Other primary headaches
Introduction[edit | edit source]
According to the World Health Organization it is estimated that the prevalence of current headache disorders among adults, that is it has been symptomatic at least once within the last year, is approximately 50% worldwide. It was noted that half to three quarters of adults in the age range of 18–65 years globally have had a headache within the last year[1]. Headaches may have a known cause or be idiopathic. Headaches are usually associated with a specific cause. Examples of such causal factors are "specific foods, stress, muscle tension, hormonal fluctuations, nerve compression or cervical spine or temporomandibular joint dysfunction [2]. Frequent headaches which are idiopathic are noteworthy. This is due to the fact that headaches may be as a result of a serious medical condition and for this reason they ought to be assessed carefully[2]. Primary headaches are headaches which are due to a headache condition itself as opposed to a secondary headache which is as a result of another condition which the individual has, Part one of the International Classification of Headache Disorders speaks of primary headaches. The primary headaches are migraine, tension-type headache, cluster headache and other trigeminal autonomic cephalgias and what are categorized as other primary headaches.
Description[edit | edit source]
Headaches classified as other primary headaches are clinically heterogeneous. According to the (ICHD-III) the pathogenesis of other primary headaches is still poorly understood. It is noted that treatment of these disorders is made on the basis of anecdotal reports or uncontrolled trials[3].
Headaches classified as other primary headaches
Adapted from The International Classification of Headache Disorders, 3rd edition[3]
4.1 Primary cough headache
4.1.1 Probable primary cough headache
4.2 Primary exercise headache
4.2.1 Probable primary exercise headache
4.3 Primary headache associated with sexual activity
4.3.1 Probable primary headache associated with sexual activity
4.4 Primary thunderclap headache
4.5 Cold-stimulus headache
4.5.1 Headache attributed to external application of a cold stimulus
4.5.2 Headache attributed to ingestion or inhalation of a cold stimulus
4.5.3 Probable cold-stimulus headache
4.5.3.1 Headache probably attributed to external application of a cold stimulus
4.5.3.2 Headache probably attributed to ingestion or inhalation of a cold stimulus
4.6 External-pressure headache
4.6.1 External-compression headache
4.6.2 External-traction headache
4.6.3 Probable external-pressure headache
4.6.3.1 Probable external-compression headache
4.6.3.2 Probable external-traction headache
4.7 Primary stabbing headache
4.7.1 Probable primary stabbing headache
4.8 Nummular headache
4.8.1 Probable nummular headache
4.9 Hypnic headache
4.9.1 Probable hypnic headache
4.10 New daily persistent headache (NDPH)
4.10.1 Probable new daily persistent headache
Assessment[edit | edit source]
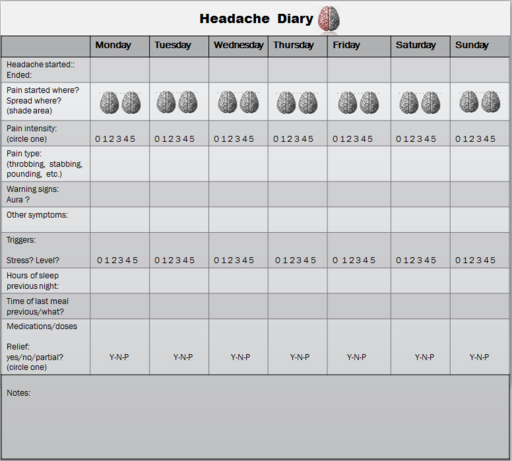
When a client with a headache presents to a physical therapist, a thorough assessment should be undertaken. It is noted that in the clinical setting the measurement of a headache is usually done via retrospective report from the patient[4]. A headache diary may be of use however it is usually recommended for the purpose of data collection in clinical trials[5].
A thorough history ought to be taken. It entails finding out if there is a family history of similar headaches. Making note of any stressors the client may have, Information should be gathered in regard to any diseases or conditions the client currently has or had in the past. Past traumatic injuries such as a hit to the head or face are also of interest. The site of the headache is of course important and needs to be made note of. The therapist also needs to acquire information on onset, frequency, intensity, duration and pattern of the headache. In regard to other primary headaches it is important to identify aggravating and relieving factors along with any associated symptoms. The therapist should assess for cardiovascular issues. This is done by assessing the blood pressure and pulse, The therapist may also auscultate for bruits in the temporal and carotid arteries. This gives the physical therapist important information in regard to the client having temporal arteritis or carotid stenosis[2].
Headache disorders that fall under other primary headaches will not usually be brought to the attention of the physical therapist, Often the individual who suffers such a headache may present to the emergency department and see a medical doctor. According to the (ICHD-III) the onset of some of these headaches can be acute, and affected patients are sometimes assessed in emergency departments[3]. If a primary contact therapist encounters a clients who suffers from other primary headache disorders they may need to refer them. According to Goodman, Heick and Lazaro (2017) "headaches that cannot be linked to a neuromuscular or musculoskeletal cause (e.g., dysfunction of the cervical spine, thoracic spine, or temporomandibular joints; muscle tension, poor posture, nerve impingement) may require further medical referral and evaluation"[2].
Of special note is the thunderclap headache. The thunderclap headache is often associated with serious vascular intracranial vascular disorders, especially a subarachnoid haemorrhage. It is therefore imperative that further tests/examination be done to exclude that diagnosis and other conditions such as [[ Hemorrhagic Stroke: Intracerebral Hemorrhage|intracerebral haemorrhage]][3], According to the ICHD-III "headaches with similar characteristics to several of the other primary headache disorders can be symptomatic of another disorder (i.e. secondary headaches); when they first present, they demand careful evaluation by imaging and/or other appropriate tests. Appropriate and full investigation (neuroimaging, in particular) is mandatory in these cases"[3].
Individual suffering from stabbing headache[6]
References[edit | edit source]
- ↑ World Health Organization. Headache disorders. World Health Organization; 2018.
- ↑ 2.0 2.1 2.2 2.3 Goodman CC, Heick J, Lazaro RT. Differential Diagnosis for Physical Therapists-E-Book. Elsevier Health Sciences; 2017 Apr 29.
- ↑ 3.0 3.1 3.2 3.3 3.4 Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd ed. Cephalalgia. 2018;38(1): 1-211.
- ↑ Niere K, Robinson P. Determination of manipulative physiotherapy treatment outcome in headache patients. Manual therapy. 1997 Nov 1;2(4):199-205.
- ↑ Selvaratnam P, Niere KR, Zuluaga MI, Oddy P. Headache, Orofacial Pain and Bruxism: Diagnosis and multidisciplinary approaches to management. (Content Advisors: Stephen Friedmann BDSc (Dental) ; Cathy Sloan MBBS Dip RANZCOG (Medical). Churchill Livingstone; 2009.
- ↑ Monique Lander. Stabbing Sharp Headache- Recorded Ice Pick Attack. Available from https://www.youtube.com/watch?v=qCw6G8vvXMw [last accessed 31/12/2018]