Pelvic Floor Exercises
Original Editor - Audrey Brown
Top Contributors - Audrey Brown, Ruchi Desai, Vidya Acharya, Kim Jackson, Lucinda hampton and Khloud Shreif
Introduction[edit | edit source]
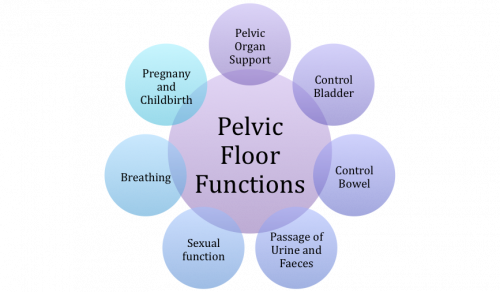
The pelvic floor, also known as the pelvic diaphragm, are a collection of muscles that span the floor of the pelvis. The pelvic floor muscles enclose the pelvic viscera, including the bladder, intestines, and uterus (in females) and separate the pelvic cavity above from the perineal region (located between the anus and the overt genitals) below.. [1]The pelvic floor supports abdominal and pelvic viscera, maintains bowel and bladder continence, and functions in voiding, defecating, sexual activity, and childbirth.[2]
Weak, strained, or overly tight pelvic floor muscles can lead to pelvic floor dysfunction, which may include pelvic pain, urinary/bowel incontinence, pain with sex, sexual dysfunction, and pelvic organ prolapse. [3]
The contraction of pelvic floor muscles during perineal exercises results in elevation of the urethra, vagina, and rectum, resulting in stabilization of the pelvic floor and resistance to downward movement.[4] Pelvic floor exercises can strengthen and increase neuromuscular control over the pelvic floor muscle and may reduce or eliminate symptoms associated with pelvic floor dysfunction.[3]
Indications for Pelvic Floor Exercise[edit | edit source]
The below symptoms may indicate the need for Pelvic Floor Exercises in all genders:
- Urinary incontinence/frequency/urgency [5][6]
- Pain in pelvic region, genitals, perineum, or rectum [6]
- Sexual dysfunction including erectile dysfunction, pain or numbness in the genitals during or after sex [7][8]See also Sexual Dysfunction After Prostate Cancer
- Pelvic organ prolapse, which may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in the vagina or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping. [9]
- Chronic low back pain unexplained by other sources[10]
Activating the Pelvic Floor Muscles[edit | edit source]
Pelvic floor exercises begin with learning to simply activate the pelvic floor muscles.
- The first step is to find a comfortable position, attempt to relax all muscles, and focus on a steady breathing pattern.
- To activate the anterior pelvic floor muscles, replicate the action of stopping the flow of urine mid-stream. [11]
- To activate the posterior pelvic floor muscles, replicate the action of stopping passing gas. [11]
- To activate both the anterior and posterior pelvic floor muscles, combine the two above actions. [11]
When activating the anterior pelvic floor muscles, it is important to not actually stop the flow of urine mid-stream when using the bathroom, as this may lead to difficulty with fully emptying the bladder.
Pelvic Floor Awareness, Training, and Strengthening[edit | edit source]
Begin pelvic floor exercise training with an empty bladder. Gravity-assisted positioning (hips higher than the heart, such as supported bridge or elbows/knees position) may be indicated initially for some women with extreme weakness and proprioceptive deficits. Positional changes are introduced as strength and awareness improve (supine, side-lying, quadruped, sitting, standing)
- Contract–Relax: tighten the pelvic floor as if attempting to stop urine flow or hold back gas. Hold for 3 to 5 seconds and relax for at least the same length of time. Repeat up to 10 times (if performed with proper technique)[12]
- Quick Contractions: perform quick, repeated contractions of the pelvic floor muscles while maintaining a normal breathing rate and keeping accessory muscles relaxed. Try for 15 to 20 repetitions per set[12].
- “Elevator” Exercise: imagine riding in an elevator. As it goes up from one floor to the next contracts the pelvic floor muscles a little more. As strength and awareness improve, add more “floors” to the sequence of the contraction. Another way to increase difficulty is to relax the muscles gradually, as if the elevator were descending one floor at a time. This component requires an eccentric contraction and is very challenging[12].
Specific Exercises[edit | edit source]
Kegel[edit | edit source]
The Kegel exercise is probably the most widely known pelvic floor exercise. It consists of an isometric contraction of the pelvic floor muscles.
To do a Kegel exercise, follow these steps:
- Start by holding your pelvic floor muscles in for 5 seconds. It is important to keeping breathing during this contraction.
- After holding for 5 seconds, slowly and completely relax your muscles for 5 seconds.
- Repeat this process 10 times, at least 3 times every day.
The pelvic floor muscles may get fatigued during this exercise. If this happens, stop and do the exercise at a later time. Don’t recruit the abdominal, adductors or buttock muscles when doing this exercise.
Exercises can be progressed by increasing the time you hold and rest your pelvic floor muscles. Start with 5 seconds, and slowly build up the time each week until you’re holding in and resting for 10 seconds.[13]
Reverse Kegel[edit | edit source]
Fatigued pelvic floor muscles and imbalanced intra-abdominal pressures can lead to hypertonic pelvic floor muscles. [14]
The Reverse Kegel is a technique to mindfully relax pelvic floor muscles. The patient focuses their mental attention to the pelvic floor muscles and then voluntarily tries to relax them. The feeling of dropping the pelvic floor is similar to the moment of relief when you have reached the bathroom; when you urinate or have a bowel movement, you first drop your pelvic floor, and let the pelvic floor muscles (PFM) go. [15]
To perform a Reverse Kegel, follow these steps:
- Start by gently contracting the pelvic floor to feel what tightening the muscles feels like.
- Relax, and release the tension to feel the difference between tension and relaxation.
- Then, try to visualize that the muscles between the pubic bone and tailbone lengthen by gently moving the pubic bone towards the ceiling (if you are lying on your back), and gently move your tailbone towards the surface you are lying on. Imagine that the pelvic floor muscles are getting longer as this happens creating more space in your pelvic floor.
- During the above action, be sure to breath normally.
As you perform a Reverse Kegel, be sure you keep your pelvis and spine still. These can be performed in sitting and standing as well. [15]
Transverse Abdominis Activation[edit | edit source]
Activation of the transversus abdominis (TrA) has been shown to facilitate pelvic floor muscle activation and vice versa. [17]TrA activation also leads to increased pelvic floor muscle activity without directly training the pelvic floor musculature.
Transverse abdominis activation can be progressed based on body position, increasing hold times, and increasing sets. Activation can first begin in low-load body positions, including supine, quadruped, sitting, or standing.[17]TrA activation can be challenged by adding arm and/or leg movements and movements like walking or balancing on a tilt board. The plank is a great exercise for TrA
Biofeedback[edit | edit source]
Biofeedback is an instrument-assisted intervention that allows patients to observe real-time pelvic floor muscle activity.[19]Biofeedback can be used to strengthen weak pelvic floor muscles and to relax hypertonic pelvic floor muscles.
Similar to the Kegel exercise, biofeedback exercises consist of alternating periods of contraction and relaxation. Biofeedback interventions may improve sensitivity and neuromuscular control of the pelvic floor muscles.[20]When using biofeedback with a patient, be sure you measure baseline pelvic floor muscle activity before beginning exercise. [20]
Hypopressive Exercises[edit | edit source]
In 1980, Caufriez developed the abdominal hypopressive technique to help postnatal women recover from pelvic floor dysfunction and prevent complications, such as UI and prolapse. The technique involves breathing, based on diaphragm expiration, apnoea and elevation of the diaphragm, coupled with postural and active muscle stretching exercises [21]
Hypopressive exercises (HE) have been used in the treatment of PFM dysfunctions, such as urinary incontinence. Hypopressive exercises are postural exercises which relax the diaphragm, reduce intra-abdominal pressure, and activate abdominal and pelvic floor muscles (PFM) without voluntary activation.[22][23] They can be performed in different positions such as supine, sitting or standing, kneeling, quadruped and with varying position of arms and legs. This performance in combination with apnea (breath hold at end expiration), while drawing-in their abdomen and opening their rib cage.[24] The resulting pressure changes has been described to activate the postural muscles, such as the deep abdominal muscles and pelvic floor muscles.
In all of the hypopressive postures, patients perform the “hypopressive maneuver,” as follows. Patients are asked to: Take a deep brathe; Exhale breath completely (that action elevates diaphragm); Close their glottis; Then asked to expand their rib cage such that, theoretically, intra‐ abdominal pressure drops.[23]
A 8-week of hpyopressive exercises showed a decrease in pelvic floor disorders associated symptoms, improved pelvic floor muscle contractility.[25] Another study shows that PFMs, abdominal, gluteal, and adductor muscles are activated during the HE maneuver.[24] A cross-sectional study done in 99 healthy university students to assess the thickness of the abdominal muscles at rest and during HE using ultrasound imaging in supine and standing positions showed that HE significantly increased the thickness of the deep abdominal muscles, such as transversus abdominis and internal oblique, both in supine and standing positions. Thus, suggesting HE has more impact on the deeper muscles, however, physical therapists and other professionals working with HE should note that the more superficial muscles of the abdominal wall, the external oblique and rectus abdominis that did not seem to change in both positions during HE would need to be addressed with appropriate exercises.[23]
Pelvic Clock Exercise[edit | edit source]
Pelvic clock exercises help in developing proprioceptive awareness and pelvic movement control[12]. The video below demonstrates pelvic clock workouts in supine, and the exercises may be advanced to be performed in side-lying, quadruped, sitting, or standing positions.
Occupational Therapy[edit | edit source]
Occupational therapists works collaboratively with other healthcare professionals to provide a comprehensive approach for managing functional impairments resulting from pelvic floor disorders (PFDs). Their intervention aims to decrease social, physical, psychological, and sexual stressors, ultimately enhancing self-esteem and quality of life (QoL)[27].
Occupational therapy include a comprehensive assessments to understand the impact of pelvic floor dysfunction on an individual's daily activities, functional abilities, and quality of life, educate individuals about pelvic floor anatomy, proper body mechanics, and strategies for managing symptoms, in addition, collaborate with individuals to identify and modify daily activities that may exacerbate pelvic floor dysfunction and may include guidance on proper body mechanics, posture, lifting techniques, and ergonomic adjustments. Occupational therapists help patient with pelvic floor disorders to develop pain management strategies, including relaxation techniques, mindfulness, and stress reduction and adaptive strategies, modifications, or using assistive devices to enhance independence and participation.
Resources[edit | edit source]
References[edit | edit source]
- ↑ Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterology & Motility. 2006 Jul;18(7):507-19.
- ↑ Mantle J, Haslam J, Barton S, Polden M. Physiotherapy in obstetrics and gynaecology. Butterworth-Heinemann,; 2004.
- ↑ 3.0 3.1 https://www.nhs.uk/common-health-questions/womens-health/what-are-pelvic-floor-exercises/
- ↑ Schreiner L, Crivelatti I, de Oliveira JM, Nygaard CC, Dos Santos TG. Systematic review of pelvic floor interventions during pregnancy. Int J Gynaecol Obstet. 2018 Oct;143(1):10-18. doi: 10.1002/ijgo.12513. Epub 2018 May 18.
- ↑ Pelvic Obstectric and Gynaecological Physiotherapy. 2016. Pelvic floor muscle exercises (for men)[online] [viewed 26 March 2018]. Available from: https://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ 6.0 6.1 NHS Choices. 2017. Living with incontinence [online] [viewed 28 March 2018]. Available from: https://www.nhs.uk/conditions/urinary-incontinence/
- ↑ Women's and Men's Health Physiotherapy. 2017. Leading the way in pelvic health [online] [viewed 28 March 2018]. Available from: https://www.wmhp.com.au
- ↑ Male Pelvic Floor. 2012. Sexual Dysfunction and the Male Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://malepelvicfloor.com/sd.html
- ↑ Pelvic Floor First. 2017. Pelvic Floor First [online] [viewed 26 March 2018]. Available from: https://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html
- ↑ Bi X, Zhao J, Zhao L, Liu Z, Zhang J, Sun D, Song L, Xia Y. Pelvic floor muscle exercise for chronic low back pain. J Int Med Res. 2013 Feb;41(1):146-52. doi: 10.1177/0300060513475383. Epub 2013 Jan 23.
- ↑ 11.0 11.1 11.2 Polden, M. and Mantle, J., 1990. Physiotherapy in obstetrics and gynaecology. Elsevier Health Sciences.
- ↑ 12.0 12.1 12.2 12.3 Kisner C, Colby L, Borstad J. eds. Principles of Exercise for the Obstetric Patient Therapeutic Exercise: Foundations and Techniques, 7e. McGraw Hill; 2018. Accessed August 01, 2023.
- ↑ https://www.mskcc.org/cancer-care/patient-education/pelvic-floor-muscle-kegel-exercises-men
- ↑ Louis-Charles K, Biggie K, Wolfinbarger A, Wilcox B, Kienstra CM. Pelvic Floor Dysfunction in the Female Athlete. Curr Sports Med Rep. 2019 Feb;18(2):49-52. doi: 10.1249/JSR.0000000000000563.
- ↑ 15.0 15.1 https://pelvichealthsolutions.ca/for-the-patient/what-is-pelvic-floor-muscle-tightness/reverse-kegels/
- ↑ Kegels Exercises for Women - Complete BEGINNERS Guide.Available from:https://www.youtube.com/watch?Wjb20SXIvA4
- ↑ 17.0 17.1 Ghaderi F, Mohammadi K, Amir Sasan R, Niko Kheslat S, Oskouei AE. Effects of Stabilization Exercises Focusing on Pelvic Floor Muscles on Low Back Pain and Urinary Incontinence in Women. Urology. 2016 Jul;93:50-4. doi: 10.1016/j.urology.2016.03.034. Epub 2016 Apr 5.
- ↑ Physical Therapy Nation. Clinician Education: How To Teach Proper Transverse Abdominis Contraction. Available from: https://www.youtube.com/watch?How To Teach Proper Transverse Abdominis Contraction
- ↑ Capelini MV, Riccetto CL, Dambros M, Tamanini JT, Herrmann V, Muller V. Pelvic floor exercises with biofeedback for stress urinary incontinence. Int Braz J Urol. 2006 Jul-Aug;32(4):462-8; discussion 469. doi: 10.1590/s1677-55382006000400015.
- ↑ 20.0 20.1 Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019 Dec;31(6):485-493. doi: 10.1097/GCO.0000000000000584.
- ↑ Soriano L, González-Millán C, Sáez MÁ, Curbelo R, Carmona L. Effect of an abdominal hypopressive technique programme on pelvic floor muscle tone and urinary incontinence in women: A randomised crossover trial. Physiotherapy. 2020 Sep 1;108:37-44.
- ↑ Navarro-Brazález B, Prieto-Gómez V, Prieto-Merino D, Sánchez-Sánchez B, McLean L, Torres-Lacomba M. Effectiveness of Hypopressive Exercises in Women with Pelvic Floor Dysfunction: A Randomised Controlled Trial. J Clin Med. 2020 Apr 17;9(4):1149.
- ↑ 23.0 23.1 23.2 Da Cuna-Carrera I, Alonso-Calvete A, Soto-González M, Lantarón-Caeiro EM. How do the abdominal muscles change during hypopressive exercise?. Medicina. 2021 Jul 9;57(7):702.
- ↑ 24.0 24.1 Navarro-Brazález B., Sánchez-Sánchez B., Prieto-Gómez V., De la Villa-Polo P., McLean L., Torres-Lacomba M. Pelvic floor and abdominal muscle responses during hypopressive exercises in women with pelvic floor dysfunction. Neurourol. Urodyn. 2020;39:793–803.
- ↑ Molina‐Torres G, Moreno‐Muñoz M, Rebullido TR, Castellote‐Caballero Y, Bergamin M, Gobbo S, Hita‐Contreras F, Cruz‐Diaz D. The effects of an 8‐week hypopressive exercise training program on urinary incontinence and pelvic floor muscle activation: A randomized controlled trial. Neurourology and Urodynamics. 2023 Feb;42(2):500-9.
- ↑ How To Do The Pelvic Clock Exercise.Available from:https://www.youtube.com/watch?How To Do The Pelvic Clock Exercise
- ↑ Rivalta M, Sighinolfi MC, Micali S, De Stefani S, Bianchi G. Sexual function and quality of life in women with urinary incontinence treated by a complete pelvic floor rehabilitation program (biofeedback, functional electrical stimulation, pelvic floor muscles exercises, and vaginal cones). The journal of sexual medicine. 2010 Mar;7(3):1200-8.