Overview of Spinal Cord Injuries
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, [[[Special:Contact|please get in touch]]]!
Original Editor - Kudzanayi Ronald Muzenda
Top Contributors - Naomi O'Reilly, Kudzanayi Ronald Muzenda, Kim Jackson, Admin, Tarina van der Stockt, Rucha Gadgil, Jess Bell, Lucinda hampton and Ewa Jaraczewska
What is a Spinal Cord Injury[edit | edit source]
Spinal Cord Injury (SCI) is a sudden onset disruption to the neuronal tisue within the spinal canal resulting in spinal cord damage as a result trauma, disease or degeneration. [1][2] It can present as either an upper motor neurone lesion or lower motor neurone lesion with varying loss of motor, sensory and autonomic function, either temporary or permanent depending on the level and type of injury to the Spinal Cord.[2][3] Classification of Spinal Cord Injury is conducted based on the degree of sparing of movement and sensation below the level of the Injury using the ASIA Impairment Scale. [4]
Paraplegia refers to impairment or loss of motor, sensory or autonomic function in areas of the body served by the thoracic, lumbar or sacral segments of the spinal cord. Depending on the level of the injury trunk, pelvic organs and lower limbs may be involved with upper limb function preserved.[1]
Tetraplegia, sometimes referred to as quadriplegia, refers to impairment or loss of motor, sensory or autonomic function in areas of the body served by the cervical segments of the spinal cord. This results in impairment in upper and lower limbs, trunk and pelvic organs with respiratory function impaired in those with high cervical injuries.[1]Clinically Relevant Anatomy[edit | edit source]
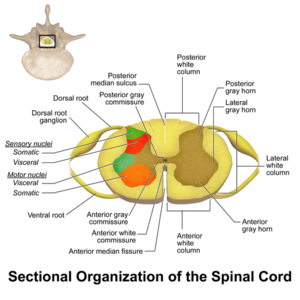
Th spinal column is comprised of 33 Vertebra; Cervical (7 Vertebrae), Thoracic (12 Vertebrae), Lumbar (5 Vertebrae), Sacral (5 Vertebrae) and Coccygeal (4 Vertebrae), which provide support and protection for the spinal cord. The spinal cord is the major conduit between the peripheral nerves and the brain, and transmits motor information from the brain to the muscles, tissues and organs, and sensory information from these areas back to the brain. [5][6]
The nervous system is divided into the central nervous system and (brain and spinal cord) and the peripheral nervous system (nerves that enter and exit the spinal cord. Information to and from the muscles, glands, organs and sensory receptors are carried through the peripheral nervous system, which is divided into the autonomic nervous system carrying information to and from the organs, and the somatic nervous system carrying information to and from the muscles and the external environment. [5] The autonomic nervous system consists of the parasympathetic nervous system that governs resting function and the sympathetic nervous system that governs excitatory functions. The spinal cord and peripheral nerves provide all impulses to control muscle contraction, cardiac rhythm, pain and other bodily functions so therefore any lesion to the spinal cord prevents of reduces transmission of this information to and from the brain to the peripheries, affecting movement sensation and visceral function. [6]
Epidemiology[edit | edit source]
A recent systematic review found the prevalence of spinal cord injury to be dependent on the region the studies were conducted in, ranging from the highest prevalence of 906 per million in the USA and the lowest prevalence of 250 per million in Rhone-Alpes, France. Annual incidence rates also varied significantly between region, ranging from 49.1 per million in New Zealand to just 10.0 per million in Fiji. [9] A further review found similar results with prevalence ranging from 1298 per million to 50 per million and incidence ranging from 246 per million to 3.3 per million.[10] These results indicate that the incidence, prevalence and causation of Spinal Cord Injury can differ significantly between developing and developed countries suggesting the need for management and preventative strategies that are tailored towards regional trends. [9]
Etiology[edit | edit source]
Spinal Cord injury can occur as a result of traumatic causes and non-traumatic causes e.g. degeneration, disease Strong inconsistencies in data were noted when analysed between countries but the most frequent causes of Spinal Cord Injury reported are, in order; [10]
- Motor Vehicle Accidents
- Falls
- Sport Injuries
- Violence
- Self-harm
- Work-related Accidents.
Similarly most studies available show a high male-to-female ratio with peak incidence occurring in those younger than 30 years old. Traffic accidents were typically the most common cause of SCI, followed by falls in the elderly population. Data from the National Spinal Cord Injury Statistical Center (USA) 2010 - 2014 provided the following statistics for etiology (illustration). Other interesting statistics from this report include:
- Males account for 80% of new cases
- Average age at injury has gone up from 29 years old (1970) to 42 years old currently.
- Only about 12% of patients are employed 1 year after trauma, rising to 34.4% 20 years post injury
- Life expectancy decreases for all individuals with Spinal Cord Injury, compared to those without a spinal cord injury.
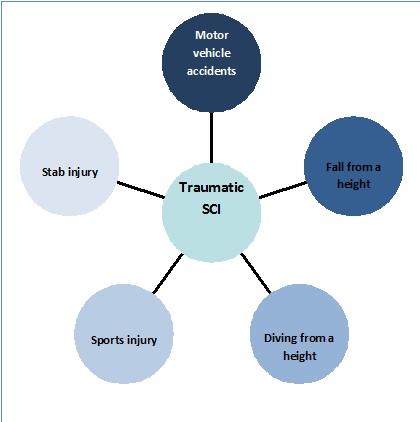
Traumatic Causes of Spinal Cord Injuries [12][edit | edit source]
The diagram below shows the traumatic causes of of SCI
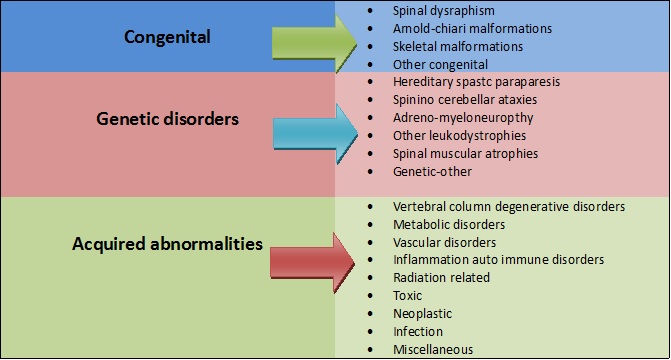
Non-traumatic causes of Spinal cord injuries[13][edit | edit source]
The table below shows a summary of non- traumatic causes of SCI injuries
Clinical Presentation[edit | edit source]
Injuries to the spinal cord are complex, and each individuals injury is unique in terms of the functions affected and therefore the clinical presentation. Classification of the spinal cord injury is conducted by means of a neurologic assessment including motor, sensory and autonomic evaluation to determine the degree of sparing of motor, sensory and autonomic function below the level of the Injury using the American Spinal Injury Association (ASIA) Impairment Scale.[4][14]
Paraplegia refers to impairment or loss of motor, sensory or autonomic function in areas of the body served by the thoracic, lumbar or sacral segments of the spinal cord. Depending on the level of the injury trunk, pelvic organs and lower limbs may be involved with upper limb function preserved.[1]
Tetraplegia, sometimes referred to as quadriplegia, refers to impairment or loss of motor, sensory or autonomic function in areas of the body served by the cervical segments of the spinal cord. This results in impairment in upper and lower limbs, trunk and pelvic organs with respiratory function impaired in those with high cervical injuries.[1]
Types[edit | edit source]
Complete[edit | edit source]
Incomplete[edit | edit source]
Brown Sequard Syndrome Anterior Cord Syndrome
Differential Diagnosis[edit | edit source]
- Aortic Artery Dissection
- Epidural and Subdural Infections
- Spinal Cord Infections
- Spinal Abscess
- Syphilis (Tertiary)
- Vertebral Fracture
- Transverse Myelitis
- Acute Intervertebral Disk Herniation
- Spinal Abscess
Diagnostic Procedures[edit | edit source]
Imaging technology is an important part of the diagnostic process of acute or chronic spinal cord injuries. Spinal cord injuries can be detected using different types of imaging which depends on the type of underlying pathology. MRI has become the golden standard for imaging neurological tissues such as the spinal cord, ligaments, discs and other soft tissues. Only MRI sequences of sagittal T2 were found to be useful for prognosticative purposes. [15] Spinal fractures and bony lesions are better characterized by computed tomography (CT) and vascular injuries van be detected by using an MR angiography or by a CT scan.[16]
Medical Management[edit | edit source]
Conservative Management[edit | edit source]
Surgical Management[edit | edit source]
Physiotherapy Management[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Stack E, Stokes M, editors. Physical Management for Neurological Conditions. Elsevier Churchill Livingstone; 2012.
- ↑ 2.0 2.1 Harvey L. Management of Spinal Cord Injuries: A Guide for Physiotherapists. Elsevier Health Sciences; 2008 Jan 10.
- ↑ Tymianski, D., Sarro, A. Green, T. (2012). Navigating Neuroscience Nursing: A Canadian Perspective. 1st Ed. Pappin Communications, Pembroke, Ontario
- ↑ 4.0 4.1 Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535-546
- ↑ 5.0 5.1 Moore KL, Agur AM, Dalley AF. Essential Clinical Anatomy. Philadelphia: Lippincott Williams & Wilkins; 2002 Mar.
- ↑ 6.0 6.1 Francisco de Assis Aquino Gondim et al., Topographic and Functional Anatomy of the Spinal Cord, Medshape, 2015
- ↑ Designed by Freepik at http://www.freepik.com
- ↑ Spinal Cord. Blausen Medical. Retrieved on 26 January 2016.
- ↑ 9.0 9.1 Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global Prevalence and Incidence of Traumatic Spinal Cord Injury. Clinical Epidemiology. 2014;6:309.
- ↑ 10.0 10.1 Furlan, J.C. et al. “Global incidence and prevalence of traumatic spinal cord injury.” Can J Neurol Sci. 2013 Jul;40(4):456-64
- ↑ Dominic Power. Spinal Cord Injury 1: Epidemiology and Classification of SCI. Available from: https://youtu.be/8lRM-emvn2Y[last accessed 25/10/18]
- ↑ Ackery A, Tator C, Krassioukov A. A global perspective on spinal cord injury epidemiology. J Neurotrauma 2004; 21: 1355-1370
- ↑ Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T, Wing P. International Spinal Cord Injury Data Sets. Spinal Cord. 2006 Sep;44(9):530-4.).
- ↑ J.W. McDonald et al. Spinal-Cord Injury. Lancet 2002 Fed2;359 (9304):417-25
- ↑ Anthony B. et al., The Role of Magnetic Resonance Imaging in the Management of Acute Spi-nal Cord Injury, J Neurotrauma. 2011 Aug; 28(8): 1401–1411
- ↑ Andrew L G. et al., Advances in Imaging of Vertebral and Spinal Cord Injury, J Spinal Cord Med. 2010 Apr; 33(2): 105–116