Opioids
An opioid refers to any substance from a group of analgesic agents derived from the ingredient opium. Opioids are a type of depressant, analgesic drug that slow down the messages being sent through the central nervous system between the body to the brain. Although used to treat pain, opioids can entice euphoric feelings and sedative effects which can be addictive which leads this drug group to be commonly abused.
Clinical Pharmacology[edit | edit source]
Four naturally occurring alkaloids can be isolated from the opium poppy seed (papaver somniferum). These plant-derived amines are morphine, codeine, papaverine and thebaine. These can be used to produce many varieties of semi-synthetic opioids useful in clinical medicine including diamorphine, dihydrocodeine, buprenorphine, nalbuphine, naloxone and oxycodone.
Opioids act on different receptors located on neuronal cell membranes. There are three major types of opioid receptor, m, d and k (mu, delta and kappa). All 3 receptors will produce analgesia when binded with an opioid substance. Activation of k receptors, as with dynorphin, does not produce as much physical dependence as activation of m receptors, as occurs with morphine. The opioid antagonist, naloxone, inhibits all of the opioid receptors which is why its used to treat opioid overdose.[1]
Benefits & Drawbacks of Opioids[edit | edit source]
Opioids can produce profound analgesia for patients with acute pain. Opioids are very effective at treating acute pain due to their ability to inhibit pain signal transmission at multiple stages in the pain pathway and their ability to enhance the inhibitory pain fibres.
There are many adverse effects associated with opioids. Kappa receptor stimulation is associated with side effects such as hallucinations, dysphoria, anxiety and restlessness. Delta and mu receptor stimulation is often dangerously associated with respiratory depression as the body is unable to regulate carbon dioxide levels in the body effectively. Other drawbacks associated with opioid use in general include sleep apnoea, hypothalamic-pituatory axis supression (hormonal changes with the potential for decreased libido, infertility & fluid retention), urinary retention, nausea & vomiting, physical dependence and addiction, opioid-induced hyperalgesia, dental pathology, constipation, increased mortality and tolerance.[2]
Considerations in Physiotherapy[edit | edit source]
Opioids are regularly administered for the treatment of pain; many patients that present to physical therapists may have already been prescribed them. Our role within any multidisciplinary management team treating a person who has pain is to ensure that we are monitoring the safe and clinically indicated use of opioids if required, identifying the potential for adverse effects and recognising these in a timely manner. The video clip below highlights the signs to look for re addiction to opiods
Opiod use is also linked to increased falls risk. A 2018 retrospective, observational, multicentre cohort study the findings were that recent opioid use is associated with a greater risk of falls in older adults and a greater likelihood of death in those with fall-related injuries.[4]
Opioids alone are not a solution for chronic pain as supported by an abundance of literature. [6][7][8]
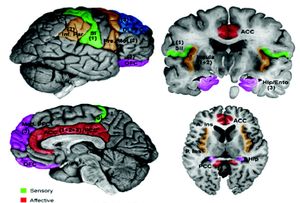
The image below shows the many areas involved in the brain with pain processing.
References[edit | edit source]
- ↑ Pathan, H., & Williams, J. (2012). Basic opioid pharmacology: an update. British journal of pain, 6(1), 11-6.
- ↑ Prescription Opioid Policy. A publication by The Royal Australian College of Physicians, Faculty of Pain Medicine ANZCA, The Royal Australian College of General Practitioners and The Royal Australian and New Zealand College of Psychiatrists.
- ↑ Bob and Brad. 9 signs someone you love is addicted to opiods. Available from: https://www.youtube.com/watch?v=NPPbkQbp5-0 (last accessed 9.4.2019)
- ↑ Daoust R, Paquet J, Moore L, Émond M, Gosselin S, Lavigne G, Choinière M, Boulanger A, Mac-Thiong JM, Chauny JM. Recent opioid use and fall-related injury among older patients with trauma. CMAJ. 2018 Apr 23;190(16):E500-6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5915247/ (last accessed 9.4.2019)
- ↑ Fox 47 news. Opiod use linked to increased risk of falls. Available from: https://www.youtube.com/watch?v=mYrQUj2yecs&app=desktop (last accessed 9.4.2019)
- ↑ Reinecke H, Weber C, Lange K, Simon M, Stein C, Sorgatz H. Analgesic efficacy of opioids in chronic pain: recent meta‐analyses. British journal of pharmacology. 2015 Jan;172(2):324-33.
- ↑ Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, Hirsch J. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017 Feb 1;20(2S):S3-92.
- ↑ Walsh K. General practice pain management: beyond opioids. InBSAVA Congress Proceedings 2016 2016 Apr 1 (pp. 354-354). BSAVA Library.