Overview of the ICF and Clinical Practice
Original Editor - Ewa Jaraczewska based on the course by Patricia Saleeby
Top Contributors - Ewa Jaraczewska and Jess Bell
Introduction[edit | edit source]
The International Classification of Functioning, Disability and Health (ICF) is a framework to describe the functioning and disability of an individual in relation to a health condition. It "offers a conceptualization of functioning and disability that can underpin assessment and documentation in rehabilitation [...] Experience with the ICF reminds practitioners to consider all the domains of participation, the effect of the environment on participation and the importance of involving clients/patients in assessment and service planning."[1]
Relevant Vocabulary[edit | edit source]
Clinical Practice: a type of practice involving activities with clients or on behalf of clients.[2]
Clinical Practice Activities: patient consultation and clinical investigation accomplished through a review of the clinical records, observation, examination, and communication with the client or another involved person (e.g. a parent or guardian).[2]
Clinical Professionals: a wide range of rehabilitation specialists whose role is to assess and improve functioning through clinical practice.[2]
ICF: a tool that helps to capture an individual's "lived experience."[2]
ICF Qualifiers: The ICF rating system which assists with the documentation of the severity of functioning problems.[3]
Capacity: The qualifiers for the Activities and Participation domain describe an individual's ability to complete a task or action in a standard environment.[2]
Performance: The qualifiers for the Activities and Participation domain describe what an individual does in their current environment.[2]
ICF Checklist: The World Health Organization (WHO) developed an assessment instrument known as the Clinician Form for the ICF.[2] The Checklist is available here.
ICD Codes: International Statistical Classification of Diseases and Related Health Problems, which allows "the systematic recording, analysis, interpretation and comparison of mortality and morbidity data collected in different countries or regions and at different times."[4]
Personal Factors: a component of contextual factors in the ICF that includes background information about the life and lifestyle of an individual.[5] Personal factors are not classified in the ICF due to the significant social and cultural variability associated with them.[2]
Environmental Factors: a component of the contextual factors in the ICF that involves the physical, social, and attitudinal environment in which people live.[6]
WHODAS: The World Health Organization Disability Assessment, which is a generic assessment instrument for health and disability.[2] The WHODAS is available here.
Social Determinants of Health: "non-medical factors that influence health outcomes."[7]
Clinical Professions[edit | edit source]
Clinical professions include allied health, nursing and medical professions. Allied health professions can be grouped into three categories: therapy, diagnostic and technical, and scientific.[8] Clinical professions include, but are not limited to:[2]
- Rehabilitation specialists
- Physical or physiotherapists
- Occupational therapists
- Social workers
- Psychologists
- Physicians
- Nurses
- Speech-language pathologists / therapists
- Audiologists
- Recreation therapists
- Vocational specialists
- Other clinical providers.
Clinical professionals practise in various settings and form interdisciplinary teams that communicate using the same terminology, standardised classifications and assessments to address and improve a person's functioning. The following are examples of practice settings where clinical professionals work:
Clinical environments:
- Hospitals
- Clinics
- Clinical offices
- Outpatient facilities
- Assisted living settings
- Retirement homes
Everyday environments:
- School system
- Patients' homes
- Communities
- Work, and vocational settings[2]
The International Classification of Functioning, Disability and Health[edit | edit source]
The International Classification of Functioning, Disability and Health (ICF) describes the functioning of an individual and the factors that relate to function. These interactive factors consist of the following components: body functions and structures, activities and participation, environmental factors, and personal factors.[9] Data obtained from the ICF provides information on an individual's life situation and helps to determine the best treatment and intervention for that person.[2] It is essential to recognise that the ICF is not an assessment tool. However, Kohler et al.[10] suggest that specific ICF categories can be used as components of rehabilitation outcome measures. The primary benefit of the ICF in clinical practice is to provide a universal language to describe an individual's function and their lived experience of health.[11]
ICF Qualifiers[edit | edit source]
ICF Qualifiers quantify "the extent of a problem experienced by a person in a specific ICF category".[12]
Qualifiers for Body Functions and Structures: this 7-point scale indicates the presence and magnitude (or extent) of an impairment. The following qualifiers are used: 0=no problem; 1=mild problem; 2=moderate problem; 3=severe problem; 4=complete problem; 8=not specified; and 9=not applicable.[3] For Body Structures, the second qualifier indicates the nature of the structural change, and the third qualifier indicates the location of the impairment.[12] The following scale is used to define the nature of the change: 0=no change; 1=total absence;2=partial absence;3=additional part; 4=aberrant dimensions; 5=discontinuity; 6=deviating position;7=qualitative changes in structure, including accumulaton of fluid; 8= not specified; 9=not applicable.
Qualifiers for Activities and Participations: this negative and positive scale indicates the presence of a barrier or facilitator along with the magnitude of an associated environmental factor.[2] Qualifiers for barriers include 0=no barrier; 1=mild barrier; 2=moderate barrier; 3=severe barrier; 4=complete barrier; 8=barrier, not specified; 9=not applicable. Facilitators are described as follows: +0=no facilitator; +1=mild facilitator; +2=moderate facilitator; +3=substantial facilitator; +4=complete facilitator; +8=facilitator, not specified.[12]
Prodinger et al.[13] provide evidence for the use of the categories and associated qualifiers to measure functioning.[13] However, in their pilot study, Kohler and colleagues,[10] indicated fair to poor interrater and intrarater reliability when using the qualifiers as published in the ICF. This highlighted a need for more explicit definitions to some of the qualifiers.[10]
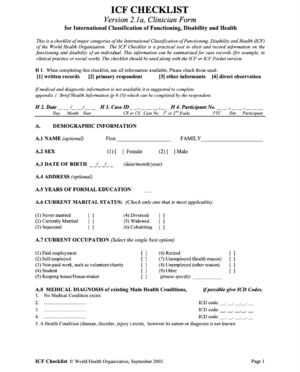
ICF Checklist[edit | edit source]
The WHO-developed ICF Checklist is a practical translation of the ICF for clinical practice. Known as the Clinician Form for the ICF,[2] it records information about the functioning and disability of an individual.[2] The ICF checklist is not a stand alone tool - it should be used alongside the ICF.[14]
The ICF checklist consists of ICF categories. These categories were chosen by experts to list the most commonly used domains, including body functions and structures, activities and participation, and environmental factors. Diagnostic information is also a component of the ICF checklist, which focuses the user's attention on the relationship between a health condition and the associated functioning problems.[15]
Sections of the Checklist[edit | edit source]
- The individual’s demographic information: includes factors that may help you better understand the life situation of a client or patient.[2]
- Medical diagnosis: provides information on medical conditions and the ICD codes. The Brief Health Information section supports this section.[2]
- The ICF domains: contain definitions and information about the qualifiers for each of the domains.[2]
- Part 4 provides space to document other contextual information, including Personal Factors which may impact the functioning of the client or patient.[2]
- The second appendix offers general questions to help determine capacity versus performance in the areas of mobility, self-care, domestic life, interpersonal interactions, major life areas, and community, social and civic life.[2]
World Health Organization Disability Assessment (WHODAS)[edit | edit source]
The World Health Organization Disability Assessment measures health needs and outcomes of interventions across various disease areas and health care settings. Its newest version, WHODAS 2.0, is a "general measure of functioning and disability that reflects major life domains as classified in the ICF".[15] It is a tool that produces standardised disability levels and profiles for all diseases, including mental, neurological and addictive disorders and is applicable across cultures in all adult populations.[2]
Methods of Assessment[edit | edit source]
WHODAS 2.0 assesses the level of functioning in six domains of life:[15]
- Cognition – understanding and communicating
- Mobility – moving and getting around
- Self-care – attending to one’s hygiene, dressing, eating and staying alone
- Getting along – interacting with other people
- Life activities – domestic responsibilities, leisure, work and school
- Participation – joining in community activities, participating in society
There are two versions of WHODAS 2.0 which differ in length and intended mode of administration. There is a full version with 36 questions and a short version with 12 questions. The 36-item version provides more details and takes about 20 minutes to complete. The 12-item version is helpful for brief assessments of overall functioning and takes about 5 minutes to complete. Questions can be asked during an interview in person or over the phone with the person themselves or with a family member, friend or caregiver. They can also be self-answered using a paper-and-pencil method.[15][2]
Scoring options[edit | edit source]
Option 1:[2]
- 5-point scoring system: 1=none, 2=mild, 3=moderate, 4=severe, 5=extreme
- Scores from each of the items are added up without recoding or collapsing the responses
- No weighting of individual items
- The sum of the items' scores across all domains describes the degree of functional limitations.
Option 2:[2]
- Item-response-theory (IRT)–based scoring
- 5-points scoring system: 1=none, 2=mild, 3=moderate, 4=severe, 5=extreme
- The items and the levels of severity are weighted by a computer to determine the summary score
- Step 1—Summing of recoded item scores within each domain
- Step 2—Summing of all six domain scores
- Step 3—Converting the summary score into a metric ranging from 0 to 100 (where 0 = no disability; 100 = full disability)
You can find more information about WHODAS 2.0 on the WHO website.
Social Determinants of Health[edit | edit source]
Social Determinants of Health (SDOH) include factors other than medical care that social policies can influence. They consider "the conditions in which people are born, grow, live, work and age" and "the fundamental drivers of these conditions."[16] According to McGinnis et al.,[17] medical care is responsible for only 10%–15% of preventable mortality in the U.S.[17] Studies completed by Mackenbach and colleagues point to the overwhelming impact of social factors on an individual's health.[18]
The ICF system recognises SDOH primarily as environmental factors (e.g. food insecurity, housing conditions). The ICF framework also includes personal factors such as age and education.[2]
Please watch this short introduction to Social Determinants of Health:
Resources[edit | edit source]
- Closing the gap in a generation: health equity through action on the social determinants of health - Final report of the commission on social determinants of health
- ICF Checklist
- WHO Disability Assessment Schedule 2.0 (WHODAS 2.0)
References[edit | edit source]
- ↑ Madden RH, Bundy A. The ICF has made a difference to functioning and disability measurement and statistics. Disabil Rehabil. 2019 Jun;41(12):1450-1462.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 Saleeby P. ICF and clinical practice course. Physiopedia 2022.
- ↑ 3.0 3.1 Senju Y, Mukaino M, Prodinger B, Selb M, Okouchi Y, Mizutani K, Suzuki M, Yamada S, Izumi SI, Sonoda S, Otaka Y. Development of a clinical tool for rating the body function categories of the ICF generic-30/rehabilitation set in Japanese rehabilitation practice and examination of its interrater reliability. BMC Medical Research Methodology. 2021 Dec;21(1):1-4.
- ↑ International Statistical Classification of Diseases and Related Health Problems (ICD). Available from https://www.who.int/standards/classifications/classification-of-diseases [last access 15.08.2022].
- ↑ Karhula M, Saukkonen S, Xiong E, Kinnunen A, Heiskanen T, Anttila H. ICF Personal Factors Strengthen Commitment to Person-Centered Rehabilitation – A Scoping Review. Frontiers in Rehabilitation Sciences, 2021; 2.
- ↑ Schneidert M, Hurst R, Miller J, Ustün B. The role of environment in the International Classification of Functioning, Disability and Health (ICF). Disabil Rehabil. 2003 Jun 3-17;25(11-12):588-95.
- ↑ Social determinants of health. Available from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 [last access 15.08.2022].
- ↑ Snowdon DA, Sargent M, Williams CM, Maloney S, Caspers K, Taylor NF. Effective clinical supervision of allied health professionals: a mixed methods study. BMC health services research. 2020 Dec;20(1):1-1.
- ↑ González-Seguel F, Corner EJ, Merino-Osorio C. International classification of functioning, disability, and health domains of 60 physical functioning measurement instruments used during the adult intensive care unit stay: a scoping review. Physical therapy. 2019 May 1;99(5):627-40.
- ↑ 10.0 10.1 10.2 Kohler F, Connolly C, Sakaria A, Stendara K, Buhagiar M, Mojaddidi M. Can the ICF be used as a rehabilitation outcome measure? A study looking at the inter- and intra-rater reliability of ICF categories derived from an ADL assessment tool. J Rehabil Med. 2013 Sep;45(9):881-7.
- ↑ van der Veen S, Evans N, Huisman M, Welch Saleeby P, Widdershoven G. Toward a paradigm shift in healthcare: using the International Classification of Functioning, Disability and Health (ICF) and the capability approach (CA) jointly in theory and practice. Disabil Rehabil. 2022 Jun 22:1-8.
- ↑ 12.0 12.1 12.2 ICF Case studies. Available from https://www.icf-casestudies.org/introduction/introduction-to-the-icf/the-content-of-the-classification [last access 15.08.2022].
- ↑ 13.0 13.1 Prodinger B, Stucki G, Coenen M, Tennant A. The measurement of functioning using the International Classification of Functioning, Disability and Health: comparing qualifier ratings with existing health status instruments. Disabil Rehabil. 2019 Mar;41(5):541-548.
- ↑ ICF Checklist. Available from https://www.who.int/publications/m/item/icf-checklist [last access 15.08.2022].
- ↑ 15.0 15.1 15.2 15.3 Kostanjsek N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health. 2011 May 31;11 Suppl 4(Suppl 4):S3.
- ↑ World Health Organization, Commission on Social Determinants of Health . Closing the gap in a generation: Health equity through action on the social determinants of health. CSDH final report. Geneva: WHO; 2008. Available from https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 [last access 16.08.2022]
- ↑ 17.0 17.1 McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002 Mar-Apr;21(2):78-93.
- ↑ Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014 Jan-Feb;129 Suppl 2(Suppl 2):19-31.
- ↑ Let's Learn Public Health. Social Determinants of Health - an introduction.2017. Available from: https://www.youtube.com/watch?v=8PH4JYfF4Ns [last accessed 16/08/2022]