Peripheral Edema
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Kim Jackson
Introduction[edit | edit source]
Peripheral edema (PE) is an accumulation of fluid in the interstitial space that occurs as the capillary filtration exceeds the limits of lymphatic drainage, producing noticeable clinical signs and symptoms[1].
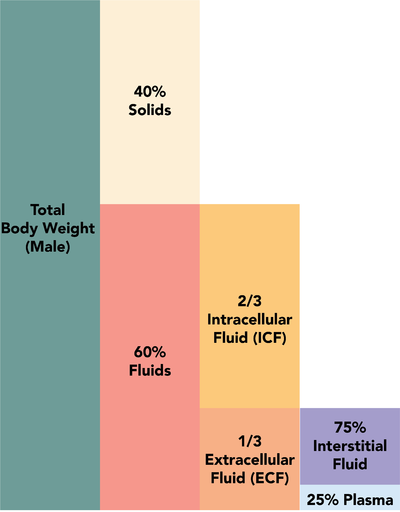
- Fluid compartments in the human body are divided between the intracellular and extracellular spaces.
- The extracellular space constitutes about one-third of total body water, which is further divided into intravascular plasma volume (25%) and the extravascular interstitial space (75%).
The fluid balance between these compartments is maintained by hydrostatic pressures and oncotic pressures. The Physiological mechanism causing peripheral edema occurs when this balance is altered by any one or more of the following factors
- Increased intravascular hydrostatic pressure
- Decreased intravascular or plasma oncotic (colloid osmotic) pressure
- Increased vascular permeability.
The lymphatic system collects fluid and filtered proteins from the interstitial space and returns that back to the vasculature. Any disturbance in this delicate homeostasis resulting in net filtration out of the vascular space or impaired return of fluid by lymphatics leads to the accumulation of fluid in the interstitial space ie PE.[2]
PE is a nonspecific symptom with a wide range of potential causes[3].
- Edema, other than localized edema, does not become clinically apparent until the interstitial volume has increased by 2.5 to 3 liters because the tissues constituting the interstitium can easily accommodate several liters of fluid. A patient's weight may increase by nearly 10% before pitting edema is evident[2].
Epidemiology[edit | edit source]
The causes of peripheral oedema are varied, requiring a systematic approach to history taking and examination. Diagnosis is often a process of elimination of the common causes[3].
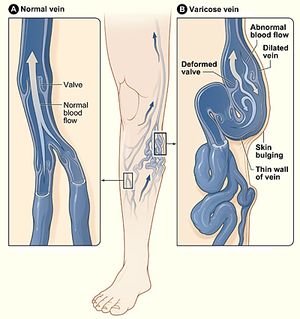
- The most common cause of peripheral edema in patients over 50 yrs of age is venous insufficiency and related to aging.
- The chronic accumulation of edema in one or both lower extremities often indicates venous insufficiency, especially in the presence of dependent edema and hemosiderin deposition[1]
- Many other underlying comorbid conditions eg heart failure, renal failure, liver failure, Lymphoedema, lipedema, cellulitis[3], obesity, obstructive sleep apnea, Complex regional pain syndrome[1] and trauma can affect any age group.
- Peripheral edema can also be commonly observed in pregnancy[2].
- Secondary causes of lymphedema include: tumor, trauma, previous pelvic surgery, inguinal lymphadenectomy, previous radiation therapy[1].
History and Examination[edit | edit source]
Peripheral edema may be a warning sign for many systemic diseases and if not treated early leads to high morbidity and mortality. The most important diseases to rule out are heart disease, liver disease, and kidney disease[2].
The history should include the
- Timing of the edema, whether it changes with position, and if it is unilateral or bilateral, as well as a medication history and an assessment for systemic diseases.
- Acute swelling of a limb over a period of less than 72 hours is more characteristic of deep venous thrombosis (DVT), cellulitis, ruptured popliteal cyst, acute compartment syndrome from trauma, or recent initiation of calcium channel blockers.
- The chronic accumulation of more generalized edema is due to the onset or exacerbation of chronic systemic conditions, such as congestive heart failure (CHF), renal disease, or hepatic disease
The physical examination should assess for systemic causes of edema eg heart failure (e.g., jugular venous distention, crackles), renal disease (e.g., proteinuria, oliguria), hepatic disease (e.g., jaundice, ascites, asterixis), or thyroid disease (e.g., exophthalmos, tremor, weight loss).
Edema should also be evaluated for pitting, tenderness, and skin changes[1].
- Pitting (See initial image) describes an indentation that remains in the edematous area after pressure is applied. This occurs when fluid in the interstitial space has a low concentration of protein, which is associated with decreased plasma oncotic pressure and disorders caused by increased capillary pressure (e.g., DVT, CHF, iliac vein compression). Lower extremity examination should focus on the medial malleolus, the bony portion of the tibia, and the dorsum of the foot.
Changes in skin temperature, color, and texture provide clues to the cause of edema. eg
- Acute DVT and cellulitis - increased warmth over the affected area.
- Chronic venous insufficiency - often associated with skin that has a brawny, reddish hue (deposition of hemosiderin) and commonly involves the medial malleolus.
- Lipodermatosclerosis (a progression of venous insufficiency) - associated with marked sclerotic and hyperpigmented tissue, and characterized by fibrosis and hemosiderin deposition that can lead to venous ulcers over the medial malleolus (may progress to deep, weeping erosion)s.
- Lymphedema (early stage) - skin has a doughy appearance, in the later stages, it becomes fibrotic, thickened, and verrucous (wart like growth)[1]
Management[edit | edit source]
Management of edema should be guided by the underlying etiology, which commonly includes chronic venous insufficiency, lymphedema, DVT, and medication-induced edema, among others[1]
- Diuretics are the treatment of choice in CHF, liver, and renal disease.
- In patients with DVT, anticoagulation therapy is used. In addition to anticoagulation, compression stockings should be used to prevent post-thrombotic syndrome.
- In patients with chronic venous insufficiency, mechanical therapies, including leg elevation and compression stockings, are effective. Compression therapy is contraindicated in peripheral arterial disease because it can compromise blood supply further.
- In lymphoedema, treatment involves complex decongestive physiotherapy that is composed of manual lymphatic massage and multilayer bandages. Maintenance therapy includes compression stockings and pneumatic compression devices.
- In patients where medications are the offending agent, they should be discontinued if possible and switch to a different class[2].
Physiotherapy Management[edit | edit source]
May be involved in (to name a few):
- Patient education - very crucial in peripheral edema as in other diseases. Generally speaking, patients should be educated regarding healthy lifestyle such as exercise, diet, and routine check-ups to diagnose underlying disease entities early and prevent long term complications.
- Complete Decongestive Therapy
- Mechanical therapies: including leg elevation and compression stockings with 20 to 30 mm Hg for mild edema and 30 to 40 mm Hg for severe edema complicated by ulceration, are recommended. Compression therapy is contraindicated in patients with peripheral arterial disease.
- Pneumatic devices: Mixed evidence exists for the use of pneumatic compression devices in patients with chronic venous insufficiency. However, these devices should be considered for patients in whom compression stockings are contraindicated.
- Skin care: eg Local skin and wound care of venous ulcers is essential in preventing secondary cellulitis and dermatitis. Eczematous (stasis) dermatitis, characterized by dry, inflamed, scaling skin overlying superficial varicose veins, often occurs in patients with chronic venous insufficiency. Treatment includes daily hydration with emollients and short courses of topical steroid creams for severely inflamed skin
- Complex regional pain syndrome: treated with physical therapy in combination with medications such as systemic steroids and tricyclic antidepressants.
- Obstructive sleep apnea: treated with positive pressure ventilation[1].
Elderly patients are at the highest risk for complications or underlying medical conditions. Physiotherapists should carefully monitor any symptoms and receive the assistance of a doctor if the condition worsens.
Conclusion[edit | edit source]
Peripheral edema can poses a diagnostic dilemma to family physicians due to a wide range of underlying diseases.
- The causes of edema may be due to a myriad of diagnoses, including heart, liver, renal, thyroid, and other vascular etiologies. Diagnosis should focus on ruling out any major organ system failure as the underlying etiology.
- If the systemic disease is suspected, then it is essential to consult with an interprofessional team of specialists, depending upon underlying disease suspicion.
- The nurses are also a vital member of the interprofessional group as they will monitor the patient's daily progress, especially when the patient is on diuretics by monitoring daily weights, fluid input, and output.
- The outcomes of edema depend on the cause. Therefore, to improve outcomes, prompt consultation with an interprofessional group of specialists is very important to prevent complications.[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Trayes KP, Studdiford JS, Pickle S, Tully AS. Edema: diagnosis and management. American family physician. 2013 Jul 15;88(2):102-10.Available from:https://www.aafp.org/afp/2013/0715/p102.html (last accessed 18.10.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Goyal A, Cusick AS, Bansal P. Peripheral Edema. InStatPearls [Internet] 2020 Feb 17. StatPearls Publishing.Available from: https://www.ncbi.nlm.nih.gov/books/NBK554452/(last accessed 18.10.2020)
- ↑ 3.0 3.1 3.2 KUMARASINGHE G. peripheral oedema 2012.Available from: https://medicinetoday.com.au/sites/default/files/cpd/MT2015-06-026-KUMARASINGHE.pdf(last accessed 18.10.2020)