Pain Behaviours
Top Contributors - Joanne Garvey, Kapil Narale, Aminat Abolade, Jo Etherton, Lucinda hampton, Melissa Coetsee, Evan Thomas, Tarina van der Stockt, Kim Jackson, Carina Therese Magtibay, Aya Alhindi, Rachael Lowe and Lauren Lopez
Introduction[edit | edit source]
When we think of pain behaviours we tend to think of our behaviour to pain but the type of pain and the and how they present is also an important factor in understanding pain. Human Pain Behaviours - much more than a sensory perception of tissue injury. Pain is a complex and unpleasant multidimensional experience of the self associated with perceived tissue threat[1].
Pain types differ. There are 3 widely accepted pain types relevant for musculoskeletal pain[2]:
Other types of pain are also described here
- Referred Pain
- Hyperalgesia
- Allodynia
Nociceptive Pain[edit | edit source]
Nociceptive pain can be thought of as pain associated with tissue injury or damage or even potential damage: nociceptors are sensory endings on nerves that can be excited or sensitized and signal potential tissue damage. Examples of nociceptive pain include jamming your finger in a car door, spraining your ankle or touching the hot plate on the stove.
Nociceptive Inflammatory Pain[edit | edit source]
Nociceptive inflammatory pain is associated with tissue damage an inflammatory response occurs. Inflammation is a coordinated body system response that is designed to help heal the tissue damage. The inflammatory response is well coordinated and involves blood-borne chemicals, immune system chemicals and some chemicals released from specialised nerve fibres. These chemicals talk to each other to help coordinate tissue repair.
Examples of nociceptive pain include jamming fingers in car door, a sprained ankle, non specific low back pain or neck pain, fractures. There may be signs of tissue injury such as swelling, redness and later purple or yellowing of the skin, a limb that looks distorted, increased sensitivity to touch and movement. Such signs are part of tissue healing.
Neuropathic Pain[edit | edit source]
Neuropathic pain is pain associated with injury or disease of nerve tissue. People often get this type of pain when they have shingles, sciatica, cervical or lumbar radiculopathy, trigeminal neuralgia, or diabetic neuropathy.
Neuropathic pain is often described as burning, shooting, stabbing, prickling, electric shock-like pain, with hypersensitivity to touch, movement, hot and cold and pressure. Neuropathic pain may cause even a very light touch or gentle movement to be very painful.
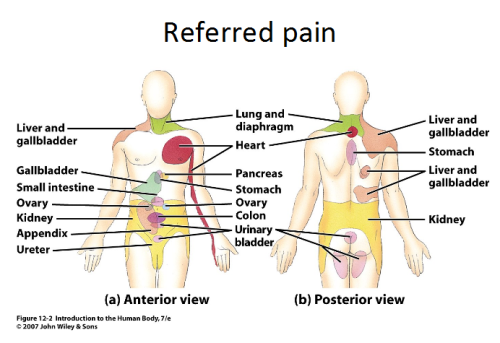
Referred Pain[edit | edit source]
Referred pain is pain perceived at a location other than the site of the painful stimulus. It usually originates in one of the visceral organs but is felt in the skin or sometimes in another area deep inside the body. Its mechanism is likely due to the fact that pain signals from the viscera travel along the same neural pathways used by pain signals from the skin. The result is the perception of pain originating in the skin rather than in a deep-seated visceral organ or neural structure.
Visceral nociceptors project into the spinal cord via small diameter myelinated and unmyelinated fibres from the autonomic nervous system. They go on to synapse close to the point of embryonic origin in the spine. When an organ develops pain, it can therefore be perceived as being at a different point in the body, on the surface, rather than in the organ itself.[3]
Mechanism
Hyperalgesia[edit | edit source]
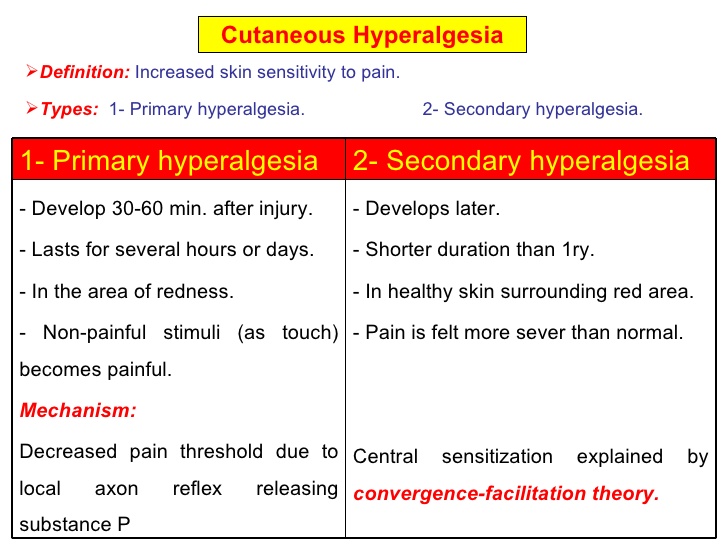
Hyperalgesia is defined as "An increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves".[4]
It is divided into 2 types, primary and secondary.
- Primary hyperalgesia - pain and sensitivity in the damaged tissues.
- Secondary hyperalgesia - pain and sensitivity that occurs in area around the damaged tissues.
Substance P appears to have a significant role in the sensitiation of nociceptors, which may explain the heightened feeling of pain in injured tissue (primary hyperalgesia). Although this doesn't account for the perception of non-painful stimuli as painful. Secondary hyperalgesia is most likely accounted for by changes in the dorsal horn which affect the processing of sensory information. [3] It is likely that normally silent nociceptors are recruited, and sprouting of large diameter sensory afferent occurs projecting into the dorsal horn laminae.
Allodynia[edit | edit source]
Central pain sensitization (increased response of neurons) following painful, often repetitive, stimulation.
Allodynia can lead to the triggering of a pain response from stimuli which do not normally provoke pain.[5]
Types of allodynia:
- Mechanical allodynia (also known as tactile allodynia)
- Static mechanical allodynia – pain in response to light touch/pressure[6]
- Dynamic mechanical allodynia – pain in response to stroking lightly[7]
- Thermal (hot or cold) allodynia – pain from normally mild skin temperatures in the affected area
- Movement allodynia - pain triggered by normal movement of joints or muscles.
Inflammatory Pain[edit | edit source]
One of the cardinal features of inflammatory states is that normally innocuous stimuli produce pain[8] Please follow the link to this article for an overview of Inflammatory pain
Further Watching[edit | edit source]
Below is a 45 minuted video on Pain Mechanisms
References[edit | edit source]
- ↑ Visser EJ, Davies S. What is pain? II: Pain expression and behaviour, evolutionary concepts, models and philosophies. Australasian Anaesthesia. 2009(2009):35. Available from:https://www.notredame.edu.au/__data/assets/pdf_file/0013/3046/What-is-pain-part-II-philosophy-behaviours-ANZCA-Blue-Book.pdf (last accessed 20.5.2020)
- ↑ Painhealth Pain Types https://painhealth.csse.uwa.edu.au/pain-module/pain-types/ (last accessed 20.5.2020)
- ↑ 3.0 3.1 Roger, Barker, Barasi, Neal. Neuroscience at a glance.1999 Blackwell science.
- ↑ Hart BL (1988). "Biological basis of the behavior of sick animals". Neurosci Biobehav Rev 12 (2): 123–37.
- ↑ Merskey & Bogduk (Eds.) Classification of Chronic Pain. Seattle: IASP Task Force on Taxonomy, 1994
- ↑ Attal N, Brasseur L, Chauvin M, Bouhassira D (1999). "Effects of single and repeated applications of a eutectic mixture of local anaesthetics (EMLA) cream on spontaneous and evoked pain in post-herpetic neuralgia". Pain 81 (1–2): 203–9
- ↑ LoPinto C, Young WB, Ashkenazi A (2006). "Comparison of dynamic (brush) and static (pressure) mechanical allodynia in migraine". Cephalalgia 26 (7): 852–6.
- ↑ B. L. Kidd1 and L. A. Urban2. Mechanisms of inflammatory pain. Oxford JournalsMedicine & Health BJA Volume 87, Issue 1Pp. 3-11