Neonatal Intensive Care Unit (NICU)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Stella Constantinides, Kim Jackson and Vidya Acharya
Introduction[edit | edit source]
Neonatal Intensive Care Units (NICUs) is for those infants who are preterm, have low birth weight, or perinatal problems, or congenital abnormalities, respiratory disorders, neuromuscular disorders and for those who have undergone thoraco-abdominal surgery[1]. A NICU has advanced life support equipment and a team of highly skilled specialist medical and nursing staff to meet the unique needs of newborn babies.[2]
Neonatal staff
Healthcare professionals must collaborate closely with parents, providing them with the necessary guidance and support."There are different types of staff in a NICU including:
- Neonatologists :A pediatrician who specialise in looking after premature or ill newborns.
- Nurses and midwives with special training in neonatal care
- Physiotherapist , Occupational , Speech therapist
- Lactation consultants
- Allied healthcare providers such as social workers
- Other medical specialists such as anaesthetists or surgeons[2]
Levels of neonatal care[edit | edit source]
- Level 1 :Newborns born 35 - 37 week gestation
- Level 2 : Special Care Nursery : Above 32 weeks gestation and weigh >1500g
- Level 3: Provide life support : Βelow 32 weeks gestation and <1500g
Role of physiotherapy[edit | edit source]
The presence of a physical therapist in the Neonatal Intensive Care Unit (NICU) has been found to be influential in reducing physical impairments and limitations in the infants, as well as in educating the family on how to provide optimal care for their newborn.Parent's education and cooperation are very essential regarding the NICU physiotherapy and invasive procedures adopted in the NICU.[3]
The practice pattern of physiotherapists for neonates in neonatal intensive care units involves both chest physiotherapy as well neuromuscular physiotherapy[1].
Neuromuscular Physiotherapy[edit | edit source]
For neuromuscular dysfunction, common therapeutic strategies for neuromuscular physiotherapy include positioning, skin to skin holding (kangaroo care), therapeutic handling, orofacial stimulation, taping, range of motion exercise, soft tissue mobilization (surgical scar release), hydrotherapy and parent education (feeding, dressing, positioning of infants for sleep, interaction/play).
These developmental strategies are beneficial for the promotion of posture and movement appropriate to gestational age and medical stability, to modulate sensory stimulation in the infant's NICU environment, to promote behavioral organization and physiological stability, to foster infant-parent attachment, and to provide direct intervention for neonatal feeding dysfunction and oral motor deficits.[1] The systematic review of studies and meta-analysis shows that the oral sensory-motor stimulation intervention is effective in managing premature infants in the NICU and is beneficial for acquiring independent oral feeding in preterm infants by decreasing the days of admission and the number of days to reach full oral feeding.[4]
Physiotherapists provide parent education on passive range of motion exercise, therapeutic handling, and positioning. A passive range of motion is mainly given to the infant who has congenital restriction of joint mobility.[1]
Due to prolonged immobilization, lack of physical activity leads to demineralization and growth retardation of bone in newborns. Studies tell that the range of motion exercises performed by therapist in different joints helps in increasing bone mineral density and weight gain in premature newborns
Chest physiotherapy[edit | edit source]
Chest physiotherapy techniques eg percussions, vibrations, positioning for postural drainage, and airway suctioning may be required eg 15 min, twice a day. At least 2—3 min be spent on each affected site while giving chest physical therapy for the airway clearance and to maintain the adequate levels of oxygenation[3].
Pain[edit | edit source]
In the NICU, neonates experience long-term sequel of pain during invasive medical procedures. Additionally, infants born extremely premature exhibit changes in their pain perception thresholds and an increased activation of cortical regions in response to painful stimuli .
Newborn babies receive routine medical procedures such as heel sticks and blood tests that can cause them pain. Premature or sick babies undergo these procedures more frequently, increasing their exposure to pain.
There are techniques which healthcare professionals can use to eliminate the level of pain such as:
- Glucose or sucrose, can help reduce pain and discomfort during procedures such as heel sticks.
- Kangaroo care, swaddling helps in pain reduction and influences the positive neurobehavioral states.
- Supporting holding:Gentle holding, which involves placing a hand on the infant's head and feet or body, can be a non-intrusive intervention that does not cause distress to the newborn.
- Hydrotherapy helps in pain reduction and improvement in sleep cycle of hospitalized stable premature newborn. [3]
Developing Countries[edit | edit source]
Modern neonatal intensive care units symbolises sophistication, and high cost automatically follows. The projected requirements in terms of money, manpower and material involved put this treatment virtually out of reach for the developing countries.[5] However more neonatal intensive care units are being built in developing countries ( Latin America, Asia, and Africa) in order to reduce their pre-term mortality. Increased understanding of accessible prenatal and neonatal intensive care facilities and high birth levels in emerging regions is driving the growth of this market. This led to a rise in demand for neonatal intensive care centers[6].
Parental Stress[edit | edit source]
Parental stress related to NICU admission is a worldwide healthcare issue. Immediate and tailored support and education for parents after the birth of their at-risk infant should be prioritized to reduce parental stress and to promote mothers and fathers' emotional well-being and new-born neurodevelopmental outcomes.[7]
The NICU can be overwhelming for parents as there are many pieces of equipment. The staff should explain to the parents what treatment, equipment and monitoring the baby needs eg. An incubator or heated cot to help regulate body temperature, a ventilator that assists breathing (in NICU), machines to deliver fluids/medicines via tubes directly into their veins, monitors attached to the baby’s body so that their heart rate, breathing rate and blood oxygen levels can be checked[2].
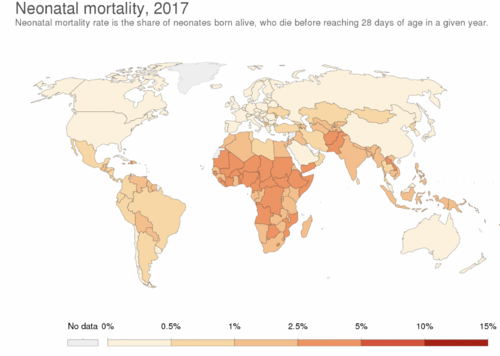
Mortality[edit | edit source]
Although neonatal care is expensive, it has been shown to be effective. In 1960, a 1- kilogram infant had a mortality risk of 95%. By 2000, it had a 95% chance of survival. The mortality rate dropped from 2.6% in 1960 to 0.69% in 2007 and 0.59% in 2016. These rates are decreasing despite an increase in the number of preterm deliveries, which in 2006 accounted for 12.8% of all births (data from North America).[8]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Chokshi T, Alaparthi GK, Krishnan S, Vaishali K, Zulfeequer CP. Practice patterns of physiotherapists in neonatal intensive care units: A national survey. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2013 Nov;17(6):359. Available:https://pubmed.ncbi.nlm.nih.gov/24501488/ (accessed 6.10.2021)
- ↑ 2.0 2.1 2.2 cahs health NICU Available:https://cahs.health.wa.gov.au/Our-services/Neonatology/Neonatal-Intensive-Care-Unit (accessed 6.10.2021)
- ↑ 3.0 3.1 3.2 Sharma N, Samuel AJ, Aranha VP. Pediatric physiotherapists' role in the neonatal intensive care unit: Parent and health-care providers' perspectives. Journal of Clinical Neonatology. 2018 Jul 1;7(3):111. Available: https://www.jcnonweb.com/article.asp?issn=2249-4847;year=2018;volume=7;issue=3;spage=111;epage=115;aulast=Sharma(accessed 6.10.2021)
- ↑ Rodriguez Gonzalez P, Perez-Cabezas V, Chamorro-Moriana G, Ruiz Molinero C, Vazquez-Casares AM, Gonzalez-Medina G. Effectiveness of Oral Sensory-Motor Stimulation in Premature Infants in the Neonatal Intensive Care Unit (NICU) Systematic Review. Children. 2021 Sep;8(9):758.
- ↑ Daga SR, Daga AS. Neonatal intensive care in the developing countries: conservative or aggressive approach. InChild Health in the Tropics 1985 (pp. 233-245). Springer, Dordrecht.Available: https://link.springer.com/chapter/10.1007/978-94-009-5012-2_23 (accessed 7.10.2021)
- ↑ Cision Insights on the Neonatal Critical Care Global Market to 2026 - Featuring Cardinal Health, Medtronic & Ambu Among Others Available: https://www.prnewswire.com/news-releases/insights-on-the-neonatal-critical-care-global-market-to-2026---featuring-cardinal-health-medtronic--ambu-among-others-301141929.html (accessed 7.10.2021)
- ↑ Caporali C, Pisoni C, Gasparini L, Ballante E, Zecca M, Orcesi S, Provenzi L. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. Journal of Perinatology. 2020 Dec;40(12):1739-52.Available: https://pubmed.ncbi.nlm.nih.gov/32901116/ (accessed 7.10.2021)
- ↑ Rajan St. Available:https://www.ahip.org/wp-content/uploads/2018/11/MCG-White-Paper-Neonatal-Care-and-the-NICU-AHIP.pdf (accessed 7.10.2021)