Pneumothorax
Original Editor - The Open Physio project.
Top Contributors - Abbey Wright, Siobhán Cullen, Admin, SULEIMAN USMAN, Eugenie Lamprecht, Kim Jackson, Nikhil Benhur Abburi, Rachael Lowe, WikiSysop, Karen Wilson, Vidya Acharya, Claire Knott, Lucinda hampton and Shreya Pavaskar
Definition[edit | edit source]
According to the Oxford Concise Medical Dictionary,a pneumothorax can be defined as "Air in the pleural cavity". This occurs when there is a breach of the lung surface or chest wall which allows air to enter the pleural cavity and consequently cause the lung to collape.
Various causes of a pneumothorax exist and each pneumothorax is classified according to its cause. A spontaneous pneumothorax, also referred to as a primary or primary spontaneous pneumothorax, is characterised by having no clear cause or no known underlying lung pathology. There may be contributing factors, such as cigarette smoke, family history,the rupture of bulla(small air filled sacs in the lung tissue) but these will not cause of the pneumothorax itself. A non-spontaneous, secondary or complicated pneumothorax occurs as a result of an underlying lung pathology such as COPD, Asthma, Tuberculosis, Cystic Fibrosis or Whooping Cough.
A pneumothorax can further be classified as a tension or non-tension pneumothorax. A tension pneumothorax is caused by excessive pressure build up around the lung due to a breach in the lung surface which will admits air into the pleural cavity during inspiration but will not allow any air to escape during expiration. The breach acts as a one-way valve. This leads to lung collapse. The removal of the air is through surgical incision by inserting a under water drain in the pleural cavity. This excessive pressure can also prevent the heart from pumping effectively which may lead to shock. A non-tension pneumothorax is not considered as severe as there is no ongoing accumulation of air and therefore there is no increasing pressure on the organs and the chest.
Other causes of a pneumothorax can be trauma or incorrect medical care.A traumatic pneumothorax is caused by trauma to the lungs. Some of the causes are the following: Stabwound, gunshot or injury from a motor vechicle accident or any other traume to the lungs. A pneumothorax which develops as a result of a medical procedure or incorrect medical care i.e. accidental puncture to the lung during surgery, is termed as an iatrogenic pneumothorax.
Causes and risk factors[edit | edit source]
Spontaneous pneumothorax may be caused by a rupture of a cyst or a small air sac (bulla) on the surface of the lung whereas, a complicated pneumothorax may occur following an injury to the chest wall such as a fractured rib, any penetrating injury (gun shot or stabbing), surgical invasion of the chest, or may be deliberately induced in order to collapse the lung. A pneumothorax can also occur as a result of medical procedures, for example, insertion of a central venous catheter in the jugular or subclavian vein as well as from mechanical ventilation, emphysema and rarely but possibly as a result of pneumonia.
Primary Spontaneous Pneumothorax (PSP)is thought to be related to increased shear forces in the apex. It is associated with the pressure of apical pleural blebs lying under the visceral pleura, however the exact site of air leakage is unknown. Lung inflammation and oxidative stress is important to the pathogenesis of PSP.
Secondary Spontaneous Pneumothorax (SSP) occurs in the presence of lung disease, primarily being Chronic Obstructive Pulmonary Disease (COPD). Other lungs diseases include Tuberculosis (TB), Cystic Fibrosis and Idiopathic pulmonary fibrosis.
Tension Pneumothorax occurs in intensive care settings in patients who are ventilated. Air is trapped in the pleural space and positive pressure rises. This pressure compresses the mediastinum and therefore decreases venous return to the heart and reducing the cardiac output. It also results in ipsilateral lung collapse and contralateral lung compression which leads to compramised gaseous exchange and ultimately leads to hypoxemia.
It is seen in a severe asthma attack that the air enters into the mediastinum which then ruptures into the pleural space, which in turn causes a pneumothorax
Generally, men are more at risk of developing a pneumothorax than women are. Smoking is also a major risk factor, and it is the leading factor associated with primary spontaneous pneumothorax. Smoking increases the risk of pneumothorax 20 fold in men and 10 fold in females compared to non smokers and this rises proportianallly with the number of cigarettes smoked. 90% of patients with PSP are smokers. The increased risk with increased cigarettes smoked per day is more pronounced in female smokers.
Lung inflammation and oxidative stress are part of pathogenesis of PSP. Current smokers at increased risk of PSP have increased number of inflammatory cells in the small airways. There is also growing evidence that genetic factors may be causes of PSP. Genetic disorders like Marfan Syndrome, Homocystinuria dn Birt-Hogg-Dube (BHD) syndrome. BHD is characterised by renal and colon cancer as well as spontaneous pneumothorax (22%).Other risk factors include; pregnancy and familial pneumothorax.
All age groups are affected and premature neonates on mechanical ventilation are at high risk of developing a pneumothorax.
There is always a risk of pneumothorax reoccurring.
Signs and Symptoms[edit | edit source]
Symptoms of pneumothorax include:
- Sudden onset of chest pain (This is a sharp pain, which may lead to a feeling of tightness in the chest)
- Dyspnoea (shortness of breath)
- Tachycardia (rapid heart rate)
- Tachypnoeas (rapid respiration rate)
- Coughing (dry)
- Fatigue
- Signs of respiratory distress (nasal flaring, anxiety etc)
- Hypotension
- Subcutaneous emphysema
According to Wikipedia free encyclopedia, Subcutaneous emphysema (also known as tissue emphysema) occurs when gas or air is present in the subcutaneous layer of the skin. This usually occurs in the chest, neck and face, where it can travel from the chest cavity along the fascia. There may also be cyanosis (skin develops bluish colour due to low levels of oxygen in the blood). When the pneumothorax is small, no symptoms may be present.
A Primary Spontaneous pneumothorax usually develops at rest and people often don't seek medical attention for days after their symptoms appear, where as a Secondary Pneumothorax develops more serious clinical symptoms due to commorbitity. Tension Pneumothorax also demonstrates the same signs and symptoms as above however usually shown more severly due to the rapid compression on the heart and vessels.
Prevelance around the world[edit | edit source]
According to Chang and Mukherji (2007) the incidence of primary spontaneous pneumothorax in the USA(age-adjusted) is 7.4-18 cases per 100,000 persons per year for men and 1.2-6 cases per 100,000 persons per year for women. Incidence of secondary spontaneous pneumothorax (age-adjusted) is 6.3 cases per 100,000 persons per year for men and 2 cases per 100,000 persons per year for women. Chronic obstructive pulmonary disease (COPD) is a common cause of secondary spontaneous pneumothorax that carries an incidence of 26 cases per 100,000 persons. The incidence of iatrogenic pneumothorax is not known, but it probably occurs more often than primary and secondary spontaneous pneumothoraces combined.Incidence is higher in men than in women, at a ratio of 6.2:1 for primary pneumothorax and 3.2:1 for secondary pneumothorax.
Although some view primary spontaneous pneumothorax as more of a nuisance than a major health threat, deaths have been reported. Secondary spontaneous pneumothoraces can be life threatening, depending on the severity of the underlying disease and the size of the pneumothorax. Mortality percentages in patients with COPD and spontaneous pneumothorax vary from 1-17%. Iatrogenic pneumothorax may cause substantial morbidity and, rarely, death (Chang & Mukerji, 2007).
Primary spontaneous pneumothorax occurs most often in people between age 18 - 40 and Secondary spontaneous pneumothoraces occur more frequently after age 60 years.Prevalence of a pneumothorax in a newborn is a potentially serious problem and it occurs in about 1-2% of all births.
Pathology[edit | edit source]
The lungs are located inside the chest cavity and air is drawn into the lungs by the diaphragm. The pleural cavity is the region between the chest wall and the lungs. If the air enters the pleural cavity, either from the outside (open pneumothorax) or from the lung (closed pneumothorax), the lung collapses and it becomes impossible for the person to breath, even if they have an open airway. If a piece of tissue forms a one way valve which allows air to enter the pleural cavity, but not to escape, overpressure can build up with each breath (tension pneumothorax). This leads to severe shortness of breath and circulatory collapse.
Air leaks from the lungs into other parts of the chest cavity can occur in newborns. Babies are normally born with collapsed lungs, and a large amount of pressure is generated as the newborn's body works to inflate their lungs with the first few breaths. For 98% of newborns there is no problem at all, but for some (2%)the lungs do not immediately open completely and the strong pressures generated to inflate the lung may cause small ruptures in the alveoli. The leaked air can be removed by the physician, and continual removal of this leaked air is required until the ruptures have healed.
There is a loss of intrapleural negative pressure that can result in a lung collapse. Due to this there is a decrease in vital capacity as well as a decrease in PaO2 which is the main consequence of a pneumothorax. The decrease in PaO2 results from various factors i.e low ventilation-perfusion ratios, anatomic shunts and alveolar hypoventilation. Most patients that suffer from a pneumothorax also have an increase in alveolar-arterial oxygen tension.
Diagnosis[edit | edit source]
Initially a complete medical and physical examination needs to be conducted.
On examination of the chest with a stethoscope it will be noted that there is either decreased or absent breath sounds over the area of the affected lung, which may indicate that the lung is not unfolded in the pleural cavity. There is hyperresonance (higher pitched sounds than normal) with percussion of the chest wall which is suggestive of pneumothorax diagnosis.
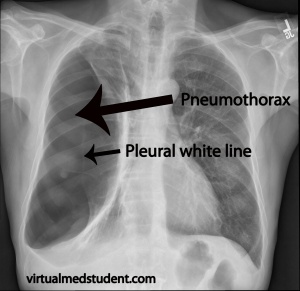
Chest x- rays will then be used to confirm the diagnosis of the pneumothorax. In a supine chest x-ray, a deep sulcus sign is diagnostic and this is characterised by a low lateral costophrenic angle on the affected side. Also the presence of air outside normal lung airways and movement or shifting of the organs away from the air leak in the thoracic cavity will be indicative of the presence of a pneumothorax.
Another procedure used is Transillumination. This is a procedure used in an emergency situation and makes use of a fiberoptic light probe that is placed on the baby's chest wall i.e. the side with the air leak will transmit a brighter light.
Diagram showing a neonate with a right tension pneumothorax. Note the tracheal deviation to the left.
Prognosis[edit | edit source]
Up to 50% of patients who suffer from a pneumothorax will have another or a recurring pneumothorax. However, there are no long-term complications after successful treatment.
Medical management[edit | edit source]
The main aim is to relieve the pressure on the lung and allow it to expand. It is of vital important to try and prevent the recurrence of a pneumothorax.
Treatment depends on the severity of the pneumothorax. If the patients lung is 20% to 25% collapsed, the doctors may choose to monitor the condition using x-rays until the lung has re-expanded. If the patients lung has collapsed more than 25%, a chest tube may be inserted into the pleural space to remove the air.
Treatment of a simple pneumothorax is given conservatively. This includes oxgygen therapy that will aid in increasing the reabsorption of the lost intrapleural air. The patient is monitored constantly and multiple chest x-rays are taken to follow the stages of healing of the pneumothorax. This type of pneumothorax is very likely to develop into a tension pneumothorax therefore the treatment becomes more invasive as a chest tube is inserted along with positive pressure ventilation to prevent lung collapse.
Types of treatment may also vary, for example, in patients that suffer from cystic fibrosis, sclerotherapy can be utilised. According to Wikipedia this is a procedure whereby medicine is injected into blood vessels that cause the vessels to shrink. This therapy is useful, however it does not take away the factor of recurrence.
The only medical interventions that can be employed are Pleurodesis, visited assisted thorascopy and thoracotomy These procedures will help minimise the recurrence of a pneumothorax.
Intercostal chest drains can also be inserted to drain air or fluid out of the pleural space to allow for expansion of the compressed lung and to prevent a build up of fluids that may lead to the development of an empyema.
Underwater chest drains ensure that the air that is removed from the pleural cavity during expiration does not re-enter the cavity during inspiration. These drains have an underwater seal on them that prevent this from occurring. The distal end of the tube is attached to the bottle and this must always be underwater. The drain is always kept below the level of the patient's chest. Gravity helps to drain fluid, and therefore it will not re-enter the pleural cavity.
Physiotherapy management[edit | edit source]
Indications for Physiotherapy
- Lung collapse
- Increased work of breathing
- Thick sputum plugs predisposing to ventilation difficulty
- Blood gas abnormalities
- Sputum retention
Goals for Physiotherapy
- To reinflate atelectatic lung areas
- To improve distribution of ventilation
- To increase oxygenation
- Maintain airway clearance
- Improve exercise tolerance
Physiotherapy Management
To reduce work of breathing
- Body positioning
- Breathing control
- Relaxation technique
To improve ventilation
- Localised thoracic expansion exercise
Sputum mobilisation techniques
- Postural drainage
- Deep breathing exercise
- Percussion, shaking and vibrations
Sputum removal techniques
- Coughing and huffing
- Airway suctioning
Physiotherapy outcome evaluation includes
- Respiratory rate
- Breathing pattern
- Sputum quantity
- Ausculatation
- Cough sound
- Oxygen requirement
- SpO2
- Arterial blood gases
- Chest x-ray changes
- Muscle strength
- Functional performance
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1HM5Uxfu7f2MxEn3rb6axoCUQHd9cly5aoDuTaX5kmvqmatgqf: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Aras Murad.Pneumothorax: What is a pneumothorax or collapsed lung. Available from: http://www.youtube.com/watch?v=i-sZzZ4TMnY [last accessed 24/6/13]
- ↑ MDChalkTalk.How a chest tube drainage system works. Available from: http://www.youtube.com/watch?v=eA_gxe8rd88 [last accessed 24/6/13]
Bascom, R.(2009). Pneumothorax. eMedicine. Retrieved February 22, 2009 from http://emedicine.medscape.com/article/424547-overview
Blaivas, A.J.(2007).Pneumothorax. Medlineplus Medical Encyclopedia. Retrieved February 22, 2009 from http://www.nlm.nih.gov/medlineplus/ency/article/000087.htm#Treatment
Chang, A. K. & Mukherji, P. (2007). Pneumothorax, Iatrogenic, Spontaneous and Pneumomediastinum. eMedicine. Retrieved April 6, 2009 from http://emedicine.medscape.com/article/808162-overview Dictionary of physiotherapy.(2005). Pneumothorax
Mayo clinic staff.(2007).Treatments and drugs. Retrieved February 22, 2009 from http://www.mayoclinic.com/health/pneumothorax/DS00943/DSECTION=treatments-and-drugs
http://student.bmj.com/back_issues/1100/education/408.html
Mamashealth.com.(2008). Pneumothorax. Retrieved April 6, 2009 from http;//www.mamashealth.com/lung/pneum.asp Mayo clinic staff. (2007). Risk factors. Retrieved February 22, 2009 from http://www.mayoclinic.com/health/pneumothorax/DS00943/DSECTION=risk-factor
Medicinenet.com. (2009). Pneumothorax. Retrieved April 6, 2009 fromhttp;//medicinenet.com/pneumothorax/page2.htm Oxford Concise Medical Dictionary.(2002). Pneumothorax.(6th ed).Oxford:Oxford University Press.p 544
Pryor, J. A. & Prasad, S. A.(2006).Physiotherapy for Respiratory and Cardiac Problem.(3rd Ed.).New york: Churchill Livingston. p 389
Pneumothorax.(2006). Retrieved February 25, 2009 from http://emedicine.medscape.com/article/1003552-overview
Pneumothorax. (2004). University of Virginia, Health system. Retrieved April 11, 2009 from www.healthsystem.virginia.edu/uvahealth/peds_hrnewborn/pnethorx.cfm.
The Health Central Network,Inc. (2001-2009). Health Encyclopedia - Diseases and Conditions.(68)Retrieved February 22, 2009 from http://www.healthscout.com/ency/68/234/main.html#TreatmentofPneumothorax
Wikipedia, The Free Encyclopedia. "Subcutaneous emphysema". Retrieved February 25, 2009 from http://en.wikipedia.org/wiki/Subcutaneous_emphysema
Wikipedia, The Free Encyclopedia. "Pneumothorax". Retrieved February 25, 2009 from http://en.wikipedia.org/wiki/Pneumothorax
Wikipedia, The Free Encyclopedia." Sclerotherapy". Retrieved February 25, 2009 from http://en.wikipedia.org/wiki/Sclerotherapy