Plantar Heel Pain
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Jess Bell, Lucinda hampton, Kim Jackson, Tarina van der Stockt and Habibu Salisu Badamasi
Introduction[edit | edit source]
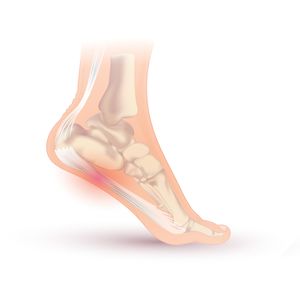
The term Plantar Heel Pain is considered more appropriate than plantar fasciitis or fasciopathy[1] because it is not the only cause of this pain.
There are several conditions that may cause plantar heel pain which could be of bony or soft tissue origins:[2]
- Skeletal problems include:
- Calcaneal stress fracture
- Apophysitis of the calcaneus (Sever’s disease)
- Osteomyelitis, or inflammatory arthropathy
2. Soft tissue pathology includes:
- Fat pad atrophy (FPA) or contusion
- Plantar fascia rupture
- Plantar fasciitis (PF).
- Nerve compression/pathology:eg
- The first branch of the lateral plantar nerve (Baxter’s nerve)
- Medial calcaneal branch of posterior tibial nerve or nerve to abductor digiti quinti muscle (see image R).
- S1 radiculopathy
- Tarsal tunnel syndrome
- Peripheral Neuropathy
Plantar heel pain is one of the most common lower limb musculoskeletal conditions that affects both sedentary and physically active people.[3] It can have a significant impacts on work and activities[4].
- Accounted for approximately one million physician consultations per year in the United States of America between 1995 and 2000[5]
- 11-18 % of people continue to report symptoms beyond 1 year following conservative management[4].
- Plantar heel pain was found to be most common in middle-aged women[6].
- The reasons for the high incidence in women are not known, however, it has been linked to early menopause. The hormonal changes are believed to attribute to a weakening of the fascia and maybe increased stress.
There is a number of risk factors found to be associated with plantar heel pain, including[7][2]:
- Prolonged standing
- Recent changing of shoe wear
- Stress
- Excessive running or suddenly increasing running distance
- Pes planus
- Limited ankle dorsiflexion
- Obesity
Patients usually use the internet to look up for education, advice and remedies for their symptoms.
- Some patients we see at the clinic may have tried strapping, rolling the foot on the ice bottle, rolling it on golf balls, and doing various stretches.
- Often they would say these treatments have been particularly painful, but they haven't made a difference to the pain.
- This drives patients to look for professional advice.
If we look at the literature, there are some pretty good studies showing that physiotherapy will have positive benefits on plantar heel pain[8]. However, when it comes to clinical practice, different measures should be considered to apply research findings properly and see positive results.
- Often, the treatment that works for a woman might differ from the treatment that works for a man.
- The level of activity is an important factor as well as the patient's history.
- Considering individual factors and using clinical reasoning skills are mandatory when it comes to the treatment of plantar heel pain and other MSK issues.
Nerve Entrapment[edit | edit source]
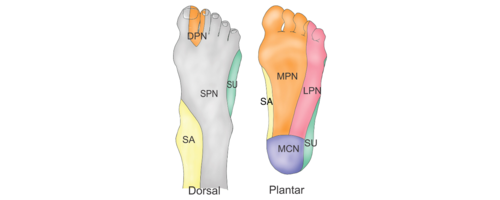
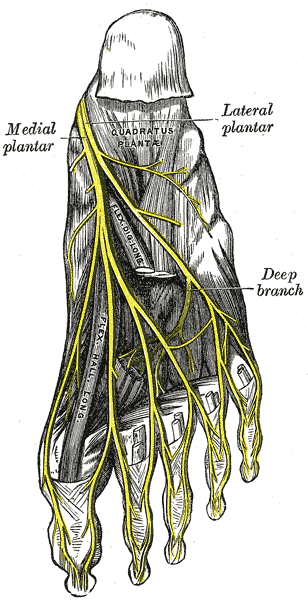
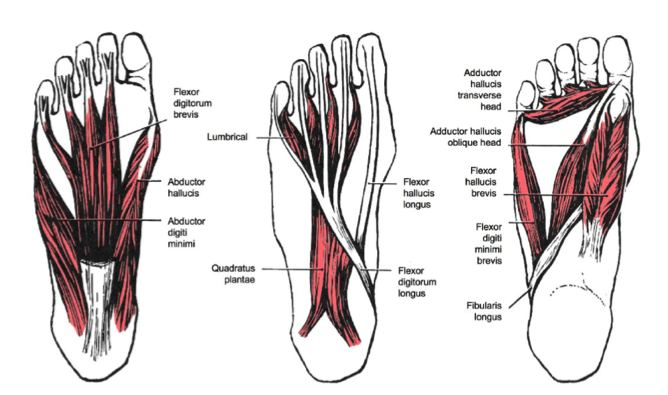
- Lateral plantar nerve (see image R), a branch of the Tibial nerve, entrapment represents 15–20% of the chronic plantar heel pain presentations[9].This can result from compression between the abductor hallucis and quadratus plantae muscles[10].
- The close proximity of this nerve to the calcaneal tuberosity suggests the possibility of entrapment, resulting in plantar heel pain[2].
3. Medial Calcaneal nerve (MCN) provides sensory innervation to most of the heel fat pad and to the superficial tissues overlying the inferior part of the calcaneus. MCN entrapment was only prevalent in 5 out of 200 surgical cases in one study[11].
4. Tarsal tunnel syndrome (TTS) can also contribute to plantar heel pain (the tunnel lies posterior to the medial malleolus of the ankle, beneath the flexor retinaculum)[12].
Presentation[edit | edit source]
- Pain[13]: usually burning, sharp, shooting, shock-like, electric, and occasionally as dull aching. Pain can be local or radiating proximally or distally. Symptoms tend to be worse during or after activities involving weight-bearing but this pain improves with rest. Progressively, the pain can occur with rest and in non weight-bearing positions. If the symptoms are caused by nerve entrapment, patients might experience night pain as a result of venostasis (slowing of venous outflow) and venous engorgement (local congestion an distension with blood)[2].
- Post-static dyskinesia: pain when a patient first stands after periods of rest. It is most commonly associated with nerve-related plantar heel pain. Patients report severe pain in the morning after rising from the bed. If the pain is due to neural compression it tends to ease with ambulation and movement, however, it tends to worsen if the pain is caused by plantar fasciitis[2].
- Paraesthesiae and neurological changes such as numbness, sensory changes, pins and needles around the medial and plantar aspects of the heel[2].
Assessment[edit | edit source]
Subjective Assessment[edit | edit source]
Pain Location. Physiotherapists are skilful at figuring out the source of the pain. ie the pain driver.
Pain Behaviour: It is important to understand the nature of the pain to get an idea of the main contributing factor.
- The pain can be neural or mechanical.
- Ask questions to investigate the pain pattern across the day and the aggravating and easing factors.
- Allowing patients to talk about their pain can be very insightful and can help us recognize catastrophizing behavior which is common in chronic pain patients.
- One of the useful motivational interviewing tips is to give your patients time to reflect on what they said. Try and summarize what they told you to understand the impact on the quality of their life[14].
Objective Assessment[edit | edit source]
Observe and Assess:
- Foot, lower leg and the entire kinetic chain.
- Posture-related problems such as leaning backward and shifting the weight to the ankles during gait or if the weight is mostly on the toes. The shape of the foot e.g. collapsed arch on one side. You can link the history of trauma from the subjective assessment to the findings on observation. Also, compare the foot shape with the other foot, a bilateral collapsed arches will be treated differently from somebody that comes in with steep thick high arched feet. The pes planusf(see image R)oot is not going to respond to the same treatment strategies as your very rigid pes cavus foot. The study of Im Yi et al[7] found excessive pronation to increase the stress on plantar fascia resulting in collapsied arch. The pronatory effect is believed to increase with age and is related to limited ankle dorsiflexion.
- Orthotics and footwear. The shape of footwear and the level of comfort they experience are important assessment measure. A study reported that people with chronic plantar heel pain have greater difficulties with footwear comfort, fit and choice[15]. Another study found a link between toe flexor weakness and foot-wear difficulties in people with plantar heel pain[16].
- Neural examination is also recommended. Some patients might describe some kind of bizarre pain which might be in different locations often disregarded because the main concern is the foot pain. Therefore, neural dynamics should be included in your assessment[6][2].
- Gait Assessment
- See also Biomechanical Assessment of Foot and Ankle
Things to observe during gait:
- Overstriding
- Short strides
- Pounding or heavy throbbing on one side
- Slapping with the foot
- Walking with inverted foot/feet
Clinical Tests:[edit | edit source]
Palpation: over the abductor hallucis and/or on the medial calcaneal tuberosity for reproduced symptoms.
The presence of maximal tenderness over the Lateral Plantar nerve indicates the diagnosis of its entrapment.
To diagnose the Medial Calcaneal nerve entrapment, look for the following findings:
- Maximal tenderness over the medial anterior part of the heel fat pad and abductor hallucis
- Distal radiating pain with pressure on the nerve
- Minimal tenderness over the plantar fascia origin
In case of Medial Plantar nerve entrapment, the tenderness is typically located over the plantar aspect of the medial arch around the navicular tuberosity
Dorsiflexion-eversion neurodynamic tests: With this test, all metatarsophalangeal joints are passively extended while the ankle is held in dorsiflexion and eversion. This test is aimed mainly to reproduce symptoms in Tarsal Tunnel Syndrome patients. By extending the Metatarsophalangeal joints we increase the strain on the Medial Plantar and Tibial nerves. Adding hip flexion with knee extension to the ankle dorsiflexion can further increase the strain on the tibial and plantar nerves at the ankle and foot without increasing the tension in the plantar fascia[17].
Tinel’s test: tapping along the course of a nerve. If the tapping produced tingling along the nerve distribution, the test is considered positive[2].
Differential Diagnosis[edit | edit source]
- Tibial Nerve
- Fat pad: fat pad atrophy and limited shock absorption capacity was found in patients older than 40 years. Wearing hard-soled shoes and walking on hard surfaces usually aggravate pain in people with soft and thin heel fat pad. On palpation, the tenderness tends to be localized on the fat pad and doesn't radiate to the medial calceneal tuberosity and plantar fascia[2].
- Kinetic chain problems
Case Study[edit | edit source]
In this section, we discuss a case presentation of a patient who had plantar heel pain and the successful management plan that she followed.
Our patient is a 50 year old professional woman who travels for work from city to another on a weekly basis. She wears high heels and regularly runs from a meeting to the next. Weekends were her exercising time when she travels home.
She is also a very good competitive cyclist who has recently decided to take up marathons as well. In order to achieve her training goals, she fitted in her busy schedule treadmill running during the week at the hotels she stays in and distance cycling on the weekends.
At one conference, she decided to wear flat shoes because there was a lot of walking involved. Two days later, the pain started in her feet. She reported burning pain in her heels that felt like electric shocks when she put her feet on the floor in the mornings.
She went to see a physiotherapist who did some shockwave therapy which she didn't find helpful. She was then referred to an orthopedic specialist who took some x-rays and found a heel spur that probably explains the pain. So she was put in a boot during waking and working hours for six to eight weeks and asked to stop exercising. At night, a splint was advised. In addition, rolling the foot on a PVC pipe was recommended to ease the pain.
Eight weeks later, she was still not able to walk. She was frustrated and felt unfit. So she presented for a second opinion to physio[6].
Remember: The spur is not the cause of the symptoms!
The spur is only an indication that there are some traction forces on the Plantar Fascia. Identifying these traction forces and the reason these forces generated a spur should be our way of thinking to help address the symptoms[6].
Also remember the Plantar Fascia is integral to the Achilles tendon complex. So by unloading and immobilizing the fascia, all these tendons are now unloaded. The Achilles and tibialis posterior tendons are responsible for unloading the foot when it's in contact with the floor/ground. Unloading these tendons can possibly make the tissue weaker and consequently increasing the stress on the Plantar Fascia. Immobilizing means taking the tendons' assistance away and applying more stress on the Plantar Fascia resulting in more pain to your patient[6].
Addressing the pain[edit | edit source]
In this patient's case, it was urgent to try and sort out her morning problem as this was the main complaint. Starting the day with pain contribute to the quality of the whole day.
Stretching the Plantar Fascia in a non-weight bearing position was recommended by Lim et al [13] and is a great way to warm up and ease the fascial pain at the start of the day.
Manage the load[13] The patient still has to be mobile and active at work and it was important to help her to return to running in the evenings on the treadmill. Although treadmills are great in the short term, they can be problematic because they do increase the tension and load on the Achilles tendon. So by running thirty minutes to an hour on the treadmill the load on the soft tissue structures is significant. Switching to stationary cycling while she's at work, in the week, and swapping with running on the weekends was advised.
Instead of running on the treadmill, the patient can do trail running, undulating, different terrains, with more cushion, and shorter runs twice a day. All these strategies were introduced to manage her load over the twenty-four hours. If there is a lot of tendon issues, a response to the training load can be seen over twenty-four hours. So in this case, the patient was asked to monitor her response to the load over twenty-four hours[6].
This patient also had rigid feet from wearing high heels for years. Manual mobilization for stiff feet can be beneficial [20][21]. Manual mobilization, myofascial releases were used to release the foot and make it more pliable and more shock absorbent. Other manual techniques to be used:
- Calf muscle release
- Mobilize the Calcaneus so that it sits neatly under the Talus.
- Release the Plantar Fascia[22]
- Improve the mobility of the first metatarsal phalangeal joint.
Improve the capacity of that Plantar Fascia. Stretching can be helpful but it won't be enough to improve the tolerance of the tissue for running. The principals of tendinopathy treatment can be used in the managing plantar fasciopathy pain. By combining the windlass mechanism with isometric exercises we can oad the plantar fascia effectively and build up the capacity gradually.
The patient was asked to do isometric sustained holds to reduce the pain for that first two weeks by extending her toes over a rolled-up towel to induce and load the foot in the windlass mechanism. Then instead of doing more repetitions, she did 5 isometric holds holding each of them for 45 seconds with her heels just slightly off the ground then lowering down very slowly followed by a one to two-minute rest. This exercise was started bilaterally then as she improved it was done unilaterally[26]. A 2014 study by Rathleff compared high load strength-training program to a standard plantar specific stretching program in the treatment of plantar fasciopathy reported positive outcomes in terms of pain and function quicker reduction in pain and improvements in function. [27] The study participants were performed unilateral heel-raises with a towel inserted under the toes to activate the windlass-mechanism (similar to the isometric holds done by our patient is this case study). The exercise was performed every second day for three months. This exercise slowly progressed to include weights (backpack or books) and decrease the number of repetitions. The results of this study showed improvement on the short term but on the long term, there was no difference between high load strengthening and plantar stretching programs.
[28] Another advice to this patient was to do Pilates and/or yoga work, to release and mobilize her overall neural system. Tibial Nerve mobilization can be done and taught to the patient but working on the overall flexibility and mobility is important to counteract the stationary posture obtained at work and through most of the day.
Foot-wear was also addressed. Clearly, high heels were contributing to the pain, putting a lot of load and stress on the metatarsal heads. To counterbalance, a nice pair of wedges (to avoid toes hyper-extension and putting the plantar fascia in a stretched position) and nice rocker-bottom heel or sole can be utilized. So the patient loaded-off her foot while she didn't compromise her work dress code[6]. Load can also be managed by wearing appropriate foot orthotics[13][29].
The patient agreed to keep a diary of her symptoms, modified the load as necessary, and increased the load gradually. Within two weeks, the pain was shifting and she was improving.
Plantar heel pain is not a simple problem, knowing from history that this patient was going through menopause, she was advised to check with her doctor if the hormonal changes are contributing to her symptoms.
There are other methods to desensitize the area and improve the motor control that can be used such as brushing the feet at night after a tough day and mirror therapy[6].
References[edit | edit source]
- ↑ Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. Is ‘plantar heel pain’a more appropriate term than ‘plantar fasciitis’? Time to move on.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: differential diagnosis and management. Manual therapy. 2008 Apr 1;13(2):103-11.
- ↑ Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC Musculoskelet Disord. 2019;20(1):337.
- ↑ 4.0 4.1 Sullivan J, Pappas E, Adams R, Crosbie J, Burns J. Determinants of footwear difficulties in people with plantar heel pain. Journal of Foot and Ankle Research. 2015 Dec;8(1):1-7.
- ↑ Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot & ankle international. 2004 May;25(5):303-10.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Simpson H. Plantar Heel Pain Course. Physioplus 2020
- ↑ 7.0 7.1 Im Yi T, Lee GE, Seo IS, Huh WS, Yoon TH, Kim BR. Clinical characteristics of the causes of plantar heel pain. Annals of rehabilitation medicine. 2011 Aug;35(4):507.
- ↑ Grim C, Kramer R, Engelhardt M, John SM, Hotfiel T, Hoppe MW. Effectiveness of Manual Therapy, Customised Foot Orthoses and Combined Therapy in the Management of Plantar Fasciitis—A RCT. Sports. 2019 Jun;7(6):128.
- ↑ Watson TS, Anderson RB, Davis WH, Kiebzak GM. Distal tarsal tunnel release with partial plantar fasciotomy for chronic heel pain: an outcome analysis. Foot & ankle international. 2002 Jun;23(6):530-7.
- ↑ May TJ, Judy TA, Conti M, Cowan JE. Current treatment of plantar fasciitis. Current sports medicine reports. 2002 Oct;1(5):278-84.
- ↑ Schon LC, Glennon TP, Baxter DE. Heel pain syndrome: electrodiagnostic support for nerve entrapment. Foot & ankle. 1993 Mar;14(3):129-35.
- ↑ Lau JT, Stavrou P. Posterior tibial nerve--primary. Foot and ankle clinics. 2004 Jun;9(2):271-85.
- ↑ 13.0 13.1 13.2 13.3 Lim AT, How CH, Tan B. Management of plantar fasciitis in the outpatient setting. Singapore medical journal. 2016 Apr;57(4):168.
- ↑ Roscher M. Motivational Interviewing course. Physioplus 2019
- ↑ Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. Journal of the American Podiatric Medical Association. 2008 Jul 1;98(4):283-9.
- ↑ Sullivan J, Pappas E, Adams R, Crosbie J, Burns J. Determinants of footwear difficulties in people with plantar heel pain. Journal of Foot and Ankle Research. 2015 Dec;8(1):1-7.
- ↑ Coppieters MW, Alshami AM, Babri AS, Souvlis T, Kippers V, Hodges PW. Strain and excursion of the sciatic, tibial, and plantar nerves during a modified straight leg raising test. Journal of Orthopaedic Research. 2006 Sep;24(9):1883-9.
- ↑ Dorsiflexion Eversion Test . Available from:https://www.youtube.com/watch?v=Z2LsxI8JWBE[last accessed 30/06/2020]
- ↑ Tinel's test (sign) for Tarsal Tunnel Syndrome . Available from:https://www.youtube.com/watch?v=xWi1tX7yrOA[last accessed 30/06/2020]
- ↑ Mischke JJ, Jayaseelan DJ, Sault JD, Emerson Kavchak AJ. The symptomatic and functional effects of manual physical therapy on plantar heel pain: a systematic review. Journal of Manual & Manipulative Therapy. 2017 Jan 1;25(1):3-10.
- ↑ Pollack Y, Shashua A, Kalichman L. Manual therapy for plantar heel pain. The Foot. 2018 Mar 1;34:11-6.
- ↑ Ajimsha MS, Binsu D, Chithra S. Effectiveness of myofascial release in the management of plantar heel pain: a randomized controlled trial. The Foot. 2014 Jun 1;24(2):66-71.
- ↑ Sports Massage - Plantar Fasciitis. Available from:https://www.youtube.com/watch?v=9SIGxc4IFGc[last accessed 30/06/2020]
- ↑ Subtalar Joint Mobilisation Techniques. Available from:https://www.youtube.com/watch?v=JzOZl2YbzeA[last accessed 30/06/2020]
- ↑ Big Toe 1st MTP joint Mobilisation. Available from:https://www.youtube.com/watch?v=YeS9NmhWfvw[last accessed 30/06/2020]
- ↑ Rathleff MS, Thorborg K. ‘Load me up, Scotty’: mechanotherapy for plantar fasciopathy (formerly known as plantar fasciitis).
- ↑ Rathleff MS, Mølgaard CM, Fredberg U, et al. High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up. Scand J Med Sci Spor 2014:n/a-n/a doi: 10.1111/sms.12313[published Online First: Epub Date]|.
- ↑ High Load Strength Training Plantar Fasciitis | Chris Johnson PT. Available from:https://www.youtube.com/watch?v=wUua8tI3m5s[last accessed 30/06/2020]
- ↑ Whittaker GA, Munteanu SE, Menz HB, Tan JM, Rabusin CL, Landorf KB. Foot orthoses for plantar heel pain: a systematic review and meta-analysis. British journal of sports medicine. 2018 Mar 1;52(5):322-8.