Parotid Gland
Original Editor - Carina Therese Magtibay
Top Contributors - Carina Therese Magtibay
Introduction[edit | edit source]
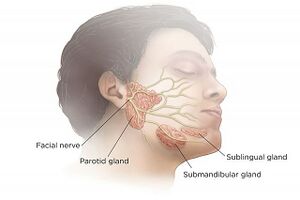
The parotid gland is the largest of three paired major salivary glands. The salivary glands' primary function is to secrete saliva, which plays an important role in lubrication, digestion, immunity, and the overall maintenance of homeostasis within the human body.[1]
Anatomy[edit | edit source]
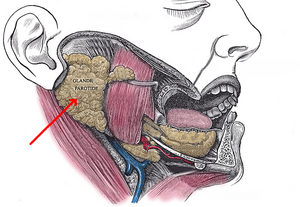
The paired parotid glands are situated in the preauricular region and span from the masseter to the posterior surface of the mandible. It is within the submandibular/digastric triangle of the neck.
The gland is divided into superficial and deep lobes by the facial nerve: [1]
- Superficial lobe - the part of the gland lateral to the nerve and overlies the lateral surface of the masseter muscle.
- Deep lobe - located medial to the facial nerve and lies between the mastoid process of the temporal bone and the mandibular ramus with deep margins resting in the prestyloid compartment of the parapharyngeal space.
Physiology[edit | edit source]
Saliva Formation[edit | edit source]
Saliva volume:[2]
- 90% of total saliva secretions are produced by the parotid, submandibular, and sublingual salivary glands
- 10% are produced by minor salivary glands
In the resting (unstimulated) state, approximately two-thirds of the total volume of the whole saliva is produced by submandibular glands. Upon stimulation, the parotid glands are responsible for at least 50% of the total volume of saliva from the mouth. Sublingual glands contribute to a small percentage, both in the unstimulated or stimulated states of the salivary glands. Minor salivary glands contribute significantly to the lubrication of the oral mucosa because of their high protein content. Unlike some other minor salivary glands which are composed exclusively of mucous cells, parotid glands are serous and produce water-like secretions. Submandibular and sublingual glands are mixed.
In general, acinar (secretory) cells are responsible for the production of the primary saliva. The ductal cells are responsible for further modifications of saliva until it is secreted in the mouth.
Saliva is 99% water and 1% protein and salts. The normal daily production of saliva varies between 0.5 and 1.5 litres. Saliva production decreases during sleep and increases during eating, chewing and other stimulating activities.
Saliva is always hypotonic to plasma. As the whole saliva flow rate increases, the tonicity of the saliva will increase too.[2]
Saliva Functions[edit | edit source]
The functions of the saliva:[2]
- Defensive/buffering capacity
- Remineralization of teeth
- Restoration of soft tissues
- Lubrication capacity
- Digestion
- Antimicrobial capacity
Vascular Supply & Lymphatic Drainage[edit | edit source]
Vascular supply of parotid gland:[1]
- Arterial blood supply: External carotid artery
- Venous outflow: retromandibular vein, which is formed by the maxillary and superficial temporal veins.
There is a high density of lymph nodes within and around the parotid gland. The parotid is the only salivary gland with 2 nodal layers, both drains into the superficial and deep cervical lymph systems. [1]
Autonomic Innervation[edit | edit source]
Salivary gland secretion is mainly controlled by the autonomous nervous system. The glossopharyngeal nerve (CN IX) provides innervation required for secretion of saliva to the parotid gland. CN IX carries preganglionic parasympathetic fibers from the medulla (inferior salivatory nucleus) through the jugular foramen.[1]
Parasympathetic stimulation produces abundant quantities of watery saliva, whereas sympathetic stimulation produces more viscous saliva.[2]
Salivary Gland Disorders[edit | edit source]
Conditions associated with parotid gland and other salivary glands: [3]
- Tumours
- Major salivary glands mainly display epithelial malignancies (carcinomas), with very heterogeneous features and occasional neuroendocrine differentiation.
- Malignant salivary gland tumours represent about 5% of all head and neck cancers, with a slight predominance in men.
- The aetiology of the salivary gland tumour is mainly described by the multicellular theory, by which each cell type can give rise to a specific type of tumour.
- Primary Sjögren’s Syndrome
- It is a systemic autoimmune disease affecting salivary and lacrimal glands typically accompanying other immune system disorders (such as lupus and rheumatoid arthritis)
- Although the pathogenesis of the disease remains largely unknown, the role of the B-lymphocytes appears to be essential in the initiation of the disease.
- Post-Irradiation Syndrome
- One of the most significant side effects of local irradiation is an alteration of salivary glands functionality, resulting in hyposalivation and xerostomia
- Parotitis - can be infectious or due to a variety of inflammatory conditions. Causes of parotitis:[4]
- Mumps - Contagious and can spread by either droplets or directly through oropharyngeal secretions containing the paramyxovirus. Universal immunization has made mumps an uncommon disease in developed countries
- Acute bacterial parotitis - It is uncommon. In the elderly population, it is a significant risk, particularly after abdominal surgery, and can be fatal if it occurs in neonates.
- Chronic bacterial parotitis may be associated with calculi or stenosis of the ducts due to injury. In most cases, chronic diseases are either autoimmune or idiopathic, with superimposed bacterial infection, and should not be regarded as a chronic bacterial infection.
- Human immunodeficiency virus (HIV) - May also cause parotitis with generalized lymphadenopathy and localized enlargement of parotid glands
- Hepatitis C and coxsackievirus - are RNA-bound viruses, able to infect salivary glands and damage the host tissue, leading to xerostomia. One of the main routes of viral spreading is the gland secretion itself and thus transmission through saliva exchange is the major infection mode.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Kochhar A, Larian B, Azizzadeh B. Facial nerve and parotid gland anatomy. Otolaryngologic Clinics of North America. 2016 Apr 1;49(2):273-84.
- ↑ 2.0 2.1 2.2 2.3 Iorgulescu G. Saliva between normal and pathological. Important factors in determining systemic and oral health. Journal of medicine and life. 2009 Jul;2(3):303.
- ↑ Porcheri C, Mitsiadis TA. Physiology, pathology and regeneration of salivary glands. Cells. 2019 Aug 26;8(9):976.
- ↑ Wilson IV J, Gorelik M, Gulliver J, Jaju A, Bhushan B, Rastatter J, Johnston D, Maddalozzo J. Superficial Parotidectomy for Juvenile Recurrent Parotitis. The Laryngoscope. 2023 Jun;133(6):1495-500.