Physical Activity in Individuals with Disabilities
Original Editor- Clara Hildt
Top Contributors - Ewa Jaraczewska, Tarina van der Stockt, Kim Jackson, Rachael Lowe, Lucinda hampton, Jess Bell, Mariam Hashem, Simisola Ajeyalemi, Evan Thomas, George Prudden, Michelle Lee, WikiSysop, Rucha Gadgil, Aminat Abolade, Merinda Rodseth, 127.0.0.1, Admin and Giulia Neculaes
Introduction[edit | edit source]
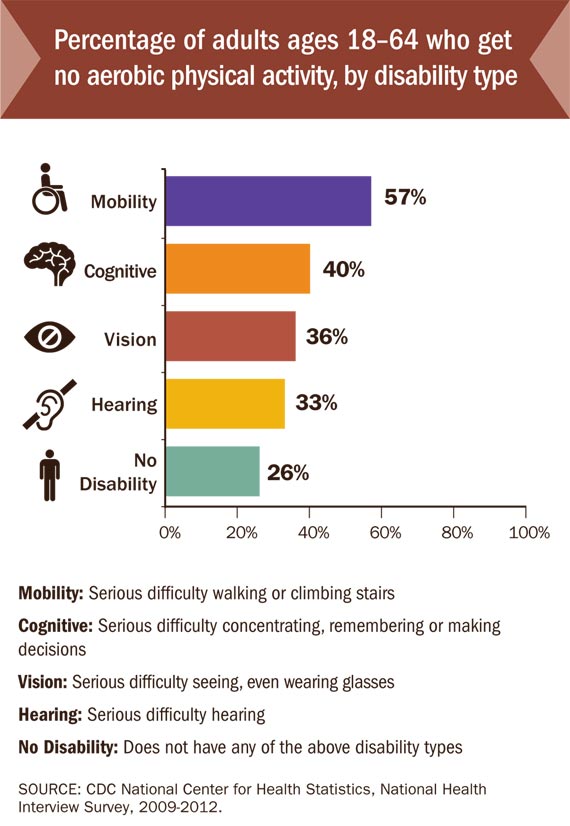
In the United States 20% of the population have a disability, which are 56 million US adults [1]. There are many types of disabilities, such as those that affect a person’s movement, vision, hearing, thinking, remembering, learning, communication, mental health or social relationships. [2] Individuals with disability are 57% more likely to be obese than adults without disabilities [3]. As obesity is an important risk factor adults with disability are three times more likely to have a chronic disease such as a heart disease, diabetes, stroke or cancer than adults without disabilities. [4] The impact of these chronic diseases can be reduced by aerobic physical activity but adults with disabilities only do physical activity on a regular basis about half as often as adults without disabilities (12% compared to 22%) [3]
Definition[edit | edit source]
Physical activity[edit | edit source]
Physical Activity (PA) is defined as any bodily movement produced by skeletal muscles that require energy expenditure. Activities undertaken while working, playing, traveling, carrying out housework and engaging in recreational pursuits are included thereby. The WHO recommends for adults to do at least 150 minutes of moderate-intensity PA throughout the week [5]. Compared to those who meet those criteria, people who are insufficiently physically active have a 20% to 30% increased risk of all-cause mortality. [6]
Individuals with Disability[edit | edit source]
When speaking about or working with individuals with a disability it is essential to put the person first. Disability does not define the person as it is only a medical diagnosis. Positive language empowers and therefore inclusive language is used in the article and should always be used. [7][8]
"A disability is any condition of the body or mind (impairment) that makes it more difficult for the person with the condition to do certain activities (activity limitation) and interact with the world around them (participation restrictions)."[9]
In the medical model of disability the condition is viewed as a medical and biological difficulty. Correcting ill-being is highlighted instead of preventing ill-being and promoting well-being. On the contrary, in the social model disability is viewed as a difference and not judged. This model would emphasise barriers such as structural factors or discriminatory behaviours that prevent PA. Both the medical and social model are criticised for highlighting extreme point of views [10]. Out of it the social relational model was developed which suggests that both impairments as well as social and environmental barriers can all operate simultaneously [11]
Benefits of physical activity for individuals with disability[edit | edit source]
PA is essential for quality of life reasons and as a public health promoter [10]
In people with disabilities PA has an amplified importance based on higher rates of chronic diseases which PA can influence. Above those metabolic advantages individuals with disability can further profit from PA:
- Health:
- PA also has amplified importance for cognitive, emotional and social difficulties
- Psychological benefits such as enhanced self-perception through successful PA experiences
- PA can reduce stress, pain, and depression → ADLs are perceived to be easier
- Social contact:
- PA can reduce the stigmatisation process and negative stereotypes
- PA can contribute to improve social status: non-disabled people see physically active individuals with disabilities more favourably than non-active people
- Social benefits as the nature of many sport activities leads to increased social integration, bonding and friendship
- Fun:
- PA leads to mood benefits
- Enjoyment through social interaction of both fitness staff and other participants
Barriers to Physical Activity[edit | edit source]
Despite the facilitators health benefits, social context and fun, there are depending on age and type of disability barriers on the individual, social and environmental level[12]:
Individual: lack of knowledge about where to exercise; fear of falling; the nature of the impairment can produce pain; lack of energy
Social: children with disabilities depend more on parents than healthy children do; Physical Education teachers lack professional preparation or equipment and have to exclude students with disabilities; doctors provide unnecessary blanket medical excuses which allow students with disabilities to skip Physical Education; lack of friends to play for children; physical abilities are underestimated by health professionals
Environmental: wheelchair; lack of place to play for children; health clubs are not accessible; barriers in outdoor areas (e.g. poorly lit or wooded walking paths, traffic lights lack audible signals) [10]
Health Care Provider[edit | edit source]
Guideline[edit | edit source]
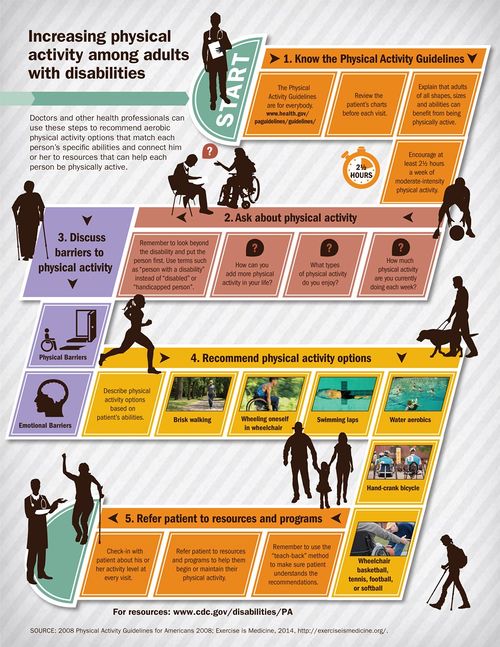
It is essential for physiotherapists and other health professionals to know the general Physical Activity Guidelines, as they are also applied for Individuals with disabilities. Adults with disabilities are more likely to be physically active if it is recommended by doctors. Thus if they got a PA recommendation they were 82% more likely to be physically active than those who did not get one. (CDC, 2014) [13] Physiotherapists and other health professionals can use these 5 steps as illustrated in the graphic below to increase physical activity among individuals with disabilities:
Interaction[edit | edit source]
General points you can consider when interacting with individuals with disabilities:
- If you are unsure about what to do when interacting with your patient, ask
- Speak directly to your patient instead of addressing a companion or interpreter when present
- Respect your patients’ assistive devices such as crutches or wheelchairs as their personal property that normally should not be moved unless having permission
- Consider extra time it may take your patient to transfer or prepare
- Never assume your patient needs your help. Offer your assistance and wait for reply and specific directions
- Avoid making general assumptions but instead try to get to know your patient’s individual needs, preferences and abilities.[8]
Find more specific advice here.
Promoting Physical Activity[edit | edit source]
Exercises[edit | edit source]
Find here factsheets describing various disabilities and health conditions, as well as physical activity, exercise, and overall health considerations and recommendations associated with each
Find here 5 easy general exercises for people with intellectual and developmental disabilities
Find [http://www.nchpad.org/1263/5964/Inclusive~Yoga NCHPAD Online program – “14 Weeks to a healthier You”: http://www.nchpad.org/14weeks/ here] different yoga poses
Inclusive Fitness Trainer[edit | edit source]
In the United States, an Inclusive Fitness Trainer (certified by the American College of Sports Medicine (ACSM) and the National Center on Health, Physical Activity and Disability (NCHPAD)), is a fitness professional who is uniquely qualified to work with people who have health risks and/or physical limitations. They have an understanding of the current Anti-Discrimination Act Policy and create adapted exercise programming that promotes safe and effective training. The aim is to empower individuals with disabilities to achieve their fitness goals.[14]
Campaign: How I Walk[edit | edit source]
“How I Walk is a movement to rebrand the word walking by challenging individual and societal perspectives.”[1] It is a call to action to promote walking and walkable communities. [1]
Special Olympics[edit | edit source]
Special Olympics is the world largest sports organisation for people with intellectual disabilities. There are programs in 169 countries with more than 4.7 million athletes and over a million volunteers. Through the joy of sport it aims to transform lives and to create a new world of inclusion. [15]
Visit this link for sports guides, rules and information
Sport Organisations[edit | edit source]
- International Wheelchair & Amputee Sports Federation
- International Paralympic Committee
- International Federation for Intellectual Disability Sport
- National Disability Sport Organisations in the UK.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 NCHPAD. How I Walk. About How I Walk. 2015 [cited 21/02/2017]. Available from: http://www.nchpad.org/howiwalk/
- ↑ CDC Centers for Disease Control and Prevention. Disability Overview. 2015 [cited 22/02/2017]. Available from: https://www.cdc.gov/ncbddd/disabilityandhealth/disability.html
- ↑ 3.0 3.1 US Department of Health and Human Services. I can do it you can do it. 2017 [cited 22/02/2017]. Available from: https://www.fitness.gov/participate-in-programs/i-can-do-it-you-can-do-it/
- ↑ CDC Centers for Disease Control and Prevention. Increasing Physical Activity among Adults with Disabilities. 2016 [cited 22/02/2017]. Available from: https://www.cdc.gov/ncbddd/disabilityandhealth/pa.html
- ↑ WHO. Physical Activity Fact sheet [Internet]. 2017 [cited 23/02/2017]. Available from: http://www.who.int/mediacentre/factsheets/fs385/en/
- ↑ WHOa. Prevalence of insufficient physical activity [Internet]. 2017 [cited 23/02/2017]. Available from: http://www.who.int/gho/ncd/risk_factors/physical_activity_text/en/
- ↑ Gov.uk. Inclusive language: words to use and avoid when writing about disability. 2014 [cited 23/02/2017]. https://www.gov.uk/government/publications/inclusive-communication/inclusive-language-words-to-use-and-avoid-when-writing-about-disability
- ↑ 8.0 8.1 NCHPAD. fckLRfckLRDisability Awareness: Interaction Tips for the Fitness Professional. General Rules. 2017 [cited 21/02/2017]. Available from: http://www.nchpad.org/615/2567/Disability~Awareness~~Interaction~Tips~for~the~Fitness~Professional
- ↑ CDC Centers for Disease Control and Prevention. Disability Overview. 2015 [cited 22/02/2017]. Available from: https://www.cdc.gov/ncbddd/disabilityandhealth/disability.html
- ↑ 10.0 10.1 10.2 Martin JJ. Benefits and barriers to physical activity for individuals with disabilities: a social-relational model of disability perspective. Disability and Rehabilitation 2013; Researchgate
- ↑ Thomas C. How is disability understood? An examination of sociological approaches. Disabil Soc 2004;19:569–83.
- ↑ Jaarsma EA, Dijkstra PU, Geertzen JHB, Dekker R. Barriers to and facilitators of sports participation for people with physical disabilities: A systematic review. 2014. Scandinavian Journal of Medicine & Science in Sports, 24 (6), 871-881
- ↑ CDC Centers for Disease Control and Prevention. Adults with Disabilities - Physical activity is for everybody. 2014 [cited 21/02/2017]. Available from: https://www.cdc.gov/vitalsigns/disabilities/
- ↑ ACSM. ACSM/NCHPAD Certified Inclusive Fitness Trainer. 2015 [cited 21/02/2017]. Available from: http://certification.acsm.org/acsm-inclusive-fitness-trainer
- ↑ Special Olympics. What We Do. 2017 [cited 22/02/2017]. Available from: http://www.specialolympics.org/Sections/What_We_Do/What_We_Do.aspx