Pain Neuroscience Education (PNE) for Low Back Pain
Introduction[edit | edit source]
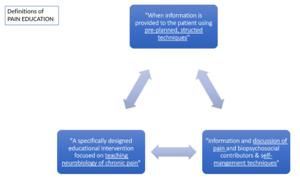
Pain Education is an intervention designed to help individuals experiencing chronic pain understand what is happening within their own body's, it aims to reconceptualize pain as a protective output of the brain rather than it being an accurate measure of tissue damage.[1]
The way it is defined varies dependent on literature but the principles remains the same . [2][3][4]
Pain education is consistently recommended as an intervention for MSK conditions as it can be used for both prevention and treatment[4][5] . It provides a foundation for better self-informed treatment choices as well as self-monitoring & self-management activities. [4]
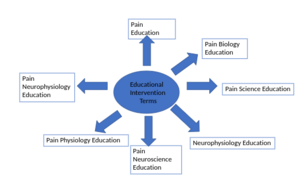
Education Intervention Terms :[4][edit | edit source]
Key messages in Pain Education: [6][3][2][edit | edit source]
- Acknowledgement & acceptance of persistent pain
- Reframing of unhelpful beliefs about LBP
- Building a support team
- Pacing (behavioural therapy technique)
- Learning to prioritise and plan days
- Setting Goals/Action Plans
- Being patient with one-self
- Learning relaxation skills
- Incorporating Stretching & Exercise
- Having back up plans for set backs
A systematic review and meta-analysis by Traeger et al [2], provides evidence that all these concepts applied in patient education can reassure patients with chronic pain and such effects are maintained up to 12 months
Pain Neuroscience Education[edit | edit source]
Pain neuroscience education (PNE) consists of educational sessions describing the neurobiology and neurophysiology of chronic pain and processing with particular focus on the role of the Central Nervous System on chronic pain and deemphasizing anatomical issues.[7]
It promotes patient understanding of chronic pain and changes maladaptive thoughts and cognitions , for instance, pain catastrophizing[7]. Through addressing these neurophysiological and neurobiological contributors of pain, PNE has been found to have a short and long-term positive effects on multiple factors , such as pain, disability , catastrophizing , overall physical performance and demand on healthcare systems[8]
The key messages found within general pain education are also reinforced in pain neuroscience although the mode of delivery can vary. For key concepts of PNE - see here
Pain Neuroscience Education delivery strategies: [9][edit | edit source]
- Online module format
- Single vs Multiple sessions
- One-to-One vs Group sessions
- Written vs Online Videos
- Metaphors
- Stories
- Videos
Low Back Pain[edit | edit source]
Low Back Pain (LBP) has several definitions dependent on the source but majority of literature defines it as "pain, muscle tension or stiffness localised below the costal margin and above the inferior gluteal folds typically, accompanied with or without pain and or neurological symptoms in one or both lower limbs" [10] [11]For majority of individuals with LBP , it is not possible to identify a specific nociceptive cause and only a small proportion have well understood pathological causes[11] i.e. vertebral fracture , malignancy etc , hence why it is commonly termed as 'non-specific'. It can be categorised in 3 subtypes : Acute , Sub-Acute and Chronic. Key concepts , anatomical structures and possible pathological causes - see here
Low Back Pain is ranked as the highest leading cause of disability globally [3][11].
- 50-80% of adults experience LBP, it is a common disorder which impacts 2 billion people globally[12][13]
- It is uncommon within the 1st decade of an individuals life but increases steeply during teenage years with around 40% adolescents in high, middle and low income countries reporting of LBP.[11]
- Studies have shown that the 1 year incidence of people experiencing LBP ranges from 1.5%-36% and 6.3%-15.4%[14]
- Patients who experience acute LBP are found to have a high prognosis , however studies have found recurrence is common for 33% of individuals within 12 months and within a population of approximately 20-40% , LBP will become persistent and disabling (chronic)[14].
- In 2015, the global prevalence of activity -limiting LBP was 7.3%, 540 million people were affected at any one time.[11]
Some studies suggest that there are predisposing factors such as age , gender , weight , occupation and particularly, occupational related musculoskeletal (msk) disorder/ repetitive strain injury [11] [14]. Occupational induced LBP is estimated to cause 21.7 million Disability Adjusted Life Years (DALYs)[15].
Low Back Pain is characterized by a range of biophysical , psychological and social dimensions . Individuals with LBP , particularly chronic , are known to experience poor sleep quality and health perception , worsened quality of life (QoL) and depressive symptoms [12]. Several studies and researchers have found that LBP results in fear-avoidance (i.e. kinesiophobia)[8], anxiety, catastrophizing and as well as it being the biggest reason for leave and absenteeism at work[14][13] , it also causes an overuse / strain of the healthcare systems , with approximately 68% of individuals visiting a physician over a year.[13]
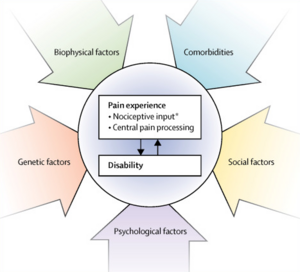
Biopsychosocial Theory[edit | edit source]
The biopsychosocial theory and model is one of the fundamental theories within pain neuroscience education[9] and it as a intervention for chronic msk disorders. It has been particularly vital in the transitioning and evolving beliefs of LBP.
Previously , LBP was mainly understood from a biomedical approach which meant that clinicians held biomedically oriented beliefs and offered advice that promoted less activity and more time off work[16] Research has since shown that such advice was interpreted by patients as indicating activity to be dangerous hence leading into factors such as fear-avoidance , catastrophising etc[12].
Through several research, over the past 15-20 years , clinicians have been encouraged to shift management of chronic msk pain from a biomedical/biomechanical approach to the biopsychosocial[12], as psychosocial factors play an important role within individuals who experience chronic pain and has an impact on their function and QoL. All the psychological attributes associated with LBP such as fear-avoidance , catastrophic thinking and familial & social stress (stress-pain cycle) can increase the risk of physical disability which manifests as reduced functional capacity, avoidance of usual activities including work as well as impaired societal and recreational participation[17].
A systematic review in 2021 by Siddall et al concluded that there was a major barrier to exercise in patients with chronic pain due to kinesiophobia Patients with low knowledge on the neurophysiology display high kinesiophobia and ultimately , it has been found that high levels of kinesiophobia is associated with reduced exercise adherence and an increase in pain & disability [8] , hence why pain neuroscience education is useful, as it aims to increase an understanding of the biopsychosocial nature of pain and the adaptability of the body [9]
Evidence[edit | edit source]
Clinician perspective[edit | edit source]
A clinician’s perspective to a treatment would concern assessing the relevant outcome measure to determine the effectiveness from that treatment / intervention. In the context of PNE and LBP, the consensus amongst research is that pain, and disability are dominant outcome measures used and can be applied through different questionnaires to evaluate these outcomes. Other outcome measures used in research include psychosocial elements to them such as quality of life, self-efficacy, Catastrophizing and kinesiophobia.
Outcome measures to evaluate the use of PNE on LBP[edit | edit source]
QOL - EQ-5D
Kinesiophobia – Tampa scale
Catastrophizing - pain catastrophizing scale
PNE[edit | edit source]
Systematic review evidence that investigated the effect PNE has on musculoskeletal and low back pain in patients included studies that evaluated the effect of PNE as a stand alone intervention. 2 studies from Woods and Hendrick (2018) and 5 studies from Louw et al (2016) contained information regarding PNE's individual effect. Results showed that no study was able significantly decrease pain and there was low to moderate evidence for improving disability in the short term or at all in regards to given outcome measures in the reviews[18][19].
Whilst PNE's effectiveness on physical attributes are not as applicable as a stand-alone intervention, PNE's stand-alone effect on psychosocial components shows promising evidence to support its use. Evidence suggests that PNE can improve other elements that can facilitate function such as kinesiophobia and illness perceptions [20]. However, limited evidence, although favourable, can't solely justify the individual application of PNE therefore future research needs to investigate this further.
PNE and Physiotherapy[edit | edit source]
Clinicians will often incorporate the application of PNE in alignment with usual physiotherapy care (manual therapy/exercise prescription) as to utilise a multi-modal approach when treating chronic back pain [21]
There is compelling evidence to support the use of PNE along with physiotherapy interventions to have short term improvements on pain. Systematic review & meta analysis evidence looking at PNE and physiotherapy in the treatment of chronic lower back pain found for pain there was low to moderate evidence in the short term[18][22]. Additional evidence also highlights its moderate effects on improving disability [22][19][23]. Information in the mentioned evidence does not specify what type of physiotherapy intervention is superior to one another.
However, emerging research has found propitious evidence to support PNE alongside motor control training (MCT) as its suggested to deliver more effective results in improving pain and disability compared to current best-evidence physiotherapy care [24][25] . MCT has also shown better results compared to core stability exercise [26], although this result was exclusive to women due to the population studied thus limiting its validity.
With limited evidence it is hard to distinguish which intervention format is more effective to combine with PNE and therefore warrants the need for further research to determine clear differences in the interventions. Updating current systematic evidence could help establish clearer findings.
PNE and physiotherapy effect on psychological aspects of patients showed potential improvements to kinesiophobia and catstrophization but improvements were negligible failing to demonstrated clinically meaningful changes[18] .
Type of physiotherapy care used with PNE[edit | edit source]
- Manual therapy
- Exercise prescription
- Aquatic therapy
- Paced/Graded exposure
- Acupuncture/dry needling
- Motor control training
Patient perspective[edit | edit source]
A patient’s treatment perspective involves two main components: the patient’s views about their health (e.g. what the condition is, what its causes are and how serious it is to the patient) and the patient’s values (e.g. what will help them most and how this can be achieved).
Patients values and beliefs[edit | edit source]
Minimal research investigates the patient’s values in learning about their pain. However, a mixed-methods survey found that patients believed PNE was necessary for their improvement of persistent pain[28]. PNE as an intervention provides a coherent biological explanation for how emotions such as stress can initiate a hormonal response which can sensitise neural processes associated with pain[19]. Pain reconceptualisation helps manage stress and anxiety, limiting the pain induced by these emotions. Although there’s limited research in this area, the mixed-methods review provides contextualised insight into qualitative data on the research question, providing a foundation for refining PNE to focus on pain concepts deemed most valuable to people with pain and use patient-centred language to best communicate the concepts.
A common belief that follows pain is the concept that pain means damage; therefore, learning that pain does not indicate bodily or tissue damage can help manage patients’ pain[28]. These findings are consistent with the fear-avoidance model, which describes how individuals may develop musculoskeletal pain due to avoidant behaviour based on fear[29]. When a patient is gradually exposed to fear situations, understanding fear-avoidance concept leads to less fear of injury and less avoidance of movement and behaviours. If a patient engages, pain may become less threatening, changing their priority from pain control to valued life goals, e.g., decreasing disability and kinesiophobia, through using positive connotations such as "understanding that even though it hurts, it is not a sign of damage"[19][30].
Future research[edit | edit source]
There are still areas within PNE that need to be further researched. One shortcoming is the heterogeneity of studies as age range, gender, and education don’t tend to be considered. Bilterys et al. (2022)[31] found no clinically meaningful differences in the effectiveness of PNE between educational levels. However, this has minimal research and would be beneficial to further understand patient factors affecting PNE.
Education[edit | edit source]
Teaching[edit | edit source]
There is limited research which evaluates the most effective use of PNE. Typically, PNE sessions are delivered in fifteen-to-thirty-minute sessions once or twice a week for four to six weeks[32] [33]. They aim to decrease inappropriate beliefs and maladaptive behaviours associated with their chronic pain experiences. Teaching is most effective if taught by an experienced clinician[34].
Delivery[edit | edit source]
Patients should receive individualised guidelines and sessions are primarily delivered as verbal one-to-one sessions; however, new research suggests that it is beneficial to promote and conduct PNE in a group-based setting[35]. Group strategy can be a powerful tool in encouraging values such as group feelings, improving self-esteem, and increasing adherence to the individual strategy. For example, a consequence of chronic pain may be kinesiophobia (the fear of movement). Romm et al. (2011) concluded that group-based interventions significantly affect kinesiophobia through biopsychosocial interventions and learning theories such as observational learning.
Patient-Clinician Relationship[edit | edit source]
To maximise the effectiveness of PNE, it is essential to build rapport with the patient. Research has shown that the patient-clinician relationship has a statistically significant effect on healthcare outcomes[36]. Within the PNE intervention, the patient-clinician relationship is vital as the patient needs to trust and comply with the instructions given by the practitioner to aid their recovery.
Clinical application of PNE[edit | edit source]
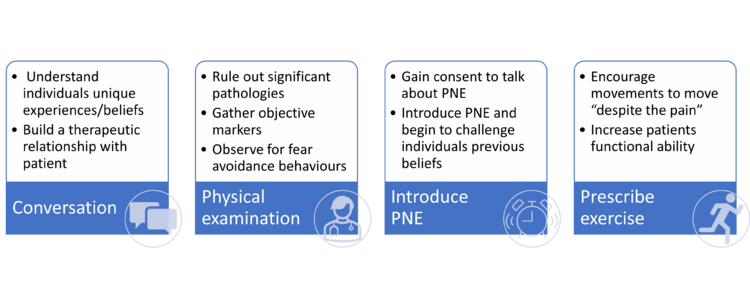
One aspect of PNE within the literature with little controversy is that PNE produces the most favourable outcomes when used in conjunction with more 'traditional' physiotherapy treatments. Utilising the current literature, in particular a study from Louw et al. (2016)[37], we have outlined a strategy which clinicians can utilise to incorporate PNE into their practice.
First session[edit | edit source]
Within the first session, a comprehensive assessment of the patient will be completed. This is like a 'traditional physiotherapy assessment' as it gathers both subjective and objective information which the clinician can utilise to inform their diagnosis and treatment. We propose the first session should be split into 4 sections which should total to around 1 hour:
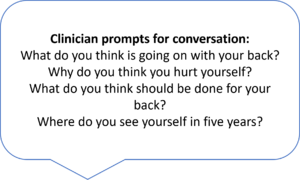
- Conversation/interview (~25-30mins): Initially clinicians should have a conversation with the patient where they predominantly listen to the patient, gathering information about their experiences, suffering and beliefs. This part should not be rushed, and adequate time is needed for the patient to tell their own story. Within this time the clinician can take note of any issues/beliefs which the patient mentions which may need to be addressed in later PNE sessions.
- Physical examination (~10 mins): It is important that significant pathologies are ruled out to ensure that there is no underlying sinister pathology. Physical examination will also give us objective markers that we can utilise to track the progress of individuals to see if treatment is effective. The results from this examination should be conveyed to the patient, with emphasis on the use of clinician language to avoid terms like “wear and tear” which have negative connotations.
- Introduction to PNE (~10-15mins): Depending on the time availability of the clinician following a thorough assessment, PNE can then be briefly introduced to the patient. A good way to start the conversation is asking “Has anyone explained to you why you are still experiencing pain?”. If the patient is interested in learning more this is when a brief metaphor can be used to start to explain the hyper sensitive nervous system which is contributing to their pain. A common metaphor used is an oversensitive alarm clock (described below), however there is a number of metaphors used within pain education and research has found that no individual story or metaphor is superior to another [38]. 'Tame the beast' by Lorimer Moseley is another popular metaphor which can be utilised by patients, one benefit to this metaphor is that it has a patient centred video which clinicians can signpost a patient to if they are short of time in the initial session.[39]
4. Exercise prescription (~10-15mins): As PNE is most effective when used in conjunction with other therapies, simple exercises should be given to the patient to encourage movement. The patient should perform the exercise during the session and the clinician should discuss the patients perception of the exercise, challenging any inaccurate beliefs utilising the PNE metaphor.
Depending on the time available to the clinician this initial session may need to be split into two sessions, however the sessions should then be delivered within a short time frame of each other.
The oversensitive alarm clock[edit | edit source]
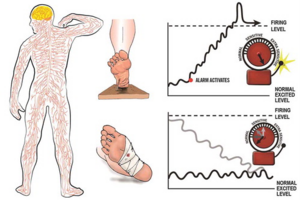
To begin with we must explain to patients the complexity of the nervous system; there are more than 400 individual nerves which all connect like roads, if they were all combined and laid out they would cover more than 45 miles (ref).We can then explain how a healthy nervous system works, introducing the metaphor of an alarm clock:
"When we step on a pin while barefoot we need to know about it so that we can remove the danger and take care of ourselves. The nervous system works like an alarm clock, sending a message to the brain producing pain so that we can take action such as removing the pin from our foot. The alarm will then calm down and is ready to warn you of any future danger such as stepping on another pin." Using illustrations will help to explain this metaphor. We can then apply this to the patients presenting problem.
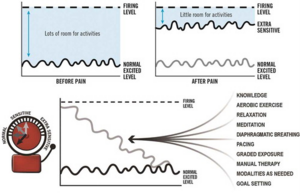
We can then explain to the patient that in approximately 1 in 4 people the alarm system does not calm down and stays extra sensitive: "Before you had the onset of pain the alarm clock had lots of space for activities before the alarm would be triggered but because it is very sensitive there is little room for activities before the alarm goes off. (That explains why your back hurts after standing up for 5 minutes.)" Again the use of an illustrations can help a patient to understand this.
We can then round up the brief introduction by explaining that there is a lot of factors that are contributing to this hypersensitivity, which you can then discuss in later sessions. It is also important that you explain that there are strategies we can use to calm the alarm clock down to give the patient the reassurance that things will get better. "There are things that are making your alarm clock extra sensitive and also strategies we can use to help calm your alarm clock down. We can discuss these in your later sessions but the main thing is that we start to calm your alarm clock down to give you more room for activities."
'Homework'[edit | edit source]
It is important that we encourage patients to take an active role in their own recovery. We should provide patients with the relevant tools to enable this and increase their self-efficacy. Giving patients a few simple tasks can help to promote this. These can include:
- Question Generation: Encourage the patient to write down any questions that they may have regarding pain and the PNE material covered in the session. This helps to remove doubts and increase their understanding of pain experiences.
- Encourage exercises: Exercise help to enhance movement and increase function. A focus on breathing and relaxation should be emphasised during the exercise with reference to PNE and relaxation of the hypersensitive nervous system.
- Aerobic exercise: Starting very small in an exercise of their own choice (walking, swimming, cycling, running etc.) patients should be encouraged to participate in aerobic exercise. The benefits should be explained to the patient in terms of the down regulation of the sensitised nervous system.
- Set goals: Patient should be encouraged to list 5 goals they wish to achieve prior to the next session. Asking the patient “If you could flip a switch and get rid of all your pain, what would you do again?”
Clinicians should use their own judgement when giving patient tasks to complete at home, some proactive patients will complete all tasks before the next session, while those with low self efficacy may be overwhelmed when given a large number of tasks. One way to combat this is to give patient 1-2 tasks at a time, a clinician should use their own judgement to determine the tasks to prescribe and what tasks can be introduced in later sessions.
Subsequent sessions[edit | edit source]
Subsequent session should be individualised to patients and their journey with PNE. The content of these sessions are dependent on what was covered in the previous session e.g. if there was not time in the last session to discuss the importance of aerobic exercise or to teach the patients relaxed breathing techniques then this could be a priority for the next session. A useful structure for later PNE could be:
- Question and answer: Discuss any questions the patient had about the previous session. If patients do not have any questions the clinician could ask the patient about what they understood from the previous session, this can help identify any areas which patients were unsure of or had forgotten which can then be revisited.
- Progress PNE: New metaphors, pictures or information can be discussed with the patient. These should be relevant to the patients experience or findings.
- Review goals: Break the patients goals down into SMART goals. This encourages pacing and graded exposure which can help to motivate patients throughout their journey. Each session the goals should be reviewed, and patient should be encouraged to progress to the next stage if appropriate.
- Traditional therapy: The clinician should use their own clinical judgement to determine if the patient would benefit from other treatments such as manual therapy. The exercises from previous session should be reviewed and new exercises prescribed to encourage increase function.
References[edit | edit source]
- ↑ 5. Traeger AC, Moseley GL, Hubscher M, Lee H, Skinner IW, Nicholas MK, et al. Pain education to prevent chronic low back pain: a study protocol for a randomised controlled trial. BMJ Open. 2014 Jun 2;4(6):e005505–5.
- ↑ 2.0 2.1 2.2 2. Traeger AC, Hübscher M, Henschke N, Moseley GL, Lee H, McAuley JH. Effect of Primary Care–Based Education on Reassurance in Patients With Acute Low Back Pain: Systematic Review and Meta-analysis. JAMA Internal Medicine [Internet]. 2015 May 1;175(5):733–43. Available from: https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2204032
- ↑ 3.0 3.1 3.2 4. Traeger AC, Lee H, Hübscher M, Skinner IW, Moseley GL, Nicholas MK, et al. Effect of Intensive Patient Education vs Placebo Patient Education on Outcomes in Patients With Acute Low Back Pain. JAMA Neurology. 2019 Feb 1;76(2):161.
- ↑ 4.0 4.1 4.2 4.3 13. Ziegler A-M, Minkalis AL, Langdon ER, Vining R. Learning the neurobiology of pain: A scoping review of pain education from an instructional design perspective. Patient Education and Counseling. 2021 Sep;
- ↑ 14. NICE. Recommendations | Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain | Guidance | NICE [Internet]. www.nice.org.uk. 2021. Available from: https://www.nice.org.uk/guidance/ng193/chapter/Recommendations
- ↑ 15. [email protected] TPT -. Pain Self Management by Pete Moore | The Pain Toolkit [Internet]. www.paintoolkit.org. 2022. Available from: https://www.paintoolkit.org/
- ↑ 7.0 7.1 6. Andias R, Neto M, Silva AG. The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: a school-based pilot, randomized and controlled study. Physiotherapy Theory and Practice. 2018 Jan 10;34(9):682–91.
- ↑ 8.0 8.1 8.2 7. Siddall B, Ram A, Jones MD, Booth J, Perriman D, Summers SJ. Short-term impact of combining pain neuroscience education with exercise for chronic musculoskeletal pain. Pain. 2021 Apr 9;Publish Ahead of Print.
- ↑ 9.0 9.1 9.2 8. Shala R, Roussel N, Lorimer Moseley G, Osinski T, Puentedura EJ. Can we just talk our patients out of pain? Should pain neuroscience education be our only tool? Journal of Manual & Manipulative Therapy. 2021 Jan 2;29(1):1–3.
- ↑ 3. Ho EK-Y, Chen L, Simic M, Ashton-James CE, Comachio J, Wang DXM, et al. Psychological interventions for chronic, non-specific low back pain: systematic review with network meta-analysis. BMJ. 2022 Mar 30;e067718.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 1. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. The Lancet. 2018 Jun;391(10137):2356–67.
- ↑ 12.0 12.1 12.2 12.3 9. Rufa A, Dolphin M, Adams K, Brooks G. Factors associated with the low back pain-related attitudes and beliefs of physical therapists. Musculoskeletal Science and Practice. 2022 Apr;58:102518.
- ↑ 13.0 13.1 13.2 18. Jana A, Paul A. Epidemiology of low back pain: A literature review. ~ 233 ~ International Journal of Physical Education, Sports and Health [Internet]. 2019 [cited 2022 May 23];6(3). Available from: https://www.kheljournal.com/archives/2019/vol6issue3/PartD/6-3-24-123.pdf
- ↑ 14.0 14.1 14.2 14.3 16. Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatology International. 2019 Mar 8;39(4):619–26.
- ↑ 17. Aschalew AB, Yosef T. Health Related Quality of Life among Cross-Country Truck Drivers with Lower Back Pain: Institution Based Cross-Sectional Study, Ethiopia. Epidemiology: Open Access [Internet]. 2019 Jan 30 [cited 2022 May 23];9(1). Available from: https://www.omicsonline.org/open-access/health-related-quality-of-life-among-crosscountry-truck-drivers-with-lower-back-pain-institution-based-crosssectional-study-ethiop-2161-1165-1000370-108151.html
- ↑ 10. Houben RMA, Gijsen A, Peterson J, de Jong PJ, Vlaeyen JWS. Do health care providersʼ attitudes towards back pain predict their treatment recommendations? Differential predictive validity of implicit and explicit attitude measures. Pain. 2005 Apr;114(3):491–8.
- ↑ 3. Ho EK-Y, Chen L, Simic M, Ashton-James CE, Comachio J, Wang DXM, et al. Psychological interventions for chronic, non-specific low back pain: systematic review with network meta-analysis. BMJ. 2022 Mar 30;e067718.
- ↑ 18.0 18.1 18.2 Wood, L. and Hendrick, P.A. (2018). A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. European Journal of Pain, 23(2), pp.234–249. doi:10.1002/ejp.1314.
- ↑ 19.0 19.1 19.2 19.3 Louw, A., Zimney, K., Puentedura, E.J. and Diener, I. (2016). The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiotherapy Theory and Practice, 32(5), pp.332–355. doi:10.1080/09593985.2016.1194646.
- ↑ Malfliet, A., Kregel, J., Meeus, M., Roussel, N., Danneels, L., Cagnie, B., Dolphens, M. and Nijs, J. (2017). Blended-Learning Pain Neuroscience Education for People With Chronic Spinal Pain: Randomized Controlled Multicenter Trial. Physical Therapy, 98(5), pp.357–368. doi:10.1093/ptj/pzx092.
- ↑ Saracoglu, I., Arik, M.I., Afsar, E. and Gokpinar, H.H. (2020). The effectiveness of pain neuroscience education combined with manual therapy and home exercise for chronic low back pain: A single-blind randomized controlled trial. Physiotherapy Theory and Practice, pp.1–11. doi:10.1080/09593985.2020.1809046.
- ↑ 22.0 22.1 Siddall, B., Ram, A., Jones, M.D., Booth, J., Perriman, D. and Summers, S.J. (2021). Short-term impact of combining pain neuroscience education with exercise for chronic musculoskeletal pain. Pain, Publish Ahead of Print. doi:10.1097/j.pain.0000000000002308.
- ↑ Puentedura, E.J. and Flynn, T. (2016). Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiotherapy Theory and Practice, 32(5), pp.408–414. doi:10.1080/09593985.2016.1194663.
- ↑ Malfliet, A., Kregel, J., Coppieters, I., De Pauw, R., Meeus, M., Roussel, N., Cagnie, B., Danneels, L. and Nijs, J. (2018). Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain. JAMA Neurology, 75(7), p.808. doi:10.1001/jamaneurol.2018.0492.
- ↑ Rabiei, P., Sheikhi, B. and Letafatkar, A. (2020). Comparing pain neuroscience education followed by motor control exercises with group‐based exercises for chronic low back pain: a randomized controlled trial. Pain Practice. doi:10.1111/papr.12963.
- ↑ Gorji, S.M., Mohammadi Nia Samakosh, H., Watt, P., Henrique Marchetti, P. and Oliveira, R. (2022). Pain Neuroscience Education and Motor Control Exercises versus Core Stability Exercises on Pain, Disability, and Balance in Women with Chronic Low Back Pain. International Journal of Environmental Research and Public Health, 19(5), p.2694. doi:10.3390/ijerph19052694.
- ↑ Physiotutors. Lumbar Movement Control Exercises | Motor Control Impairment. Available from: https://www.youtube.com/watch?v=x6mRy22eYkA [Accessed 22/05/22]
- ↑ 28.0 28.1 Leake, H.B., Moseley, G.L., Stanton, T.R., O'Hagan, E.T. and Heathcote, L.C., (2021). What do patients value learning about pain? A mixed-methods survey on the relevance of target concepts after pain science education. Pain, 162(10), pp.2558-2568.
- ↑ Cosio D. (2019) Fear-Avoidance and Chronic Pain: Helping Patients Stuck in the Mouse Trap. Practical Pain Management, 19(5), Available at:https://www.practicalpainmanagement.com/treatments/psychological/cognitive-behavioral-therapy/fear-avoidance-chronic-pain-helping-patients
- ↑ Louw, A., Diener, I., Butler, D.S. and Puentedura, E.J., (2011). The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation, 92(12), pp.2041-2056.
- ↑ Bilterys, T., Kregel, J., Nijs, J., Meeus, M., Danneels, L., Cagnie, B., Van Looveren, E. and Malfliet, A., (2022). Influence of education level on the effectiveness of pain neuroscience education: A secondary analysis of a randomized controlled trial. Musculoskeletal Science and Practice, 57, p.102494.
- ↑ Evidence In Motion (2022). Pain Neuroscience Education 101. Evidence in motion. Available at: https://evidenceinmotion.com/wp-content/uploads/2020/02/PNE101.pdf
- ↑ Meeus, M., Nijs, J., Van Oosterwijck, J., Van Alsenoy, V. and Truijen, S., (2010). Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Archives of physical medicine and rehabilitation, 91(8), pp.1153-1159.
- ↑ Watson, J.A., Ryan, C.G., Cooper, L., Ellington, D., Whittle, R., Lavender, M., Dixon, J., Atkinson, G., Cooper, K. and Martin, D.J., (2019). Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. The journal of pain, 20(10), pp.1140-e1.
- ↑ Romm, M.J., Ahn, S., Fiebert, I. and Cahalin, L.P., (2021). A Meta‐Analysis of Therapeutic Pain Neuroscience Education, Using Dosage and Treatment Format as Moderator Variables. Pain Practice, 21(3), pp.366-380.
- ↑ Kelley, J.M., Kraft-Todd, G., Schapira, L., Kossowsky, J. and Riess, H., (2014). The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PloS one, 9(4), p.e94207.
- ↑ Louw, A., Zimney, K., O’Hotto, C. and Hilton, S. (2016). The clinical application of teaching people about pain. Physiotherapy Theory and Practice, 32(5), pp.385–395. doi:10.1080/09593985.2016.1194652.
- ↑ Louw, A., Puentedura, E.J., Diener, I., Zimney, K.J. and Cox, T. (2019). Pain neuroscience education: Which pain neuroscience education metaphor worked best? South African Journal of Physiotherapy, 75(1). doi:10.4102/sajp.v75i1.1329.
- ↑ Lorimer Moseley. Tame The Beast — It’s time to rethink persistent pain. YouTube. Available at: https://www.youtube.com/watch?v=ikUzvSph7Z4&t=204s [Accessed 19 May 2022].