Neurofibromatosis Type I
Original Editors -Nick Pucillo & Cody Russell from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Nicholas Pucillo, Cody Russell, Lucinda hampton, Elaine Lonnemann, WikiSysop, Kim Jackson, Shaimaa Eldib and Wendy Walker
Definition/Description[edit | edit source]
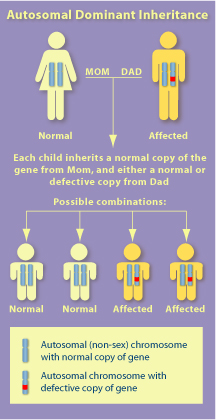
Neurofibromatosis Type 1 (NF1) is an autosomal dominant disorder on the long arm of chromosome 17, characterized by predominately benign tumor growth on nerve sheathes called neurofibromas and cutaneous spotting called café-au-lait macules. The role of the mutated, naturally occurring protein neurofibromin is not fully understood but does appear to play some role in regulating Ras proteins which promote cell division and growth. NF1 varies a great deal in presentation and complications, even between immediate family members.[1][2]
Prevalence[edit | edit source]
Neruofibromatosis type 1 affects approximately 1 in 3,000 peolple worldwide. Neruofibromatosis occurs equally between sexes and races.[3]
Characteristics/Clinical Presentation
[edit | edit source]
Neurofibromatosis type 1 has dermal, ocular, neoplastic, neurological, cardiovascular, and orthopedic manifestations. These various manifestations are what calls for aggressive treatment from a multidisciplinary team.
Dermal Manifestations
- Cafe-au-lait macules (CALM): CALM is one of the most prevalent features of NF1. These macules are usually on of the first features to present in patients. These lesions are flat along the patient's skin and have a coffee-colored hyperpigmentation. The lesions are also round with well-defined borders and have an average diameter of 2-5 cm. [3]CALM is one of the cardinal diagnostic criteria for NF1. When multiple macules are present, NF1 is highly suggestive. [4]
- Skin Fold Freckling: Skin fold freckling are little brown macules that appear in regions where freckling is uncommon. These areas include the axilla, inguinal region, breast folds, neck, and upper eyelids. [3]Skin fold freckling is also involved in the diagnostic criteria for NF1 and usually occurs around the ages of 3 to 5 years. [4]
Ocular/Orbital Manifestations
- Lisch Nodules: Lisch nodules are hyperpigmentations of the iris. The hamartomas are affected consisting of a spindle-shaped cells. Lisch nodules do not cause visual impairments. [3]Visualization requires slit lamp examination by experienced practitioner. Eye examination is necessary in individuals in which the diagnosis of NF1 is uncertain. [4]
- Optic Pathway Glioma (OPGs): OPG is a tumor of the optic nerve and is present in 15% to 20% of NF1 patients. The tumor is slow growing and clinically presents as eye proptosis, decreased visual acuity, or precious puberty. Symptoms usually present before the age of 6 with diagnosis made by 3 years of age. [4]
Neoplastic Manifestaions
- Neuofibroma: Neuorfibromas are benign neoplasms of peripheral nerve sheaths. They are composed of schwann cells, fibroblast, perineural cells, and mast cells. Neurofibromas typically evolve in late childhood. Nerofibromas can increase in both size and magnitude with time with periods of accelerated proliferation during puberty and pregnancy. [3]Neuofibromas are a hallmark sign of NF1 and present as dome-shaped, soft, fleshy, slightly hyperpigmentated cutaneous tumors. Subcutaneous neruofibromas present as firm and nodular. [4]
- Plexiform Neurofibroma (PN): The plexiform neuorbifroma differs from cutaneous neruofibroma in that PN is usually congenital. PNs present as hyperpigmentated and/or hypertrichosis tumors and can develop into malignant peripheral nerve sheath tumors. [4]
- Malignancies: Individuals with NF1 are at a greater risk of developing benign and malignant neoplasms. These neoplasms include melanoma, leukemia, rhabdomyosarcoma, pheochromocytoma, carcinoma, and pancreatic endocrine tumors. [3]
Neurologic Manifestations
- Learning Disability: 75% of NF1 children have some sort of learning disability. Speech and language deficits have been noted along with delayed gross motor development. [3]Frequent assessments must be made for developmental milestone delays, learning disabilities, and school performances. [4]
Cardiovascular Manifestations
- Individuals with NF1 are at a greater risk for stroke, hypertension, congenital heart disease, and vasculopathy. [3]
Orthopaedic Manifestations
- Spinal Deformity: Spinal deformity is common in NF1 and is thought to be caused by osteomalacia, intraspinal neruofibromas that erode and infiltrate bone, and endocrine disturbances. Several dystropic changes in NF1 are rib penciling, vertebral scalloping, dumbbell lesions, and dural ectasia. Less common Dystropic changes are spindling of the transverse process, vertebral wedging and rotation, foraminal enlargement, widened interpediculate distance, and dysplasia of the pedicles. [3]
- Scoliosis: The most common orthopedic finding in NF1 patient's is scoliosis and usually manifests around 10 years of age. The pathogenesis of scoliosis is uncertain but may be related to osteopenia and subsequent dysplasic bones. [4]Individuals with NF1 will require regular scoliosis screenings and should be evaluated with MRI or CT scans for accurate assessment of the deformity. Management of the scoliosis is based primarily on the degrees of the curvature of the spine. [3]
- Long Bone Dysplasias: The most commonly affected long bone in individuals with NF1 is the tibia. The tibia will typically bow in an anterior-lateral direction. Overgrowth or congenital pseudoarthrosis are common dysplasias of NF1. These dysplasias produce abnormalities in fracture healing. [4] Deformities in NF1 typically involve cortical thickening with a narrowed medullary canal. [3]
Associated Co-morbidities[edit | edit source]
Associated psychiatirc morbidity have been reported with NF1. Autism spectrum disorder and attention-deficit-hyperactivity disorder have shown to have a high prevalence with individuals with Neruofibramatosis type 1. [5] Hypertension is also significantly associated with NF1. The leading cause of hypertensions in NF1 patients is due to the stenosis of the renal arteries which decrease blood flow to the kidneys.[6]
Medications[edit | edit source]
The following is a list depicting common medications prescribed addressing signs/symptoms of Neruofibromatosis Type 1:[7]
- Antihistamines: Diphenhydramine (Benadryl, Benylin, Diphen, AllerMax)- May control itching by blocking effects of histamine
- Alpha-adrenergic blocking agents: Prazosin (Minipress), Doxazosin (Cardura)- Cause vasodilation of veins and arterioles and decrease total peripheral resistance and blood pressure
- Antineoplastic agents: Erlotinib (Tarceva), Sorafenib (Nexavar), Carboplatin (Paraplatin)- Inhibit cell growth and proliferation
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Neruofibromatosis type 1 is diagnosed through clinical assessment including patient history and physical examination. The National Institutes of Health have developed a diagnostic criteria for NF1 based upon common clinical features. The diagnosis is made by an individual having 2 or more of the following features:
- Six or more cafe au laite macules > 5 mm in prepubertal individuals and > 15 mm in diameter in adults.
- Two or more neruorfibromas.
- Freckling in the axillary or inguinal regions.
- Optic glioma visual pathways tumors most often presenting as grade I pilocytic astrocytomas.
- Two or more Lisch Nodules
- Abnormal development of the spine (scoliosis), the sphenoid bone, or the tibia.
- A first degree relative with NF1
Early diagnosis is challenging because of the variable characteristics of NF1.[1] Diagnosis my be delayed due to the different ages that features can emerge. [3]
Etiology/Causes[edit | edit source]
The genetic disorder that is Neruofibromatosis Type 1 originates from the NF1 gene that is located in the long arm of chromosome 17. While the role of the NF1 gene is not fully understood, it is known, however, that it produces the protein product neurofibromin. Neurofibromin indirectly dictates cell growth and division, at especially high levels in the nervous system (predominately as a suppressor). In individuals with Neurofibromatosis Type 1, neurofibromin is not produced in sufficient quantities to inhibit cell growth and thus, neruofibromas form along the nerves. While predominately all neuromas of Neurofibromatosis Type 1 are benign, there is a rare occasion in which a neuroma may be malignant (8-13%, especially so in 20-35 year olds). [1][8]
Systemic Involvement[edit | edit source]
Musculoskeletal: Children with NF1 have been shown to have significantly lower motor proficiency than there peers without NF1. NF1 patients also have spinal malalignments resulting in scoliosis and a tendency to have long bone bowing in such bones as the tibia. [9][3]
Dermatological: Patient's with NF1 may develop a variety of cutaneous finding. Cafe-au-lait macules, Nerofibromas, skin freckling are all physical presentations associated with NF1. Other cutaneous findings include juvenile xanthogranuloma, glomus tumor, melanoma, nevus anemicus, and Pruritus. [4]
Vision: The presentation of Lisch Nodules and Optic Gliomas may have an affect on NF1 patient's vision. Individuals with Optic Gliomas may present with eye proptosis, decreased visual acuity, nystagmus, and optic disk atrophy. [4][3]
Cardiovascular: Individuals with NF1 could have cardiovascular manifestations such as congenital heart disease, vasculopathy, and hypertension. Heart disease occurs at a higher than expected rate than the general public. Vasculopathies include stenosis, aneurysms, and arteriovenous malformations. High blood pressure is significantly associated with NF1. The most common cause of hypertension in the pediatric population is stenosis of the renal arteries. Blood pressure should be monitored annually.[6]
Cognitive: Learning disabilities occur in NF1 patients. Children with NF1 have had noted delays in speech and language as well as motor development. There is a proposed relationship between unidentified bright objects on MRI and cognitive function but researchers are unsure of their clinical significance. [4][3]
Medical Management (current best evidence)[edit | edit source]
Currently there is no treatment for the underlying cause of Neurofibromatosis Type 1. While several drugs have been administered and tried for both addressing etiology and symptoms, there have been few proven to have substantial benefits. Diphenhydramine (Benadryl, Benylin, Diphen, AllerMax) has been shown to give most comfort and relief for unceasing itching. Research trials continue in hopes for finding a cure, however, best medical management currently involves routine examinations by a team of health care clinicians. [1][7][10]
Physical Therapy Management (current best evidence)[edit | edit source]
- Best practice of physical therapy in individuals with NF1 has not been identified in research. Recognizing and treating impairments that manifest due to the underlying pathology is within our scope and should be considered when evaluating and treating a patient with NF1.
- As a profession it is important to recognize the manifestations and diagnostic criteria of NF1 in order to screen appropriately regarding orthopedic, neurological, cardiovascular, integumentary, and cognitive impairments.
- A series of case reports have been published depicting the benefits of strength training, stretching, postural training, and palliative medicine. [11] [12]
Differential Diagnosis[edit | edit source]
Following is a comprehensive list of diagnosis that potential mimic NF1:[8]
Other forms of neurofibromatosis
• Segmental/mosaic NF1 (http://www.nfauk.org/assets/downloads/SEGMENTAL%20NF1%20June%202011-6.pdf)
• Watson syndrome (http://rarediseases.info.nih.gov/gard/5540/watson-syndrome/resources/1)
• Autosomal dominant multiple café au lait patches alone (some allelic with NF1) (http://escholarship.org/uc/item/3d56c2q8)
• Neurofibromatosis 2 (http://www.physio-pedia.com/Neurofibromatosis_Type_II)
• Schwannomatosis (http://www.ctf.org/Learn-About-NF/Schwannomatosis.html)
Other conditions with café au lait patches
• McCune–Albright syndrome (http://ghr.nlm.nih.gov/condition/mccune-albright-syndrome)
• DNA repair syndromes (http://www.geneskin.org/dna-repair-disorders.aspx)
• Homozygosity for one of the genes causing hereditary non‐polyposis cancer of the colon. (http://www.ncbi.nlm.nih.gov/books/NBK1211/)
Conditions with pigmented macules confused with NF1
• LEOPARD syndrome (http://ghr.nlm.nih.gov/condition/multiple-lentigines-syndrome)
• Neurocutaneous melanosis (http://www.ncbi.nlm.nih.gov/pubmed/1869648)
• Peutz–Jeghers syndrome (http://ghr.nlm.nih.gov/condition/peutz-jeghers-syndrome)
• Piebaldism (http://ghr.nlm.nih.gov/condition/piebaldism)
Localized overgrowth syndromes
• Klippel–Trenauny–Weber syndrome (http://ghr.nlm.nih.gov/condition/klippel-trenaunay-syndrome)
• Proteus syndrome (http://ghr.nlm.nih.gov/condition/proteus-syndrome)
Conditions causing tumors confused with neurofibromas
• Lipomatosis (http://www.pathologyoutlines.com/topic/softtissueadiposelipomatosis.html)
• Banayan–Riley–Ruvalcuba syndrome (http://ghr.nlm.nih.gov/condition/bannayan-riley-ruvalcaba-syndrome)
• Fibromatoses (http://rarediseases.info.nih.gov/gard/6439/fibromatosis/resources/1)
• Multiple endocrine neoplasia type 2B (http://ghr.nlm.nih.gov/condition/multiple-endocrine-neoplasia)
Case Reports/ Case Studies[edit | edit source]
Physical therapy as conservative management for cervical pain and headaches in an adolescent with neurofibromatosis type 1: a case study.
www.ncbi.nlm.nih.gov/pubmed/20208466
Effects of a plyometric training program for 3 children with neurofibromatosis type 1.
www.ncbi.nlm.nih.gov/pubmed/22466394
Resources
[edit | edit source]
http://www.hopkinsmedicine.org/neurology_neurosurgery/specialty_areas/neurofibromatosis/nf1/
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XaEVbf0Ww08RnamtriDyix1cfDvnZKeXSnVZn5r: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 Julian N, Edwards NE, DeCrane S, Hingtgen CM. Neurofibromatosis 1: Diagnosis and Management. The Journal for Nurse Practitioners. 2014;10(1):30-35.
- ↑ Genetics Home Reference. Neurofibromatosis type 1. Available at: http://ghr.nlm.nih.gov/condition/neurofibromatosis-type-1. Accessed March 4, 2014].
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 Feldman DS, Jordan C, Fonseca L. Orthopaedic manifestations of neurofibromatosis type 1. J Am Acad Orthop Surg. 2010;18(6):346-57.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61(1):1-14.
- ↑ Garg S, Lehtonen A, Huson SM, et al. Autism and other psychiatric comorbidity in neurofibromatosis type 1: evidence from a population-based study. Dev Med Child Neurol. 2013;55(2):139-45.
- ↑ 6.0 6.1 Williams VC, Lucas J, Babcock MA, Gutmann DH, Korf B, Maria BL. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123(1):124-33.
- ↑ 7.0 7.1 emedicine.com. Accessed March 4, 2014].
- ↑ 8.0 8.1 Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44(2):81-8.
- ↑ Johnson BA, Macwilliams BA, Carey JC, Viskochil DH, D'astous JL, Stevenson DA. Motor proficiency in children with neurofibromatosis type 1. Pediatr Phys Ther. 2010;22(4):344-8.
- ↑ Rosalie E Ferner. Neurofibromatosis 1. European Journal of Human Genetics. 2006;15(2):131.
- ↑ Johnson BA, Salzberg CL, Stevenson DA. Effects of a plyometric training program for 3 children with neurofibromatosis type 1. Pediatr Phys Ther. 2012;24(2):199-208.
- ↑ Helmers KM, Irwin KE. Physical therapy as conservative management for cervical pain and headaches in an adolescent with neurofibromatosis type 1: a case study. J Neurol Phys Ther. 2009;33(4):212-23.
- ↑ Neurofibromatosis. Available at:http://www.youtube.com/watch?v=BQBKQB3zq9s