Peabody Developmental Motor Scale (PDMS-2)
Original Editor - Wanda van Niekerk
Top Contributors - Wanda van Niekerk, Jess Bell, Kim Jackson, Mariam Hashem and Robin Tacchetti
Introduction[edit | edit source]
The Peabody Developmental Motor Scale was first developed and published in 1983 by Rhonda Folio and Rebecca Fewell.[1] A second edition was published in 2000 by the same authors (PDMS-2).[2]
No specific course or accreditation is needed to be able to conduct the test, but it is valuable to have good knowledge on the developmental stages of a child. A wide variety of healthcare professionals, such as physiotherapists, occupational therapists, psychologists, doctors and physical education teachers, can perform the test in the assessment of a child with possible developmental delay or issues. A good knowledge base in normal and typical development as well as in atypical development is recommended. This will make it easier to understand the nuances in the development of children.[3] The assessment kit is available for purchase online.
Benefits of the PDMS-2[edit | edit source]
- Excellent tool for the evaluation of the motor development of young children by providing separate tests and grading scales for both gross motor skills and fine motor skills[4]
- Test battery standardisation carried out with a total of 2003 children in the USA and Canada and is the first battery that was standardised on a national level[2][4]
- Only tool of its kind that combines evaluation with planned intervention. A planned program of 104 motor teaching and therapy activities is included.[2][4]
- These activities are organised based on the child’s development. The program can help in:
- the development of skills, provided that the evaluation of a child’s skills based on the test battery has been completed.[4]
Application of the PDMS-2[edit | edit source]
The test was designed to identify developmental delays in children. The test can be used in various populations and settings to achieve specific goals. These may include[2][3]:
- Assessing a child's motor competence relative to his/her peers
- For example in a clinical setting where children with various diagnosis and a wide range of neuromuscular impairments can be assessed and therapy provided
- Identifying delays or disorders in development
- For example in a school setting – i.e. At a preschool, to pick up on children that may have developmental delay as well as their strengths and weaknesses
- Useful tool to evaluate a child's progress
- Test was developed to identify strengths and weaknesses in a child’s motor development. Administering the test before and after a physical therapy intervention plan is a good way to document the child’s progress and to measure the efficacy of the intervention.
- Research purposes
- PMDS-2 is the gold standard and is often used in research and literature to assess the nature of motor development in various populations of children
- Specific skill deficits can be used to develop individualised goals.
- Helps in designing treatment goals and treatment plan based on the child’s strengths and weaknesses in motor development
Administrator Qualification[edit | edit source]
No specific course or accreditation is needed to be able to conduct the test, but it is valuable to have good knowledge on the developmental stages of a child. A wide variety of healthcare professionals can perform the test in the assessment of a child with possible developmental delay or issues. These may include:
- physiotherapists
- occupational therapists
- psychologists
- doctors
- physical education teachers
A good knowledge base in normal and typical development as well as in atypical development is recommended. This will make it easier to understand the nuances in the development of children.[3] It is also recommended to have a thorough understanding of[5]:
- test statistics
- general procedure governing test administration
- scoring and interpretation of score
- specific information about gross and fine motor skills testing
- development in children who are not progressing typical to their peers
Validity and Reliability of PDMS-2[edit | edit source]
The PDMS-2 has been proven as a reliable and valid measurement tool in various paediatric populations, such as:
- Children on the autistic spectrum[6]
- Children with cerebral palsy[7]
- Premature children and babies[8][9]
- Children receiving physical therapy for various diagnoses[10][11]
Target Population[edit | edit source]
The Peabody Developmental Motor Scale -2 is appropriate and should be used for children from birth to 5 years (72 months) old.[2]
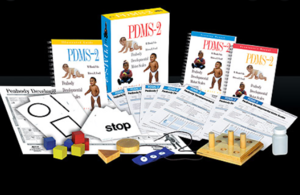
PDMS-2 Toolkit[edit | edit source]
The Peabody Developmental Motor Scale -2 Toolkit is available for online purchase and consists of the following materials that are required to administer the test:
- Examiners manual
- includes the history of test development
- describes the validity and reliability measures of the test
- contains the various scoring charts
- The Guide to Item Administration
- includes a description and images of each of the activities or skills assessed
- Motor Activities Program Book
- includes various ways/options in which to teach a child the skills that he/she is having difficulty with
- the importance of various skills is also discussed and highlighted
- Profile/Summary form
- document where all raw data can be added to create a scoring graph
- Examiners Record Booklet
- used by therapist when administering the test to score all activities or skills assessed
- Test Manipulatives document
- indicates what items are needed to administer the test, for example a 8-inch ball, tennis ball, string, chair, tape measure, etc.
- Peabody Motor Development Chart
Administration of PDMS-2[edit | edit source]
Authors' Advice[edit | edit source]
- Read the manual beforehand
- Have someone assist who is familiar with the test
- Run the test three times before actually concluding a score
- Calm and nice environment
- Be sensitive to the child’s limitations – avoid the child becoming frustrated[2]
Important Tips[edit | edit source]
- All assessment items should be presented in a precise manner with specific verbal cues and demonstrations
- Administer test in an environment with minimal distractions
- The area where test is administered should be set-up beforehand, areas marked out and pre-measured and equipment ready. This is to avoid any disruptions during the test and allow the test to flow. Examples of areas to pre-measure include[3]:
- Line on the floor clearly marked (spray paint or duct tape) – 4 inches wide and 8 feet long
- Area where child needs to run also marked out – 10 feet (3m) 30 feet (9m), 45 feet (13m) or converted to the metric system
- Jumping distances demarcated
- Jumping from different heights – have benches already ready and at correct heights
Description of the PDMS-2[edit | edit source]
The Peabody Developmental Motor Scale (PDMS-2) assesses fine and gross motor skills of children from birth to six years old relative to their peers. There are four subtests about gross motor skills and two subtests about fine motor skills. The gross motor subtests include[12]:
- Reflexes (birth to 11 months)
- Stationary performances (all ages)
- Locomotion (all ages)
- Object manipulation (12 months and older)
The fine motor skills subtests include:
- Grasping (all ages)
- Visual-motor integration (all ages)
The total score is determined by the sum of the points of each subscale/item. Every item is rated on a 3-point rating scale. Internal consistency of the scale is very high (alpha = 0.97).[13]
Administering the Gross Motor Function Part of the PDMS-2[edit | edit source]
Often in multidisciplinary team set-ups, the physiotherapist will assess the gross motor function part and an occupational therapist will focus on the fine motor section. As already mentioned the complete PDMS-2 has six subtests. The first four focuses on gross motor skills and the last two on fine motor skills. For the purpose of this page, focus will be on the gross motor skill subtests.
Reflexes[edit | edit source]
- This investigates the child’s reaction to outside stimuli or the child's ability to automatically react to environmental events.
- This test is only administered to children under the age of 1 year, as reflexes are typically integrated by the time a child is 12 months old.
- Eight different items are assessed under reflexes. Some of these are:
- Walking reflex
- Positioning Reflex: Asymmetrical Tonic Neck Reflex (integrated)
- Landau Reaction
- Protecting Reaction - Forward
- Protection Reaction - Side
- Right Reaction - Forward
- Protecting Reaction - Backward
Stationary[edit | edit source]
- This subtest assesses a child's ability to sustain control of his/her body within its centre of gravity and the ability to retain equilibrium
- Thirty different items are assessed under Stationary. These can include:
- rotating head
- stabilising trunk
- sitting
- raising to sit
- standing on 1 leg
- standing on toes
- initiation of movements such as:
- sit-ups
- push-ups
Locomotion[edit | edit source]
- This measures a child's ability to move from one place to another
- This is the largest section of the PDMS-2 and assesses 89 items in this subtest. Actions that are measured include:
- crawling
- walking
- running
- hopping
- jumping forward
- bearing weight
- rolling
- pushing up
- moving forward
- creeping
- scooting
- pivoting
- stairs climbing
- walking line
- jumping hurdles
- skipping
Object Manipulation[edit | edit source]
- This subtest measures a child's ability to manipulate balls, such as catching, throwing and kicking
- These skills are not apparent until a child is 11 months old, therefor this subtest is only administered in children ages 12 months and older
- This subtest includes 24 items. These include:
- catching a ball
- throwing a ball (overhand and underhand)
- kicking a ball
- hitting target (overhand and underhand)
- bouncing a ball
- catching a bounced ball
Additional Comments[edit | edit source]
In addition, the therapist is encouraged to observe and record the following behaviours[5]:
- the child's interest in the task
- the child's approach to understanding the instructions
- the child's approach to problem solving
- the child's comments or non-verbal response to the task
- the child's latency of response
- the child's use of self-corrections
- the child's preferred hand use in throwing, grasping, etc
- the child's directionality in transferring materials
Grading and Scoring of the PDMS-2[edit | edit source]
The therapist will ask the child to do a specific item and observes how the child is doing the task. Items are scored as 2, 1 or 0.
- 0 = child cannot or will not attempt item or the attempt does not indicate that the specific skill is emerging
- 1 = child's performance shows clear resemblance to item mastery criteria, but does not fully meet the criteria or there are signs of an emerging skill
- 2 = child performs item according to the criteria specified for mastering the skill
It will be too time-consuming to administer the complete the examiner's booklet for every child, so it is recommended to begin or enter the test at the entry point appropriate for the age of the child as marked in the scoring sheet. In the examiner's booklet the different ages are marked in dark blue and this is where the test is "entered" and continued from. The test will begin at the basal level. This is the level where a child receives a score of 2 on three items in a row. The test will be stopped at the ceiling level. This is the level where a child scores 0 on each of three items in a row. This will be done for each subtest.[2]
Note that the skills to be assessed are all in chronological order. Therefor, if a child is not standing yet, the assessment will focus on activities such as rolling or crawling, for example.[3]
The duration of the test is normally around 45 - 60 minutes. Some therapists prefer to do the gross motor and fine motor sections on different days, as doing the them back to back may be too much for the child.
At any point of the PDMS-2, three gross motor subsets will be assessed. If the child is younger than 11 months, the three subsets included will be reflexes, stationary and locomotion. If the child is over 1 year, the three subsets to be assessed will be stationary, locomotion and object manipulation.
Examples of Scoring Subtest Items[edit | edit source]
Reflexes[edit | edit source]
When assessing the walking or stepping reflex in a child younger than 11 months, the therapist holds the child from under his chest up on a table. Allow the child to take some automatic steps. If the child is able to lift one foot and then the other in forward walking within three seconds, a score of 2 can be documented. If the child lifts one foot, but cannot take the steps within three seconds, a score of 1 can be documented. If the child's legs remain still and no steps are taken, a score of 0 can be documented.[3]
Locomotion[edit | edit source]
The child is asked to walk on a line, four inches wide and 8 feet long. If the child is able to walk on the line for six feet, a score of 2 is allocated.[3]
Scoring of the PDMS-2[edit | edit source]
Scoring of the PDMS-2 is documented on the scoring profile or summary form. This is done after the administration of the test. The raw data scores are used in conjunction with the various appendices available in the PDMS-2 reference guide and the following standardised scores can be calculated from these[2]:
- Age equivalents
- Percentiles
- Standard scores
- Gross Motor Quotients
Raw Score[edit | edit source]
The raw score is the sum of the various scores (0,1 and 2) on each of the items. As the test is "entered" at the basal level (where child scores three 2's in a row), it may be assumed (and this assumption is built into the test) that the child also scored 2's on all the items before the start (basal level) of the test. These items also needed to be added as part of the raw score.
Profile Summary[edit | edit source]
The raw data scores are added to the profile summary form. It is key to know the child's age before commencing with the assessment, and with prematurely born children, the corrected age will be used up until 2 years old.
In the examiner's manual, Table A is used to determine the child's percentile rank for the various subtests, based on the raw score achieved. This percentile score can be used as an indication whether physical therapy is needed. The standard score of the various subtests is also extracted from Table A and also added to the profile summary document.
Table B in the examiner's manual will provide the gross motor score. The gross motor score is the sum of the standard scores of each of the subtests. Based on the gross motor score the percentile rank of the child's gross motor abilities is determined.
Table C in the examiner's manual provides the age proficiency of the child for each of the separate subtests such as reflexes, stationary, locomotion and object manipulation.
On the Profile summary page, a graph can then be drawn up, based on all the various scores obtained from Tables A, B and C in the examiner's manual.
Score Interpretation[edit | edit source]
It is important to consider that children from different countries may score differently from the scores provided in the PDMS-2. For example, in India it has been shown that the children's gross motor skill norms are lower than in America.[18] Or in Israel, where baseball is not really played, throwing a tennis ball over hand and under hand might be a bit more difficult for children. Cultural differences may play a part in administering the test and the choice of objects used.
In premature babies, the gross motor deficit may become stronger over time.[8] For example, at 18 months, there may not be much of a deficit, and the child's score may fall within the wide developmental norm. However, at the age of 5 the deficits may be more obvious. Therapists are recommended to consider this in their assessment and treatment of the child and re-evaluate on a regular basis to ensure that the gross motor skill development gap is not getting larger, but just getting smaller.
Therapy goals and planning[edit | edit source]
The Motor Activities Program Book is a very useful tool to consult in the planning of therapy and goal setting. It provides reasons for the child being able to perform the various skills. It also provides useful ways to address developmental delays of each of the items and shows different examples on how to progress. It can provide the therapist with good ideas on how to start of with therapy and address the specific developmental issues and also help with the planning of a home program where parents or guardians can also be involved in helping the child.[3]
Ultimately our goal of therapy is to be able to help the child with developmental delays to be a happier, productive, motor proficient and moving child in his/her environment.[3]
References[edit | edit source]
- ↑ Folio MR, Fewell RR. Peabody developmental motor scales and activity cards. DLM Teaching Resources; 1983.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Folio MR, Fewell RR. PDMS-2 Peabody developmental motor scales second edition. Austin: PRO-ED Inc. 2000.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Taragin, A. Administration and Scoring of the Peabody Developmental Motor Scale - 2. Course, Physioplus 2020.
- ↑ 4.0 4.1 4.2 4.3 Dourou E, Komessariou A, Riga V, Lavidas K. Assessment of gross and fine motor skills in preschool children using the Peabody Developmental Motor Scales Instrument. Eur Psychomotricity J. 2017;9:89-113.
- ↑ 5.0 5.1 Peabody Developmental Motor Scales (PDMS)– 2 Erin Chang, OTS, Karinette Leano, OTS, Thanh Luong, OTS, and Lisa Mireles, OTS. Presentation on Slideshare. Available from https://www.slideshare.net/stanbridge/peabody-developmental-motor-scales-pdms-2 (last accessed 27 August 2020).
- ↑ Holloway JM, Long TM, Biasini F. Relationships between gross motor skills and social function in young boys with autism spectrum disorder. Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association. 2018 Jul;30(3):184.
- ↑ Clutterbuck GL, Auld ML, Johnston LM. High‐level motor skills assessment for ambulant children with cerebral palsy: a systematic review and decision tree. Developmental Medicine & Child Neurology. 2020 Jun;62(6):693-9.
- ↑ 8.0 8.1 Tavasoli A, Azimi P, Montazari A. Reliability and validity of the Peabody Developmental Motor Scales-for assessing motor development of low birth weight preterm infants. Pediatric neurology. 2014 Oct 1;51(4):522-6.
- ↑ Wang M, Mei H, Liu C, Zhang Y, Huixian LI, Yan F. Application of the Peabody developmental motor scale in the assessment of neurodevelopmental disorders in premature infants. Chinese Pediatric Emergency Medicine. 2017 Jan 1;24(10):760-3.
- ↑ Phillips D. Concurrent Validity and Responsiveness of the Peabody Developmental Motor Scales-2 (PDMS-2) in Infants and Children with Pompe Disease undergoing Enzyme Replacement Therapy.
- ↑ Parmar Sanjay KS. Applicability of Peabody developmental Motor Scales PDMS-2 as a developmental assessment scale for Indian children. Occup Ther Int. 2008;2:1-3.
- ↑ Karimi H, Aliabadi F, Hosseini Jam M, Afsharkhas L. Evaluation of motor skills in high risk infants based on Peabody Developmental Motor Scales (PDMS-2). International Journal of Children and Adolescents. 2016 Jan 10;2(1):4-7.
- ↑ Minoliti R, Crepaldi M, Antonietti A. Identifying Developmental Motor Difficulties: A Review of Tests to Assess Motor Coordination in Children. Journal of Functional Morphology and Kinesiology. 2020 Mar;5(1):16.
- ↑ Nicole Edmonds. Spontaneous Stepping Reflex. Published on 22 October 2018. Available from https://www.youtube.com/watch?v=cn7XPS21avE (last accessed 30 August 2020)
- ↑ Healthy Life. Postural Reflexes - Landau. Newborn Reactions (6 months). Published on 16 November 2014. Avaialable from https://www.youtube.com/watch?v=Q5pZNd93qEw. (last accessed 30 August 2020)
- ↑ Kaitlyn Morley. Stationary subset of PDMS-2. Published on 3 June 2015. Available from https://www.youtube.com/watch?v=rlo0gKpQ-ig&t=8s. (last accessed 30 August 2020)
- ↑ Cheyann Walters. Peabody Developmental Motor Scales - 2nd Edition. Published on 16 September 2019. Available from https://www.youtube.com/watch?v=cVW1NrFrs08. (last accessed 30 August 2020)
- ↑ Tripathi R, Joshua AM, Kotian MS, Tedla JS. Normal motor development of Indian children on peabody developmental motor scales-2 (PDMS-2). Pediatric Physical Therapy. 2008 Jul 1;20(2):167-72.