Opioid Use Disorder
Definition/Description[edit | edit source]
Opioid use disorder is a condition characterized by identifying the consequences associated with repeated opioid use, reflective compulsive use, and prolonged self-administration of opioid substances that includes non-prescription or prescription for a medical condition [1]. Prescribed opioid misuse can lead to addiction and occurs by taking the prescription in greater quantities other than specified, prolonged use past the intended prescribed time period, and use of prescription for other medical conditions that was not identify by the prescribing physician [1].
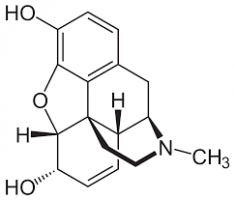
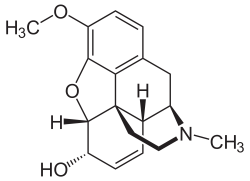
Opioids work by binding to specific receptors found throughout the body’s nervous and immune system [2]. The receptors are responsible for several functions that include pain, stress, temperature, respiration, endocrine activity, gastrointestinal activity, mood, and motivation. The main intended use is to reduce pain perception, but is associated with causing euphoria, drowsiness, mental confusion, nausea, constipation, and depress respiration (high doses) [2].
Commonly used opioids identified in the healthcare setting include:
- Codeine
- Fentanyl (patch)
- Hydrocodone (Hysingla ER, Zohydro ER)
- Hydrocodone/Acetaminophen (Lorcet, Lortabe, Norco, Vicodin)
- Hydromorphone (Dilaudid)
- Methadone (Dolophine)
- Morphine (Avinza, Kadian)
- Oxycodone (OxyContin, Roxicodone)
- Oxycodone
- Naloxone [1].
Prevalence[edit | edit source]
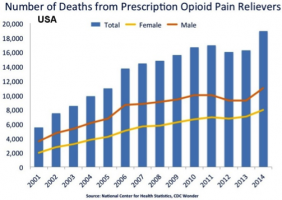
Drug overdose deaths are on the rise in the United States. The CDC reported that in 2014 overdose deaths increased 6.5% from the previous year [3]. The report also stated that since 2000, overdose death rate had risen 137% [3]. Of this rise in overdose deaths 61% was attributed to some type of opioid, with synthetic opioid being the leading of categories examined [3]. 78 people die per day due to opioid drug abuse [4].
Results of the 2014 National Survey on Drug Use and Health reported the impact of opioid use disorders among varying demographics. When examining age, the survey found that roughly 586,000 Americans age 12 or older had a heroin use disorder, with average first use age being 28 [5]. An estimated 1.9 million Americans age 12 or older reported a pain reliever use disorder [5]. Opioid use disorder is more common with males than females with the highest abuse rates among the Native American population [6].
A recent study performed by the Substance Abuse and Mental Health Services Administration found a trend in among non-medical pain reliever use and its initiation of heroin use [7]. More research is being done in this area to examine the relationship among these topics.
Clinical Presentation[edit | edit source]
Literature suggests that pain and addiction commonly co-exists. There are two theories on how this develops: (1) Individuals with pain are prescribed opioids as part of pain management and develop an opioid use disorder; (2) Individuals with a history of substance use disorder develop subsequent pain syndromes [8].
A detailed and pertinent history should be obtained not only by the individual, but from the family, caregiver, and/or friends to identify ingestion time, quantity and any co-ingestants of substances [8].
Symptoms associated with opioid use disorder include:
- Strong desire of opioids
- Inability to control or reduce use
- Continued use despite interference with major obligations or social functioning
- Use of larger amounts over time
- Development of tolerance
- Spending a great deal of time to obtain and use opioids
- Withdrawal symptoms that occur after stopping or reducing use
Ex: negative mood, nausea or vomiting, muscle aches, diarrhea, fever and insomnia [2]
Another issue associated with the presences of opioid use is the risk of toxicity which characteristically present with decreased level of consciousness. Signs and symptoms include:
- Altered mental status – confusion or delirium
- Respiratory depression – low respiratory rate
- Extreme sleepiness
- Nausea and vomiting
- Pupillary miosis (constriction)
Respiratory depression is the most significant sign and not all cases present with pupillary miosis [1].
Potential behavioral aspects can be indicated for individuals that should be screen for any type of substance use/abuse can include:
- Consistently missing appointments/ being extremely late
- Noncompliance with home exercise program or poor attention to self-care
- Shifting mood patterns (especially the presences of depression)
- Excessive daytime sleepiness or unusually excessive energy
- Deterioration of physical appearance and personal hygiene [2]
The older adult population may be harder to identify causative signs and symptoms due to mimicking typical aging characteristics including memory loss, cognitive problems, tremors, falls, weight loss, and muscle wasting [9].
Associated Co-morbidities[edit | edit source]
As research has shown, there is a high correlation between drug abuse and mental disorders. The National Institute on Drug Abuse has seen this association through national surveys dating back to the 1980s [10]. People that are “diagnosed with mood or anxiety disorders are twice as likely to suffer from a drug use disorder” and vice versa [10]. While different mental disorders can bring about opioid use disorder, the most common comorbidities associated with opioid use are anxiety and depression [1].
Another frequent comorbidity associated with opioid use disorder is chronic pain. Both opioid use disorder and chronic pain are driven by neurophysiological changes that can lead to altered or dysfunctional neural patterns [2]. Opioids are a common treatment option for those who have recently experienced trauma, surgery, and with chronic pain [2]. Opioid use disorder is increasing in chronic pain patients due to the risk of noncompliance with drug use [3]. The importance of screening an individual with chronic pain for substance use disorder is crucial; this way it can prevent any relapses with previously abused drugs like opioids or set up a strict plan for the individual using the drug [2].
Medications[edit | edit source]
Medication use in this population is indicated mostly for management of withdrawal symptoms and/or overdose. The purpose of the medication is to reduce the side effects of the opioid substance and/or the body’s dependence for the substance [4]. Treatment/management for opioid withdrawal is discussed in Medical Management. The medications that may be used as a form of treatment include [4]:
- Naloxone (opioid reversal agent) - Pure opioid antagonist – reverse opioid intoxication
- Methadone (opioid analgesic) - Reduces craving and withdrawal symptoms, Preferred agent for opioid agonist maintenance, Benefits – good treatment retention, psychosocial adjustment, and reduced criminal activity
- Buprenorphine (opioid analgesic) - Produces agonist/antagonist effects, Potent analgesic - can be administered once a day to block withdrawal symptom, Agonist effect is limited by ceiling effect (higher doses do not have additive effect), Abuse potential is low (compared to other opioids)
- Naltrexone (antidote) - Long-acting opioid antagonist, Blocks receptor sites, Indicated for prevention of relapse following detox
- Clonidine (alpha 2 adrenergic agonists) - May reduce norepinephrine release, Most effective in suppressing autonomic signs/symptoms (withdrawal), Less effective for subjective symptoms [4]
“Medication-assisted treatment with methadone, buprenorphine, or extended-release injectable naltrexone plays a critical role in the treatment of opioid use disorders. According to the latest survey of opioid treatment providers more than 300,000 people received some form of medication-assisted treatment for an opioid use disorder in 2011” [2].
Diagnostic Tests[edit | edit source]
The following are laboratory screening tools that can be used to test for opioid use disorder.
- Drug Abuse Screening Tool (DAST-10): assesses drug use in the past 12 months. 10-item yes-no questions; high scores indicate drug abuse. [5]
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5): assesses a 12 month period. Can indicate opioid use disorder if the patient fits in the criteria of 2 or more of the 11 criteria examined (ex. craving the substance). [6]
- CAGE-AID Questionnaire: 4 yes-no question tool about drug use. Answering yes to 1 or more questions is a positive test [6].
- RAFFT: Relaxed, Alone, Friends, Family, Trouble. 5 yes-no questionnaire targeting adolescent drug abuse. 2 or more yes answers results in a positive test [7].
- COMM: Current Opioid Misuse Measurement. 17 item, self-reported questionnaire. The higher the score, the increased likelihood of current opioid related deviant behavior [8].
The following are lab tests to test for opioid use disorder.
- Urine/blood toxicology tests: opioids can elicit positive test results 12-36 hours after ingestion [1].
- Screening for Hepatitis A, B, and C, and HIV: opioid abusers have an increased risk for acquiring these diseases from injection or sharing needles [1].
- Liver function tests: increase in ALT and AST can represent signs of acute liver damage; which could be a result from drug use [1].
Differential Diagnosis[edit | edit source]
In the healthcare profession, the importance to accurately identify the diagnosis is key for the effectiveness of treatment. There are several different diagnoses that present with similar signs and symptoms as opioid use disorder and must be considered with each individual. The list presented is not a limitation to possible diagnosis and proceeds as follows:
- Acute Pancreatitis
- Bacterial Gastroenteritis
- Barbiturate Toxicity
- Benzodiazepine Toxicity
- Chronic Pancreatitis
- Influenza
- Peptic Ulcer Disease
- Sepsis
- Antisocial Personality
- Panic Attack
- Pontine Infarct or hemorrhage
- Depressed Mood
- Viral Gastroenteritis [4]
Physical therapists work directly with individuals that experience pain and are prescribed opioid medications. Therefore, screening for the presence of substance abuse needs to be included in the physical therapy assessment. The Trauma Scale Questionnaire consists of four questions that are based on an established correlation between trauma and substance use (alcohol and other) for individuals 18 years old and older [9]. Answering “Yes” to two are more of the questions is an indication to discuss with the physician and/or generate a referral for further evaluation of substance use [9]. The questions included are:
- Have you had any fractures or dislocation to your bones or joints?
- Have you been injured in a road traffic accident?
- Have you injured your head?
- Have you been in a fight or assault? [9]
Etiology[edit | edit source]
There is not one single cause that will lead someone to develop an opioid use disorder. Although, there are several factors that can increase the risk for developing an addiction including both individual and environmental [1]. Genetic factors have been found to play an important role for predisposition tendencies that can respond to the environment [1].
Opioids are known to activate the mesolimbic reward system which signals the release of dopamine causing feelings of pleasure. Our brains ability to establish this conditioned association is responsible for the desire to repeatedly use the drug [9]. However, the body is highly specialized to make adaptations to the presence of the drug and will transition from compulsion of seeking pleasure to depending on the drug existence entirely. Therefore, the increased compulsion is related to an individual tolerance and dependence of the drug [9].
Systemic Involvement[edit | edit source]
Opioids reduce the perception of pain by attaching to proteins called opioid receptors that are located in the brain, spinal cord, gastrointestinal tract, and other organs [10]. Opioids also affect brain regions involved in reward so they produce a sense of well-being and pleasure [10].
Common side effects associated with taking opioid include the following [1]:
- Drowsiness
- Confusion
- Nausea and vomiting
- Constipation
- Sweating
- Pruritus
For those that inject opioids, the following complications can be seen [1]:
- Scarred/collapsed veins
- Abscesses
- Bacterial infections
- Blood borne viruses
- Thrombophlebitis
- Intravascular sepsis
- Endocarditis
- Accidental arterial injection
- Peripheral ischemia
For those with long-term opioid abuse, the following can be seen [1]:
- Gonadal suppression
- Reduced bone density
- Increase risk of osteoporotic fractures
- Decreased decision making ability
- Decreased ability to regulate behaviors
- Decreased management of stressful situations
- Addiction/dependence
Signs of opioid overdose include [1][10]:
- Respiratory depression
- Cardiovascular depression
- Loss of consciousness/coma
- Hypoxia
Signs of patients having withdraw symptoms include [1] [10]:
- Restlessness
- Muscle and bone pain
- Insomnia
- Vomiting
- Diarrhea
- Cold flashes
- Involuntary leg movements
- Agitation
- Flu-like symptoms
Medical Management[edit | edit source]
Current best evidence for the medical management of individuals with opioid use disorder begins treatment with detoxification followed by pharmaceutical maintenance therapy, psychotherapy, and treatment of acute pain in patients already on maintenance therapy [4].
Pharmacologic methods of detoxification typically include the use of methadone, burprenorphine, and alpha-2 agonists [4]. Other medications (listed in Medication section) are used for treating associated signs/symptoms from opioid intoxication, opioid overdose, and/or opioid withdrawal. Cognitive behavior psychotherapy works by focusing on the individual’s thoughts/behaviors and establishes techniques used to resist substance abuse and reduce factors related to drug use [4]. Treatment of acute pain in these individuals should include education on how to aggressively treat their pain with conventional opioid analgesics and reassurance of previous addiction history not hindering from adequate pain management [4].
Physical Therapy Management[edit | edit source]
Physical therapists are not qualified to manage opioid use disorders. Physical therapists should be able to recognize signs and symptoms of this disorder, but need to refer patients out for treatment. Physical therapists need to advocate for their patients to get them the treatment and help they deserve. Once treatment plans for the opioid use disorder are in place with a physician and patients began receiving medical treatment, if physical therapy treatment is needed, it would be utilized to help recover functional deficits. The physical therapy role mainly applies in opioid use disorders to get patients the appropriate care and begin advocating for nonopioid therapy through research in order to help decrease the prevalence of opioid abuse. The APTA has called to action for physical therapists and physical therapist assistances to focus on their role in pain management with the use of fewer or no drugs, such as opioids [1].
As the epidemic of opioid overuse has increased, the CDC has been working on guidelines to decrease risks of abuse and deaths in the United States. On March 15, 2016 the CDC released “Guideline for Prescribing Opioids for Chronic Pain” [2]. In these guidelines it promotes “nonpharmacological therapy and nonopioid therapy as preferred treatment for chronic pain” [2]. The CDC found that physical therapy and exercise therapy had a high-quality of evidence to reduce pain and improve function [2]. The CDC also states that the risks are much lower with nonopioid treatment plans, but in situations that opioids are prescribed they should always be combined with nonopioid therapies, such as physical therapy [2]. The movement is toward physical therapy affects in pain management to prevent opioid use disorder.
Case Reports[edit | edit source]
- Sullivan M, Edlund M, Fan M, DeVries A, Braden J, Martin B. Risks for Possible and Probable Opioid Misuse Among Recipients of Chronic Opioid Therapy in Commercial and Medicaid Insurance Plans: the TROUP Study. Pain. 2010 Aug; 150(2): 332–339. www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/
- Niesters M, Overdyk F, Smith T, Aarts L, Dahan A. Opiod-induced respiratory depression in paediatrics: a review of case reports. Br. J. Anaesth. (2013) 110 (2): 175-182. bja.oxfordjournals.org/content/110/2/175.short
- 5. Maloney E, Degenhardt L, Darke S, Mattick R, Nelson E. Suicidal behaviour and associated risk factors among opioid-dependent individuals: a case–control study. Addiction. December (2007) 102 (12) 1933–1941. onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2007.01971.x/full
- 4. Ives T, Chelminski P, Hammett-Stabler C, Malone R, Perhac J, Potisek N, Shilliday B, DeWalt D, Pignone M. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Services Research 2006, 6:46. bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-6-46
- Muhuri P, Gfroerer J, Davies M. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. CBASQ Data Review. 2013 August. archive.samhsa.gov/data/2k13/DataReview/DR006/nonmedical-pain-reliever-use-2013.htm
Resources[edit | edit source]
National Institute on Drug abuse: www.drugabuse.gov/
Substance Abuse and Mental Health Services Administration: www.samhsa.gov/
SAMHSA: Results from the 2014 National Survey on Drug Use and Health
NIDA: Comorbidity- Addiction and Other Mental Illnesses
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 American Psychiatric Association. Opioid Use Disorder Diagnostic Criteria. http://pcssmat.org/wp-content/uploads/2014/02/5B-DSM-5-Opioid-Use-Disorder-Diagnostic-Criteria.pdf Accessed 07 April 2016.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Substance Use Disorders. Substance Abuse and Mental Health Services Administration. 2015. Available at: http://www.samhsa.gov/disorders/substance-use. Accessed April 8, 2016.
- ↑ 3.0 3.1 3.2 3.3 Rudd R, Aleshire N, Zibbell J, Gladden M. Increases in Drug and Opioid Overdose Deaths — United States, 2000–2014. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm?s_cid=mm6450a3_w (accessed 04 April 2016).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Center for Disease Control and Prevention. Understanding the Epidemic. http://www.cdc.gov/drugoverdose/epidemic/index.html (accessed 04 April 2016).
- ↑ 5.0 5.1 5.2 Substance Abuse and Mental Health Services Administration. Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health. http://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf (accessed 04 April 2016).
- ↑ 6.0 6.1 6.2 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. http://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596 (accessed 06 April 2016).
- ↑ 7.0 7.1 Muhuri P, Gfroerer J, Davies M. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. http://archive.samhsa.gov/data/2k13/DataReview/DR006/nonmedical-pain-reliever-use-2013.htm (accessed 04 April 2016).
- ↑ 8.0 8.1 8.2 Wachholtz, A, Foster, S, Cheatle, M. Psychophysiology of pain and opioid use: Implications for managing pain in patients with an opioid use disorder. Drug and Alcohol Dependence. 2015;146:1–6. doi:10.1016/j.drugalcdep.2014.10.023.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Goodman, CC, Snyder, TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013. (Pg 49-51)
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 National Institute on Drug Abuse. Comorbidity: Addiction and Other Mental Illnesses. https://www.drugabuse.gov/sites/default/files/rrcomorbidity.pdf (accessed 06 April 2016).