[5] A person who chooses to do nocturnal hemodialysis will undergo extended treatments 3 or more nights a week while asleep.[5] Finally, if a person chooses to undergo daily home hemodialysis, they will complete 2-3 hour sessions 5-6 days a week.[5] According to the PKD Foundation website, Medicare and private insurance companies may not pay for the extra treatments needed for nocturnal and home hemodialysis.[5] Peritoneal dialysis involves a person filling their abdominal cavity with dialysate via a catheter allowing the peritoneal membrane to act as the semi-permeable membrane.[5] The dialysate stays in the abdominal cavity and pulls the waste through the peritoneal membrane for several hours.[5] The person may manually empty and refill the dialysate 4-5 times per day, or they may choose to have a machine known as a cycle do this automatically while they sleep.[5]
Physical Therapy Management[edit | edit source]
Though there is no cure for PKD, there has been research that shows that exercise can help decrease or manage symptoms on people with chronic kidney disease. (Renal Rehabilitation is an emerging therapy) Many of these studies look at the effect of exercise on the proteinuria, glomerular filtration rate (GFR) and blood pressure. One study found that a 12-week aquatic exercise program improved cardiorespiratory functional parameters, resting blood pressure, proteinuria, and the GFR in patients with chronic kidney disease.[12]
Strength Training[edit | edit source]
Another study looked at the effects of strength training in elderly patients in the predialysis phase.[13] The authors of the study found that after completion of a 12-week exercise program that included resistance training with 60% of the person’s 1 RM, there was no difference in muscle fibre area or fibre type between the exercise group and the control group which was sedentary.[13] However, there were no disadvantageous effects in the histopathology of the muscle in the exercise group.[13] Thus the authors concluded that 60% of the patient’s 1RM is sufficient to build strength and endurance in the patient population but not to increase muscle fibre area or muscle fibre type.[13]
Exercise Program[edit | edit source]
A systematic review and meta-analysis of randomized clinical trials suggested that intradialytic exercise protocols had positive outcomes in chronic kidney disease patients with poor cardiopulmonary function and reduced exercise tolerance and ventilatory efficiency[14].
A third study questioned the number of dialysis patients who might benefit from an exercise program while in the hospital.[15] The authors also looked at the number of patients who adhered to the program as well as the effect of the exercise on the patients’ “10-m shuttle walk test, haemoglobin, body mass index, urea reduction ratio, nutritional status and nine domains of quality of life using the Short Form 36 (SF36) questionnaire”.[15] The results of the study showed that approximately 50% of the hospital haemodialysis patients were interested and able enough to start a dialysis cycling program three times a week.[15] The percentage of the patients that continued the program after 2 months was slightly less than 80% of the starting number.[15] The patients who continued to exercise showed a significant improvement of their walking distance on the shuttle walk test which was correlated with an “improvement in well-being as judged by the quality-of-life scores”.[15] According to the study, “there were no important changes in haemoglobin, nutritional status or effectiveness of dialysis during the 8 weeks of study”.[15]
Dietary Management[edit | edit source]
One way of slowing the progression of PKD is by managing the diet. Many people manage the disease by eating low sodium and low protein diet and drinking lots of fluids. A person with chronic kidney disease may have lab work done to determine which nutrients are and are not being processed properly. With this information, the person may choose to visit a renal dietician to discuss a specific diet customized for the person’s needs.[17] Fluid intake is also important in the management of PKD and should be discussed with a nephrologist. People with PKD lose the ability to absorb water efficiently early on in the disease process. Therefore, a person with PKD may easily become dehydrated during strenuous exercise or extreme heat. A person who is undergoing dialysis must also monitor fluid intake based on the amount of urine produced and the type of dialysis they are using. If the person is no longer urinating, fluid intake should be limited to 1 litre per day.
Researchers suggests potential use of nutraceutical for the treatment of autosomal dominant polycystic kidney disease. Several natural compounds, such as triptolide, curcumin, ginkolide B, and steviol (stevia extract) have been shown to be able to retard cyst progression in ADPKD[18].
Resources[edit | edit source]
PKD Foundation: http://www.pkdcure.org
National Kidney Foundation: http://www.kidney.org
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Goodman CC, Fuller KS, Boissonnault WG. Pathology: implications for the physical therapist. 2nd ed. Philadelphia, PA: Saunders; 1998.
- ↑ 2.0 2.1 PKD Foundation. What is PKD? https://pkdcure.org/what-is-pkd/
- ↑ 3.0 3.1 3.2 National Center for Biotechnology Information, U.S. National Library of Medicine. Polycystic kidney disease. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001531 (accessed 5 March 2011).
- ↑ 4.0 4.1 National Kidney Foundation. Polycystic Kidney Disease. http://www.kidney.org/atoz/content/polycystic.cfm (accessed 5 March 2011).
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 PKD Foundation. The Science of PKD.https://pkdcure.org/living-with-pkd/dialysis/ (accessed 5 MaY 2019).
- ↑ U.S National Library of Medicine. Genetic Home Reference,Polycystic kidney disease.Accessed on 05/05/19 https://ghr.nlm.nih.gov/condition/polycystic-kidney-disease#genes
- ↑ PKD Foundation, Complications https://pkdcure.org/what-is-pkd/adpkd/what-are-the-related-health-complications/Accessed on 13.05.19.
- ↑ 8.0 8.1 8.2 8.3 8.4 Mayo Clinic. Polycystic kidney disease. http://www.mayoclinic.com/health/polycystic-kidney-disease/DS00245/DSECTION=symptoms (accessed 5 March 2011).
- ↑ Alves M, Fonseca T, de Almeida EA. Differential diagnosis of autosomal dominant polycystic kidney disease. InPolycystic Kidney Disease [Internet] 2015 Nov. Codon Publications.
- ↑ Goodman CC, Snyder TE. Differential Diagnosis for physical therapists: screening for referral. 4th ed. St. Louis, MO: Saunders Elsevier; 2000.
- ↑ 11.0 11.1 Mayo Clinic. Acetaminophen (Oral Route, Rectal Route). http://www.mayoclinic.com/health/drug-information/DR601885 (accessed 5 March 2011).
- ↑ Pechter U, Ots M, Maaroos J, et al. Beneficial effects of water-based exercise in patients with chronic kidney disease. International Journal of Rehabilitation Research [serial online]. June 2003;26(2):153-156. Available from: CINAHL with Full Text, Ipswich, MA. Accessed March 5, 2011.
- ↑ 13.0 13.1 13.2 13.3 Heiwe S, Clyne N, Tollbäck A, Borg K. Effects of Regular Resistance Training on Muscle Histopathology and Morphometry in Elderly Patients With Chronic Kidney Disease. American Journal of Physical Medicine & Rehabilitation [serial online]. November 2005;84(11):865-874. Available from: Academic Search Premier, Ipswich, MA. Accessed March 5, 2011.
- ↑ Andrade FP, Rezende PS, Ferreira TS, Borba GC, Müller AM, Rovedder PME. Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: systematic review and meta-analysis of randomized clinical trials. Scientific Reports. 2019 Dec 5;9(1):18470.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 Torkington M, MacRae M, Isles C. Uptake of and adherence to exercise during hospital haemodialysis. Physiotherapy [serial online]. June 2006;92(2):83-87. Available from: SPORTDiscus with Full Text, Ipswich, MA. Accessed March 5, 2011.
- ↑ PKD Foundation. Good Activities for People with Polycystic Kidney Disease (PKD). Available from: http://www.youtube.com/watch?v=kW_vY7DGRuI&NR=1 [last accessed 7 March 2011]
- ↑ PKD Foundation. The Science of PKD.https://pkdcure.org/living-with-pkd/nutrition/
- ↑ Yuajit C, Chatsudthipong V. Nutraceutical for Autosomal Dominant Polycystic Kidney Disease Therapy. Journal of the Medical Association of Thailand= Chotmaihet thangphaet. 2016 Jan;99:S97-103.
- ↑ PKD Foundation. Drinking Water and Polycystic Kidney Disease. Available from: http://www.youtube.com/watch?v=2_RCEwDvRfk [last accessed 7 March 2011]