Oxford Shoulder Score
Objective[edit | edit source]
A patient-reported measure (questionnaire) of shoulder pain and function domains combined in one composite scale. Devised in 1996 (Dawson, Fitzpatrick, & Carr, 1996) and for assessing outcomes of shoulder surgery for degenerative conditions (excluding conditions of shoulder instability, for which the Oxford Shoulder Instability Score (Dawson, Fitzpatrick, & Carr, 1999) was developed)[1].
Intended Population[edit | edit source]
The OSS was designed to assess the outcome of all shoulder surgeries with the exception of instability surgery.
Method of Use[edit | edit source]
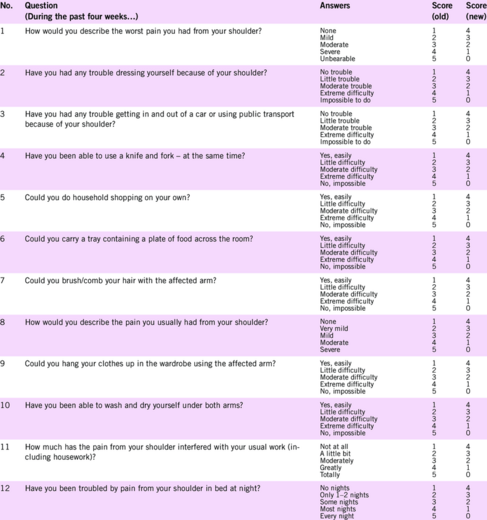
It contains 12 items, each with 5 potential answers. A mark between 1 (best/fewest symptoms) and 5 (worst/most severe) is awarded to correspond to the patient's symptoms. The combined total gives a minimum score of 12 and a maximum of 60. A higher score implies a greater degree of disability.
In 2009 the scoring method for the OSS was modified so that each of the 12 items is scored from 4 (best/fewest symptoms) to 0 (worst/most severe) [2].
Reference[edit | edit source]
The total score, therefore, ranges from 48 to 0, with a lower score indicating a greater degree of disability.
Reliability[edit | edit source]
Internal Consistency: Cronbach’s alpha was 0.89 at the preoperative assessment (n = 111) and 0.92 at the 6-month follow-up (n = 56). All items correlated with the total score at >0.4. Test-Retest Reliability: assessed on n = 68 with 24 h between assessments. The estimated mean (−0.12) of score differences was not significantly different from 0. The coefficient of reliability was calculated as 6.8 using the Bland and Altman method and 95 % of score differences fell between 0 and ±6.8. Overall, 83 % of score differences lay between 0 and ±4 points. The intraclass correlation was subsequently calculated as 0.83 [1].
Validity[edit | edit source]
Evidence of convergent validity included large correlations (pre-op: r = 0.74 p < 0.01, post-op: r = 0.75 p < 0.01) between the OSS and the clinically assessed Constant Shoulder score (Constant & Murley, 1987). There was also moderate to high correlations (r > 0.49 to r = 0.86, p < 0.01) between the preoperative OSS questionnaire and relevant domains of the Health Assessment Questionnaire (HAQ) and the SF-36 (particularly physical function and pain domains)[1].
Responsiveness[edit | edit source]
Responsiveness/Sensitivity to Change: Patients reported substantial improvement at the 6-month follow-up assessment. The effect size (1.2) was slightly larger for the OSS questionnaire than for any of the individual subscales of the HAQ or SF-36 questionnaires. The change scores for the OSS were significantly greater (p < 0.001) for patients who reported the most improvement in their condition using transition items.[1]
Links[edit | edit source]
Oxford Shoulder Score http://www.orthopaedicscore.com/scorepages/oxford_shoulder_score.html
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement. The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.
- ↑ Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement. The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.