Pelvic Floor Distress Inventory (PFDI - 20)
Original Editor - Kirsten Ryan
Top Contributors - Kirsten Ryan, Admin, Laura Ritchie, Michelle Walsh, Kim Jackson, Tony Lowe, WikiSysop, Evan Thomas, Oyemi Sillo and Nicole Hills
Objective[edit | edit source]
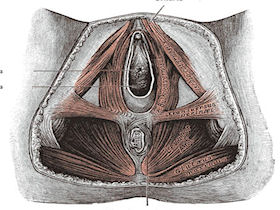
The Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20) is the short-form version of the Pelvic Floor Distress Inventory (PFDI).[1] Similar to the PFIQ-7, it is a health-related quality of life questionnaire for women with pelvic floor conditions to fill out.[1] The PFDI-20 is comprised of 3 scales, which include the Urinary Distress Inventory-6 (UDI-6), Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), and the Colorectal-Anal Distress Inventory-8 (CRADI-8).[1]
Intended Population[edit | edit source]
Women over the age of 18 with disorders of the pelvic floor including urinary incontinence, pelvic organ prolapse, and fecal incontinence.[1]
Method of Use[edit | edit source]
Since it is comprised of the UDI-6, POPDI-6, and the CRADI-8, the PFDI-20 includes 20 questions.[1] Each question begins with a "yes" or "no" response. If "yes," the patient must indicate how much bowl, bladder, or pelvic symptoms have been bothering them in the past 3 months on a 4-point scale that ranges from "not at all" (0) to "quite a bit" (4).[1] The scale scores are found individually by calculating the mean value of their corresponding questions and then multiplying by 25 to obtain a value that ranges from 0 to 100.[1] The sum of the 3 scales are added together to get the PFDI-20 summary score, which ranges from 0 to 300.[1]
Evidence[edit | edit source]
Correlation[edit | edit source]
Correlation, represented by r, ranges from -1.0 to +1.0. If the r value is 0 that means there is no correlation. If the r value is close to -1.0 that means that both values will decrease linearly. If the r value is close to +1.0 that means that both values will increase linearly.
Correlation of the short-form versions with the long-form versions:[1]
Reliability[edit | edit source]
The test-retest reliability, represented by intraclass correlation coefficients (ICC):[1]
Validity[edit | edit source]
The PFDI-20 demonstrates construct validity as it demonstrates a significant association with appropriate measures of symptom severity and pelvic floor diagnoses.[1]
Responsiveness[edit | edit source]
Each of the 3 scales of the PFDI-20 demonstrated moderate to excellent responsiveness with effect size and standardized response mean values ranging from 0.70 to 1.28.[1] The sensitivity of the PFDI-20 as a whole was excellent with an effect size of 1.48 P < .0001 and standardized response mean of 1.09 P < .0001.[1] The ability of the PFDI-20 to discriminate between subjects who indicated that they were "worse" after surgery from those who indicated they were "better" was excellent with c-statistic of .95.[1]
Clinically Meaningful Change[edit | edit source]
At the time of creation, the clinically meaningful change in quality of life (MCID)[2] needed to be studied in larger populations.[1] Studies have found minimal importance changes (MIC) ranging from 23 to 45.[1][3][4] For example, in their small sample size, Barber and colleagues (2004)[1] found a change in the summary score of 45 points or more to be meaningful after surgery.[1] However, it is important to consider that patients undergoing surgery also generally have higher scores at baseline.[5]
More recently, Wiegersma and colleagues (2017)[5] aimed to determine the MIC in women undergoing conservative pelvic organ prolapse treatments for mild symptoms.[5] They found that an improvement of 13.5 points to be helpful when evaluating the effects of conservative treatment strategies.[5]
Miscellaneous[edit | edit source]
The strength of the PFDI-20 is that it is a short form that gives a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as urinary incontinence. A more generic quality-of-life form as the SF-36 has demonstrated poor responsiveness in patients undergoing treatment for urinary incontinence. In these patient populations, it may be important to use both a generic quality-of-life instrument and a condition-specific instrument that has demonstrated responsiveness. The PFDI-20 is easy to use in both clinical and research settings.[1]
Links[edit | edit source]
- Overview of PFDI-20 on the Rehabilitation Measures Database.
- Paper by Barber et al 2005 describing the development of the PFIQ-7
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area. |
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 adn PFIQ-7). Am J Obstet Gynecol 2005;193:103-113.
- ↑ Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. Journal of clinical epidemiology. 2003 May 1;56(5):395-407.
- ↑ Gelhorn HL, Coyne KS, Sikirica V, Gauld J, Murphy M. Psychometric evaluation of health-related quality-of-life measures after pelvic organ prolapse surgery. Female pelvic medicine & reconstructive surgery. 2012 Jul 1;18(4):221-6.
- ↑ Utomo E, Blok BF, Steensma AB, Korfage IJ. Validation of the pelvic floor distress inventory (PFDI-20) and pelvic floor impact questionnaire (PFIQ-7) in a Dutch population. International urogynecology journal. 2014 Apr 1;25(4):531-44.
- ↑ 5.0 5.1 5.2 5.3 Wiegersma M, Panman CM, Berger MY, De Vet HC, Kollen BJ, Dekker JH. Minimal important change in the pelvic floor distress inventory-20 among women opting for conservative prolapse treatment. American journal of obstetrics and gynecology. 2017 Apr 1;216(4):397-e1.