Pancreatic Cancer: Difference between revisions
mNo edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- Jaimin Shah | '''Original Editors '''- Jaimin Shah [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
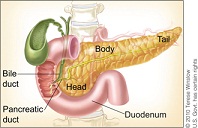
[[Image:Blah.jpg|frame|Anatomical Position of Pancreas]] | [[Image:Blah.jpg|frame|Anatomical Position of Pancreas]] | ||
| Line 9: | Line 9: | ||
Pancreatic cancer is a malignant disease of the pancreas. “Pancreatic adenocarcinoma is a highly lethal disease, which is usually diagnosed in an advanced state.”<ref name="Li et al">Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM. Identification of pancreatic stem cells. Cancer Res 2007;67: 1030-1037</ref> The malignant tumor can be located near the head, body, or the tail of the pancreas. The pancreas is an organ that helps secrete insulin and glucagon which helps control blood glucose levels in the body. Pancreatic cancer is the fourth common cancer among men and the fifth leading cause of cancer in women. There are two types of pancreatic cancers which are exocrine cancer and endocrine cancer. “Pancreatic ductal adenocarcinoma (PDAC) compromises 90 % of pancreatic cancers.”<ref name="Shore et al">Shore S, Vimalachadran D, Raraty MGT, Ghaneh P. Cancer in the elderly: pancreatic cancer. Surgical Onocology 2004;13:201-210</ref> Exocrine pancreatic cancers are the most common of pancreatic cancers. Exocrine pancreatic cancer is involved in the ducts of the pancreas that secrete juices. [[Image:Blah3.jpg|frame|center]] | Pancreatic cancer is a malignant disease of the pancreas. “Pancreatic adenocarcinoma is a highly lethal disease, which is usually diagnosed in an advanced state.”<ref name="Li et al">Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM. Identification of pancreatic stem cells. Cancer Res 2007;67: 1030-1037</ref> The malignant tumor can be located near the head, body, or the tail of the pancreas. The pancreas is an organ that helps secrete insulin and glucagon which helps control blood glucose levels in the body. Pancreatic cancer is the fourth common cancer among men and the fifth leading cause of cancer in women. There are two types of pancreatic cancers which are exocrine cancer and endocrine cancer. “Pancreatic ductal adenocarcinoma (PDAC) compromises 90 % of pancreatic cancers.”<ref name="Shore et al">Shore S, Vimalachadran D, Raraty MGT, Ghaneh P. Cancer in the elderly: pancreatic cancer. Surgical Onocology 2004;13:201-210</ref> Exocrine pancreatic cancers are the most common of pancreatic cancers. Exocrine pancreatic cancer is involved in the ducts of the pancreas that secrete juices. [[Image:Blah3.jpg|frame|center]] | ||
== Prevalence == | == Prevalence == | ||
| Line 16: | Line 14: | ||
“It is estimated 43,140 men and women will be diagnose with and 36,800 men and women will die of cancer of the pancreas in 2010”<ref>U.S National Institutes of Health-National Cancer Institute. SEER Stat Fact Sheets: pancreas. http://seer.cancer.gov/statfacts/html/pancreas.html(accessed 16 March 2011)</ref><br>“Pancreatic cancer is the fourth most common cause of cancer death for men and women in US”<ref name="Farma et al">Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen D, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Annals of Surgical Oncology 2008;15(9):2465-2471</ref> ; about 32,000 people die each year. Pancreatic cancer has the lowest 5-year survival rate (3 to 5 %). Pancreatic cancer is more common in black men and women than whites. “In the United States, the age-adjusted incidence of pancreatic cancer is higher in blacks (14.9 cases per 100,000) than in whites (11.1 cases per 100,000) and it is higher in men (12.8 cases per 100,000) than in women (10.0 cases per 100,000).”<ref name="Maitra et al">Maitra A, Hruban RH. Pancreatic Cancer. Annu Rev Pathol 2008;3:157-188</ref> The peak incidence of pancreatic cancer occurs in the 7th and 8th decade. <br>Pancreatic cancer is rare in people under the age of 45, the risk increases after age of 50. The risk factors associated with pancreatic cancer include family history, genetic syndromes, tobacco use, exposure to chemicals, obesity, diets in high fats and meat, diabetes mellitus, hx of chronic pancreatitis, and hx of partial gastrectomy. “Individuals with a strong family history of pancreatic cancer have a significantly increased risk of developing the disease themselves.”<ref name="Maitra et al" /> “The lifetime risk for developing pancreatic cancer for men and women is 1.27%. 1 in 80 men and women will develop cancer in their lifetime.”<ref name="Chari et al">Chari ST. Detecting early pancreatic cancer-problems and prospects. Semin Oncol 2007;34(4):284-294</ref> | “It is estimated 43,140 men and women will be diagnose with and 36,800 men and women will die of cancer of the pancreas in 2010”<ref>U.S National Institutes of Health-National Cancer Institute. SEER Stat Fact Sheets: pancreas. http://seer.cancer.gov/statfacts/html/pancreas.html(accessed 16 March 2011)</ref><br>“Pancreatic cancer is the fourth most common cause of cancer death for men and women in US”<ref name="Farma et al">Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen D, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Annals of Surgical Oncology 2008;15(9):2465-2471</ref> ; about 32,000 people die each year. Pancreatic cancer has the lowest 5-year survival rate (3 to 5 %). Pancreatic cancer is more common in black men and women than whites. “In the United States, the age-adjusted incidence of pancreatic cancer is higher in blacks (14.9 cases per 100,000) than in whites (11.1 cases per 100,000) and it is higher in men (12.8 cases per 100,000) than in women (10.0 cases per 100,000).”<ref name="Maitra et al">Maitra A, Hruban RH. Pancreatic Cancer. Annu Rev Pathol 2008;3:157-188</ref> The peak incidence of pancreatic cancer occurs in the 7th and 8th decade. <br>Pancreatic cancer is rare in people under the age of 45, the risk increases after age of 50. The risk factors associated with pancreatic cancer include family history, genetic syndromes, tobacco use, exposure to chemicals, obesity, diets in high fats and meat, diabetes mellitus, hx of chronic pancreatitis, and hx of partial gastrectomy. “Individuals with a strong family history of pancreatic cancer have a significantly increased risk of developing the disease themselves.”<ref name="Maitra et al" /> “The lifetime risk for developing pancreatic cancer for men and women is 1.27%. 1 in 80 men and women will develop cancer in their lifetime.”<ref name="Chari et al">Chari ST. Detecting early pancreatic cancer-problems and prospects. Semin Oncol 2007;34(4):284-294</ref> | ||
[[Image:Smoke-that-cigarette.jpg|frame|left|cigarette-- risk factor]] | |||
[[Image:800px-High Fat Foods - NCI Visuals Online.jpg|frame|right|A display of high fat foods such as cheeses, chocolates, lunch meat, french fries, pastries, doughnuts, etc-National Cancer Institute-Unknown Author]] | |||
<br> | <br> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”<ref name="Shore et al" /> | Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”<ref name="Shore et al" /> Symptoms associated with pancreatic cancer include: | ||
*Pain | |||
Pain | *Jaundice | ||
*Digestive Problems | |||
Jaundice | *Blood Clots<br> | ||
*Weight Loss | |||
Digestive Problems | *Abdominal or Back Pain | ||
*Gallbladder Enlargement | |||
Blood Clots<br> | *Dark Urine<br> | ||
*Nausea and Vomiting <br> | |||
Weight Loss | |||
Abdominal or Back Pain | |||
Gallbladder Enlargement | |||
Dark Urine<br> | |||
Nausea and Vomiting <br | |||
Abdominal pain is more common among patients with pancreatic cancer. The pain is insidious in onset originating in the epigastric region moving towards the sides and back<ref name="Shore et al" />. “Pain is the presenting symptom in between 31% and 71% of pancreatic cancer patients”<ref name="Shore et al" /> | |||
[[Image: | [[Image:Abdominal pain.jpg|frame|center]] | ||
[[Image:Jaundice.jpg|frame|center]]Jaundice occurs from compression of the biliary duct. “About 70% of PDACs occur in the head of the pancreas.”<ref name="Shore et al" /> Therefore, patients are more likely to have this as symptomatic manifestation. | |||
<br> | <br> | ||
Advanced Cancer symptoms: | Advanced Cancer symptoms: | ||
*Weakness or very feeling tired | |||
*Loss of appetite or fullness <br> | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
| Line 65: | Line 48: | ||
== Medications == | == Medications == | ||
'''Pain Relief-Opioids''' | '''Pain Relief-Opioids''' | ||
*codeine | |||
*hydrocodone (Vicodin®, Vicoprofen®) | |||
*hydromorphone (Dilaudid®) | |||
*levorphanol (Levo-Dromoran®) | |||
*morphine (Kadian®, MSIR®, MS Contin®, Oramorph-SR®) | |||
*oxycodone (Roxicodone®, OxyIR®, OxyContin®, Percodan®)<br>fentanyl (Duragesic®, Actiq®) | |||
*methadone (Dolophine®) | |||
*tramadol (Ultram®) | |||
*MSIR=morphine sulfate immediate release | |||
*MS Contin=morphine sulfate sustained release | |||
*Oramorph-SR=morphine sulfate sustained release | |||
*Roxicodone=oxycodone immediate release | |||
*OxyIR=oxycodone immediate release | |||
*OxyContin=oxycodone sustained release | |||
*Percodan=oxycodone and immediate release <br> | |||
'''Pain Relief- Non-Opioids''' | '''Pain Relief- Non-Opioids''' | ||
*NSAIDs | |||
*Antidepressants | |||
*Anticonvulsants | |||
== <ref>John Hopkins Medicine-Pancreatic Cancer-Pain Management http://pathology.jhu.edu/pc/TreatmentPain.php?area=tr(accessed 5 April 2010)</ref> <br>Diagnostic Tests/Lab Values == | |||
== <ref>John Hopkins Medicine-Pancreatic Cancer-Pain Management http://pathology.jhu.edu/pc/TreatmentPain.php?area=tr(accessed 5 April 2010)</ref> <br>Diagnostic Tests/Lab Values | |||
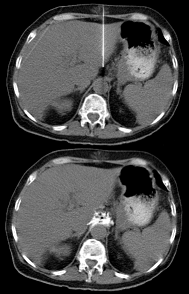
'''Spiral CT '''displays continuous images of the body. Dual contrast enhanced spiral CT provides a continuous enhanced spiral CT that may provide diagnostic rates up to 97% for pancreatic cancer<ref name="Shore et al" />. CT scans can also help determine if a tumor is resectable. The sensitivity for determining resectability with a CT scan is in the range of 68% to 96%<ref name="Shore et al" />. The sensitivity drops to 58% when examining tumors less than 2 cm<ref name="Shore et al" />. “Spiral CT with intravenous contrast of the abdomen is the most common test in the assessment of pancreatic adenocarcinoma.” <ref name="Goodman et al">Goodman CC,Fuller KS. Pathology Implications for the physical therapist. In: Goodman CC, Peterson C. The hepatic, pancreatic, and biliary systems. 3rd ed. St. Louis Saunders Elsevier, 2009.p916-918</ref> [[Image:Ct scan.png|frame|left]] | '''Spiral CT '''displays continuous images of the body. Dual contrast enhanced spiral CT provides a continuous enhanced spiral CT that may provide diagnostic rates up to 97% for pancreatic cancer<ref name="Shore et al" />. CT scans can also help determine if a tumor is resectable. The sensitivity for determining resectability with a CT scan is in the range of 68% to 96%<ref name="Shore et al" />. The sensitivity drops to 58% when examining tumors less than 2 cm<ref name="Shore et al" />. “Spiral CT with intravenous contrast of the abdomen is the most common test in the assessment of pancreatic adenocarcinoma.” <ref name="Goodman et al">Goodman CC,Fuller KS. Pathology Implications for the physical therapist. In: Goodman CC, Peterson C. The hepatic, pancreatic, and biliary systems. 3rd ed. St. Louis Saunders Elsevier, 2009.p916-918</ref> [[Image:Ct scan.png|frame|left]] | ||
| Line 98: | Line 90: | ||
== Etiology/Causes == | == Etiology/Causes == | ||
The specific cause of pancreatic cancer is unknown. Some of the genes investigated in potential related causes include K''-ras ''mutation, ''p''16, ''p''53, DPC4, ''h''MLH1, and ''h''MLH2.<ref name="Goodman et al" /> | |||
"The K-''ras ''mutation has been found in over 90% of tested pancreatic adenocarcinomas."<ref name="Goodman et al" /> The genes ''p''16, ''p''53, and DPCA4 inactive tumor suppressor genes. | "The K-''ras ''mutation has been found in over 90% of tested pancreatic adenocarcinomas."<ref name="Goodman et al" /> The genes ''p''16, ''p''53, and DPCA4 inactive tumor suppressor genes. | ||
| Line 156: | Line 148: | ||
[http://www.medscape.com/viewarticle/472537 Cough as the Presenting Symptom of Pancreatic Adenocarcinoma]<ref name="Richwine et al">Richwine RT, Ahmed N, Mortensen M. Cough a the prestenting symptom of pancreatic adenocarcinoma. J Am Board Fam Med 2004;17(1)</ref> | [http://www.medscape.com/viewarticle/472537 Cough as the Presenting Symptom of Pancreatic Adenocarcinoma]<ref name="Richwine et al">Richwine RT, Ahmed N, Mortensen M. Cough a the prestenting symptom of pancreatic adenocarcinoma. J Am Board Fam Med 2004;17(1)</ref> | ||
== Resources | == Resources == | ||
*National Cancer Institute [http://www.cancer.gov/cancertopics/types/pancreatic www.cancer.gov/cancertopics/types/pancreatic] | |||
National Cancer Institute [http://www.cancer.gov/cancertopics/types/pancreatic www.cancer.gov/cancertopics/types/pancreatic] | *American Cancer Society [http://www.cancer.org/cancer/pancreaticcancer/index www.cancer.org/cancer/pancreaticcancer/index] | ||
American Cancer Society | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10iSX9Fqs0DPh8DIA4HTS4VnJ177tQkbxMecdd_6MR</rss> | <rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10iSX9Fqs0DPh8DIA4HTS4VnJ177tQkbxMecdd_6MR</rss> | ||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Oncology]] [[Category:Medical]] [[Category:Bellarmine_Student_Project]] | ||
Revision as of 07:52, 1 August 2017
Original Editors - Jaimin Shah from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jaimin Shah, Admin, Elaine Lonnemann, Lucinda hampton, WikiSysop, Kirenga Bamurange Liliane, Wendy Walker, Evan Thomas, Kim Jackson and Chelsea Mclene
Definition/Description[edit | edit source]
Pancreatic cancer is a malignant disease of the pancreas. “Pancreatic adenocarcinoma is a highly lethal disease, which is usually diagnosed in an advanced state.”[1] The malignant tumor can be located near the head, body, or the tail of the pancreas. The pancreas is an organ that helps secrete insulin and glucagon which helps control blood glucose levels in the body. Pancreatic cancer is the fourth common cancer among men and the fifth leading cause of cancer in women. There are two types of pancreatic cancers which are exocrine cancer and endocrine cancer. “Pancreatic ductal adenocarcinoma (PDAC) compromises 90 % of pancreatic cancers.”[2] Exocrine pancreatic cancers are the most common of pancreatic cancers. Exocrine pancreatic cancer is involved in the ducts of the pancreas that secrete juices.
Prevalence[edit | edit source]
“It is estimated 43,140 men and women will be diagnose with and 36,800 men and women will die of cancer of the pancreas in 2010”[3]
“Pancreatic cancer is the fourth most common cause of cancer death for men and women in US”[4] ; about 32,000 people die each year. Pancreatic cancer has the lowest 5-year survival rate (3 to 5 %). Pancreatic cancer is more common in black men and women than whites. “In the United States, the age-adjusted incidence of pancreatic cancer is higher in blacks (14.9 cases per 100,000) than in whites (11.1 cases per 100,000) and it is higher in men (12.8 cases per 100,000) than in women (10.0 cases per 100,000).”[5] The peak incidence of pancreatic cancer occurs in the 7th and 8th decade.
Pancreatic cancer is rare in people under the age of 45, the risk increases after age of 50. The risk factors associated with pancreatic cancer include family history, genetic syndromes, tobacco use, exposure to chemicals, obesity, diets in high fats and meat, diabetes mellitus, hx of chronic pancreatitis, and hx of partial gastrectomy. “Individuals with a strong family history of pancreatic cancer have a significantly increased risk of developing the disease themselves.”[5] “The lifetime risk for developing pancreatic cancer for men and women is 1.27%. 1 in 80 men and women will develop cancer in their lifetime.”[6]
Characteristics/Clinical Presentation[edit | edit source]
Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”[2] Symptoms associated with pancreatic cancer include:
- Pain
- Jaundice
- Digestive Problems
- Blood Clots
- Weight Loss
- Abdominal or Back Pain
- Gallbladder Enlargement
- Dark Urine
- Nausea and Vomiting
Abdominal pain is more common among patients with pancreatic cancer. The pain is insidious in onset originating in the epigastric region moving towards the sides and back[2]. “Pain is the presenting symptom in between 31% and 71% of pancreatic cancer patients”[2]
Jaundice occurs from compression of the biliary duct. “About 70% of PDACs occur in the head of the pancreas.”[2] Therefore, patients are more likely to have this as symptomatic manifestation.
Advanced Cancer symptoms:
- Weakness or very feeling tired
- Loss of appetite or fullness
Associated Co-morbidities[edit | edit source]
Diabetes[7]
Medications[edit | edit source]
Pain Relief-Opioids
- codeine
- hydrocodone (Vicodin®, Vicoprofen®)
- hydromorphone (Dilaudid®)
- levorphanol (Levo-Dromoran®)
- morphine (Kadian®, MSIR®, MS Contin®, Oramorph-SR®)
- oxycodone (Roxicodone®, OxyIR®, OxyContin®, Percodan®)
fentanyl (Duragesic®, Actiq®) - methadone (Dolophine®)
- tramadol (Ultram®)
- MSIR=morphine sulfate immediate release
- MS Contin=morphine sulfate sustained release
- Oramorph-SR=morphine sulfate sustained release
- Roxicodone=oxycodone immediate release
- OxyIR=oxycodone immediate release
- OxyContin=oxycodone sustained release
- Percodan=oxycodone and immediate release
Pain Relief- Non-Opioids
- NSAIDs
- Antidepressants
- Anticonvulsants
[8]
Diagnostic Tests/Lab Values[edit | edit source]
Spiral CT displays continuous images of the body. Dual contrast enhanced spiral CT provides a continuous enhanced spiral CT that may provide diagnostic rates up to 97% for pancreatic cancer[2]. CT scans can also help determine if a tumor is resectable. The sensitivity for determining resectability with a CT scan is in the range of 68% to 96%[2]. The sensitivity drops to 58% when examining tumors less than 2 cm[2]. “Spiral CT with intravenous contrast of the abdomen is the most common test in the assessment of pancreatic adenocarcinoma.” [9]
Carbon antigen 19-9 is detected in serum and pancreatic juice. “Carbon antigen 19-9 has a reported sensitivity of 70-90%, a specificity of 90%, PPV of 69%, NPV of 90%.”[2] Carbon antigen 19-9 is produced normal in the body by the pancreas. An elevation of this serum can be indicated for other pancreatic disorders. CA 19-9 is not a useful screening tool for pancreatic cancer in asymptomatic population[2].
TNM staging system classifies pancreatic adenocarcinoma into tumor size, local invasion, regional lymph node metastases, and distant nonnodal metastatic disease.
MRI is equal in comparison to CT scan for being sensitive in detecting pancreatic cancers. “With improved MRI with T1 and T2 imaging and with fast scanning techniques, tumor detection rate is reported up to 90%."[2]
Transabdominal Ultrasound is used for investigating abdominal pain. “The sensitivity of transabdominal US in diagnosing pancreatic cancer has a wide range between 44% and 94%. Transabdominal US is poor in detecting small lesions of less than 1cm, with a sensitivity of 50%.”[2]
Endoscopic Ultrasound is useful in detecting early pancreatic cancer as small as 2-3cm[2]. “A more recent report of series of 89 patients where EUS was compared with surgical and histopathological TNM staging found the overall accuracy to be 69% and 54% for tumor and nodal status.”[2]
Endoscopic retrograde cholangiopancreatography (ERCP) is used for imaging of the pancreatic duct
and biliary system. “The sensitivity and specificity of ERCP is 70-82% and 88-94% in symptomatic patients or those with suspected pancreatic cancer.”[2]
Etiology/Causes[edit | edit source]
The specific cause of pancreatic cancer is unknown. Some of the genes investigated in potential related causes include K-ras mutation, p16, p53, DPC4, hMLH1, and hMLH2.[9]
"The K-ras mutation has been found in over 90% of tested pancreatic adenocarcinomas."[9] The genes p16, p53, and DPCA4 inactive tumor suppressor genes.
hMLH1 and hMLH2 are defective DNA repair genes.[9]
Systemic Involvement[edit | edit source]
Pancreatic cancers are often diagnosed in advanced stages where the cancer has metastasized to other areas. Pancreatic cancers can metastasize to regional lymph nodes, liver, lungs, duodenum, stomach, colon, and anywhere in the abdominal cavity. Pancreatic cancer can spread to the skin as painful nodules. Usual sites for metastases in pancreatic cancer occur in the liver and peritoneal cavity[10].
Medical Management (current best evidence)[edit | edit source]
Treatment of pancreatic cancer is based on the stage of the tumor[9].
Resectable Disease- 15-20%
Locally advanced- 40-45%
Metastatic- 40-45%
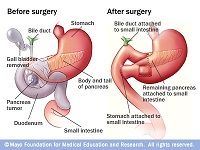
Surgery is the primary option if the pancreatic cancer is resectable. “Surgical resection provides the only curative therapy, only appropriate for a minority of clients.”[9] “Around 9-15% of patients are suitable for potentially curative resection.”[2]
Kausch-Whipples (Pancreaticoduodenectomy) - This procedure involves the removal of the head of the pancreas, a portion of the small intestine, gallbladder, bile duct, and stomach.
Pylorus preserving pancreaticoduodenectomy (PPPD)- This procedure is similar to the Kausch-Whipples except it spares the pylorus. “The preservation of the pyloric sphincter should decrease morbidity and prevent biliary reflux and retention of the duodenal pacemaker should reduce delayed gastric emptying.”[2]
Left pancreatectomy- This procedure involves the removal of the tail of
the pancreas.
Unresectable Disease
Biliary and duodenal obstruction- "Approximately 70-80% of these patients will present with obstructive jaundice and will require decompressionof the biliary tree."[2] Two techniques that are used are endoscopic stenting and operative bypass[2].
Neurolytic celiac plexus block (NCPB)- Nerve fibers are block to control pain symptoms. "A recent large randomised controlled trial showed that neurolytic celiac plexus block improved pain relief in unresectable pancreatic cancer patients when compared with systemic analgesic therapy alone."[2]
Chemotherapy- Involves the use of chemicals in destruction of cancerous cells. "Chemotherapy has been shown to be beneficial in pallative therapy trials."[2] 5-Fluorouracil and Gemcitabine are commonly used agents in treatment of advanced pancreatic cancer[2].
Gene therapy
Immunotherapy
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy management involves helping the patient live a functional life while dealing with pain, fatigue, and weakness. The patient feels he/she is not able to do much because of the disease and its implications. "Disability in patients with advanced cancer often results from bed rest, deconditioning, and neurologic and musculosketal complications of cancer or cancer treatment. Terminally ill patients have a high prevelance of weakness, pain, fatigue, and dyspnea in addition to other symptoms."[11] Improvement in functional ability is necessary for a patient with a diagnosis of cancer to enjoy a quality of life. "Clinical experience suggests that the application of the fundamental principles of rehabilitation medicine is likely to improve care."[11] Physical training had a significant and beneficial effects on reducing fatigue[12].
The physical therapy management will consist of controlling symptoms of pain, reducing fatigue, and strengtening weak muscles. Along with these 3 focal points, impairments should be addressed to improve functional abilities. "When patients are terminally ill, both symptom control and maintenance of function become central aspects of their treatment."[11] Patients who have advanced cancer will have symptoms of pain, fatigue, generalized weakness, dyspnea, delirium, nausea, vomiting, depression, and anxiety[11]. The physical therapist will need to address these symptoms in order for the patient to become independent and reduce the burden of caregivers. "Two-hundred thirty nine of 301 patients had difficulties with activities of daily living. A mean 27% improvement in the Barthel mobility index was recorded following rehabilitation."[11]
Pain is one of the most common symptom of cancer and its advancing state. Severe pain in patients with cancer leads to impaired function. "Knowledge of the biology and natural history of the specific cancer types, including familiarity with common cancer pain syndromes and opioid pharmacology, are important in assessing and managing these patients."[11]
Physical therapy modalities can also be used for treatment of pain but with caution. "The use of physical modalities such as massage, heat, and cold can be implemented at bedside and aid in the pain management of patients."[11] Heat can be utilized when performing ROM exercises in order to reduce the symptoms of pain. "Heat should not be applied to skin areas that are insensitive, have been exposed to radiation, or are atrophic or acutely inflamed."[11] Cold therapy should not also be applied to these areas[11].
Providing the patient with education on about the cancer and its implications can also be beneficial in physical therapy management. Energy conservation and work simplification can also assist patients in reducing and controlling symptoms[11]. Patient education can also include the use of assistive devices if necessary. "Immune function may be improved by moderate exercise."[11] Exercise should be implemented at low intensity levels[11].
Differential Diagnosis[13][edit | edit source]
Abdominal Aortic Aneurysm
Ampullary Carcinoma
Bile Duct Strictures
Bile Duct Tumors
Cholangitis
Pancreatitis, Acute
Cholecystitis
Pancreatitis, Chronic
Choledochal Cysts
Choledocholithiasis
Cholelithiasis
Duodenal ulcers
Gastric ulcers
Neoplasms of endocrine pancreas
Intestinal Ischemia
Gastric Lymphoma
Pancreatic Lymphoma
Heptacellular Carcinoma
Case Reports/ Case Studies[edit | edit source]
A Case Study on the Use of Athletic Performance Strategies in an Elite Athlete’s Management of Pancreatic Cancer[14]
Past Medical History and Pancreatic Cancer Risk: Results From a Multicenter Case-Control Study[15]
New-onset diabetes: a potential clue to the early diagnosis of pancreatic cancer[16]
Cough as the Presenting Symptom of Pancreatic Adenocarcinoma[17]
Resources[edit | edit source]
- National Cancer Institute www.cancer.gov/cancertopics/types/pancreatic
- American Cancer Society www.cancer.org/cancer/pancreaticcancer/index
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=10iSX9Fqs0DPh8DIA4HTS4VnJ177tQkbxMecdd_6MR: Error parsing XML for RSS
References[edit | edit source]
- ↑ Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM. Identification of pancreatic stem cells. Cancer Res 2007;67: 1030-1037
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 Shore S, Vimalachadran D, Raraty MGT, Ghaneh P. Cancer in the elderly: pancreatic cancer. Surgical Onocology 2004;13:201-210
- ↑ U.S National Institutes of Health-National Cancer Institute. SEER Stat Fact Sheets: pancreas. http://seer.cancer.gov/statfacts/html/pancreas.html(accessed 16 March 2011)
- ↑ Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen D, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Annals of Surgical Oncology 2008;15(9):2465-2471
- ↑ 5.0 5.1 Maitra A, Hruban RH. Pancreatic Cancer. Annu Rev Pathol 2008;3:157-188
- ↑ Chari ST. Detecting early pancreatic cancer-problems and prospects. Semin Oncol 2007;34(4):284-294
- ↑ Extermann M. Interaction between comorbidity and cancer. Cancer Control 2007;14(1):13-22
- ↑ John Hopkins Medicine-Pancreatic Cancer-Pain Management http://pathology.jhu.edu/pc/TreatmentPain.php?area=tr(accessed 5 April 2010)
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Goodman CC,Fuller KS. Pathology Implications for the physical therapist. In: Goodman CC, Peterson C. The hepatic, pancreatic, and biliary systems. 3rd ed. St. Louis Saunders Elsevier, 2009.p916-918
- ↑ Borad MJ, Saadati H, Lakshmipathy A, Campbell E, Hopper P, Jameson G, Von Hoff DD, Wasif Saif M. Skeletal metastases in pancreatic cancer: a retrospective study and review of the literature. Yale Journal of Biology and Medicine 2009;82:1-6
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 Santiago-Palma J, Payne R. Palliative care and rehabilitation. Cancer Supplement 2001;92(4):1049-1052
- ↑ van Weert EV, May AM, Korstjens I, Post WJ, van der Schans CP, van den Borne B, Mesters I, Ros WJG, Hoekstra-Weebers JEHM. Cancer-related fatigue and rehabilitation: a randomized controlled multicenter trial comparing physical training combined with congnitive-behavioral therapy with physical training only and with no intervention. Physical Therapy 2010;90(10):1413-1425
- ↑ Dragovich T, Erickson RA,Larson CR. Pancreatic Cancer.emedicine on medscape.http://emedicine.medscape.com/article/280605-overview. Updated March 11, 2011. Accessed April 26, 2011.
- ↑ Harris BE. A case study on the use of athletic performance strategies in an elite athlete's management of pancreatic cancer. Boise State University Theses and Dissertations 2010.
- ↑ Maisonneuve P, Lowenfels AB, Bueno-De-Mesquita HB, Ghadirian P, Baghurst PA, Zatonski WA, Miller AB, Duell EJ, Boffetta P, Boyle P. Past medical history and pancreatic cancer risk: results from a multicenter case-control study. Ann Epidemiol 2010;20:92-98
- ↑ Pannala R, Basu A, Petersen GM, Chari ST. New-onset diabetes: a potential clue to the early diagnosis of pancreatic cancer. Lancet Oncol 2009;10:88-95
- ↑ Richwine RT, Ahmed N, Mortensen M. Cough a the prestenting symptom of pancreatic adenocarcinoma. J Am Board Fam Med 2004;17(1)