Myofascial Pelvic Pain
Original Editor - Joseph Ayotunde Aderonmu
Top Contributors - Joseph Ayotunde Aderonmu, Khloud Shreif, David Olukayode, Kim Jackson and Leana Louw
Introduction[edit | edit source]
Myofascial Pelvic Pain (MPP) also called Myofascial Pelvic Pain Syndrome (MPPS) is a condition which affects the musculoskeletal system.[2] It is usually an unrecognized and untreated component of chronic pelvic pain (CPP) associated with high percentage of misdiagnosis, and high failure rate of medical interventions. Due to the above, it results in frustrated specialists and patients.[3]
Myofascial pelvic pain refers to pain found in the pelvic floor musculature and connecting fascia. It is characterized by adverse symptoms of tender points, myofascial trigger points (MTrPs) in skeletal muscles.[4][5] It could exist alone with no concomitant medical pathology, exist as either a precursor or sequela to urological, gynecological, and colorectal medical conditions or other musculo-skeletal-neural issues. The hallmark diagnostic indicator of MFPP is myofascial trigger points in the pelvic floor musculature that refer pain to adjacent sites.[6][2]
Studies in the CPP literature have demonstrated existence of MTrPs or hypertonic pelvic floor muscles in medical conditions of different origins.[4][7][8] Yet, MPP is often overlooked by first-line health care providers as either a primary or contributing source of pain for conditions such as urgency/frequency, urge incontinence, constipation, dyspareunia, endometriosis, vulvodynia, coccygodynia, pudendal neuralgia, post-surgical or birthing pelvic pain, interstitial cystitis/painful bladder syndrome (IC/PBS). [9][4][10][7][8][11][12][13]
Epidemiology[edit | edit source]
Pelvic pain affects 3.8–24% of women ages 15–75 years old. Annually, pelvic pain is the primary indication for 10% of outpatient gynecology visits, 40% of diagnostic laparoscopies, 12–17% of hysterectomies.[14] A female chronic pelvic pain clinic reported that 14% to 23% of women with chronic pelvic pain have myofascial pelvic pain. [15] This can get as high as 78% among women with interstitial cystitis.[4][6]
Clinically Relevant Anatomy[edit | edit source]
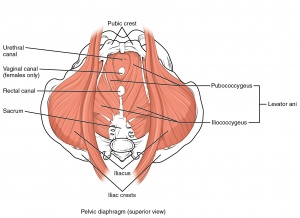
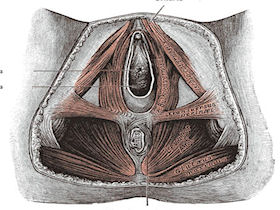
The pelvic floor or perineum is that part of the trunk that is located below the pelvic diaphragm. The pelvic floor is bounded by [17][18]:
Anal triangle (posterior part)[edit | edit source]
Contains the anal canal, the ischiorectal fossae on each side, and the external anal sphincter;
Urogenital triangle (anterior part)[edit | edit source]
Contains the external genitalia and terminal portions of the urogenital ducts
The posterior part is closed by the pelvic diaphragm, and the anterior part of the inferior part of the pelvis is closed by the urogenital diaphragm.
Primarily, the pelvic floor musculature provide the following essential roles[19]:
- Provide support for the pelvic organs and their contents
- Withstand increases in intra-abdominal pressure
- Contribute to stabilization of the spine/pelvis
- Maintain continence at the urethral and anal sphincters
- Sexual response and reproductive function
Etiology[edit | edit source]
MPP is caused by factors that affect muscular strain, circulation and pain, which could be[20][21]:
Mechanical Factors[edit | edit source]
Factors such as direct trauma, chronic poor posture or body mechanics, ergonomic stressors, joint hypermobility, leg length discrepancy, scoliosis, pelvic torsion can result in increased muscle strain due to low-level static exertion of the muscle during prolonged motor tasks, resulting in muscle pain and injury.[3]
Mechanical factors may also occur from prior surgeries, birthing trauma, childhood falls, injuries, accidents, illnesses, physical or sexual abuse, repetitive movement patterns, muscular strains which can cause decreased circulation, localized hypoxia, and ischemia. These conditions can ultimately result in the formation of MTrPs.[22][23]
Nutritional Factors[edit | edit source]
Nutritional deficiencies are often common among women with MPP but often overlooked. Deficiencies of vitamins B1, B6, and B12, folic acid, vitamin C and D, iron, magnesium, and zinc have all been associated with chronic MTrPs. In people with chronic MTrPs, 16% have insufficient B12 levels, whereas 90% lack proper vitamin D.[24]
Psychological Factors[edit | edit source]
Psychological stress may also activate underlying MTrPs. Stress, hyper-responsible personalities, depression, anxiety-depression syndrome can all contribute to the activation of MtrPs [25]. Mental and emotional stress have been shown to increase the electromyographic activity in MTrPs, whereas neighboring muscle without trigger points remains electrically unchanged.`[24]
Other factors that can result in MPP include chronic infections, metabolic factors. [20][21]
Mechanism of Myofascial Pelvic Pain[edit | edit source]
Symptoms of MPP are caused by tender points and MTrPs in pelvic floor muscles. These trigger points usually refer sensation or pain to adjacent sites. These referral patterns do not present in classic nerve or dermatomal regions, (although characteristic referral patterns for pelvic MTrPs have been well documented).[6]
Myofascial trigger points are localized, often extremely painful lumps or nodules in the muscles (“taut bands”) or associated connective tissue known as fascia.[26][6][27]
They are classified as either active, secondary or latent[28]:
Active Trigger Points[edit | edit source]
- Produce local or referred pain or sensory disturbances without stimulation.
- Always sensitive.
- Constantly painful spots.
- Pain increases on palpation, pressing, stretching and mobilizing the muscle.
Latent Trigger Points[edit | edit source]
- Develop within reference area of original trigger point.
- Will not trigger symptoms unless activated by an exacerbating physical, emotional, or other associated stressor.
- They become active on activation.
Secondary TrPs[edit | edit source]
- Appear in response to the contraction of agonist and antagonist muscles that attempt to compensate for the injured muscle.
Clinical Presentation[edit | edit source]
The symptoms of MPP are described in any area of the pelvis and pelvic floor as well as referred to distal areas in the abdomen, back, or legs.
Pain[edit | edit source]
Resting symptoms[edit | edit source]
Often triggered by specific factors such as menses, long walks, prolonged sitting, defecation, sexual intercourse.[10]
Differential Diagnosis[edit | edit source]
- Fibrositis or fibromyalgia
- Joint disorders [3]
Diagnosis Procedures[edit | edit source]
Physical Examination[edit | edit source]
The clinician’s investigation of MTrPs, is directed by a detailed history, examination of movement patterns, knowledge of referred pain patterns. A manual examination of the pelvic floor is essential to determine the presence of trigger points. Trigger points are best palpated perpendicularly to the muscle fibre attempting to find the taut band and tender nodule in the abdomen, pelvis, and perineum, a flat approach, using the finger pads is preferred. During physical examination, a reliable clinical criteria have been developed to detect a trigger point include the following: [2][3]
- A palpable taut band,
- An exquisitely tender nodule in the taut band,
- Reproduction of the woman’s pain with pressure on the tender nodule,
- Painful limit to stretch or full range of motion.
- An additional sign of a trigger point is a palpable, visible local twitch response, also referred to as “jump sign” when a trigger point is palpated.
Electrophysiological Studies[edit | edit source]
It is common to find an increased basal muscular activity at rest which is related to the pathogenesis of the process; this can be quantified by averaging the turn/amplitude obtained in electromyographic(EMG) analysis.[3]
Thermography[edit | edit source]
Thermographically, a TrP appears as a small area that has a temperature between 0.6 and 1°C higher than the surrounding tissue or its contralateral area. [29]
Confirmatory findings of Myofascial Syndrome[3][edit | edit source]
- Local twitch response induced by palpation or by inserting an EMG needle through a TrP, which is evidenced by detection of movement by sight, palpation, or ultrasound imaging.
- Referred pain patterns for each muscle.
- Motor endplate noise when an EMG needle is inserted into the TrP.
Management[edit | edit source]
A multidisciplinary approach is best approach to management of MPP. The team could consist of the following healthcare professionals: [2]
- Physiatrist: Refers to the physical therapist if MPP is suspected or if the musculoskeletal screening and pelvic floor muscle assessment reproduces symptoms.
- Physical therapist.
- Psychologist: to help manage psychological/emotional issues.
- Clinical sexologist or sex therapist to assist with sexual concerns.
- Urologists, urogynecologists, gastroenterologists, and other specialists (as appropriate).
Medical Management[edit | edit source]
This could involve the following: [30][31]
- Antibiotics (in case of pelvic infections)
- Local anesthesia (to inactivate trigger points)
Physical Therapy Management[edit | edit source]
A comprehensive history specifically regarding the nature, progression, and stability of the pain and related urinary, gastrointestinal, or sexual symptoms are obtained to in relation to the patient’s complaints. Also, a physical examination serves to determine the primary and contributing pain generators, establish baseline status using objective measures including functional activities for future reassessment, and to initiate an appropriate plan of care. [9][32]
Pelvic Floor Rehabilitation[edit | edit source]
Pelvic floor rehabilitation is a component of the treatment for MPP. Treatment interventions include:
- Myofascial release of painful trigger points of the pelvic floor myofascial release [33]
- Stretching exercises to the hip, gluteal, pelvic and abdominal muscles
- Contract-relax technique followed with prolonged stretch.[8][34] [35]
Patient Education[edit | edit source]
Patients have to be educated on activities that might exacerbate symptoms (such as kegels exercises, abdominal contractions, tight clothings). Also, in the management of MPP, it is beneficial to educate patients on proper posture, self-management and relaxation techniques.[8][34][35] Patient education could also include cognitive coping strategies on psychological factors which might trigger pain in the condition.[36]
Prognosis[edit | edit source]
Clear signs of improvement are seen in most cases after three or four months of treatment with medical and physical therapy management, with two weekly one-hour sessions, a daily program of specific stretches at home, body relaxation techniques, and stress management. However, up to two years may be necessary for a stable and permanent improvement of myofascial syndrome. [3]
Conclusion[edit | edit source]
Myofascial pelvic pain is a major component of CPP in women that is often not properly identified by health care providers. Women presenting with myofascial pelvic pain may describe symptoms in the pelvis, pelvic floor, and distally in the abdomen, back, and legs. A proper musculoskeletal screening and pelvic floor muscle assessment can help reproduce symptoms of MPP component of CPP. Physiotherapy can effectively help in the management of MPP using a comprehensive approach to treatment.
Resources[edit | edit source]
References[edit | edit source]
- ↑ File:1115 Muscles of the Pelvic Floor.jpg. (2018, June 18). Physiopedia, . Retrieved 14:57, September 29, 2020 from https://www.physio-pedia.com/index.php?title=File:1115_Muscles_of_the_Pelvic_Floor.jpg&oldid=191214.
- ↑ 2.0 2.1 2.2 2.3 Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2012 Sep 1;41(5):680-91.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Itza Santos F, Zarza D, Serra Llosa L, Gómez Sancha F, Salinas J, Bautrant E. Myofascial pain syndrome in the pelvic floor: etiology, mechanisms, symptoms, diagnosis, and treatment. Pelvic Pain: Causes, Symptoms and Treatments. 2012.
- ↑ 4.0 4.1 4.2 4.3 Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. International urogynecology journal. 2011 Apr 1;22(4):413-8.
- ↑ Doggweiler-Wiygul R. Urologic myofascial pain syndromes. Current pain and headache reports. 2004 Dec 1;8(6):445-51.
- ↑ 6.0 6.1 6.2 6.3 Itza F, Zarza D, Serra L, Gomez-Sancha F, Salinas J, Allona-Almagro A. Myofascial pain syndrome in the pelvic floor: a common urological condition. Actas Urológicas Españolas (English Edition). 2010 Jan 1;34(4):318-26.
- ↑ 7.0 7.1 Bendaña EE, Belarmino JM, Dinh JH, Cook CL, Murray BP, Feustel PJ, De EJ. Efficacy of transvaginal biofeedback and electrical stimulation in women with urinary urgency and frequency and associated pelvic floor muscle spasm. Urologic nursing. 2009 May;29(3):171.
- ↑ 8.0 8.1 8.2 8.3 Chiarioni G, Nardo A, Vantini I, Romito A, Whitehead WE. Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology. 2010 Apr 1;138(4):1321-9.
- ↑ 9.0 9.1 Apte G, Nelson P, Brismée JM, Dedrick G, Justiz III R, Sizer Jr PS. Chronic female pelvic pain—part 1: clinical pathoanatomy and examination of the pelvic region. Pain Practice. 2012 Feb;12(2):88-110.
- ↑ 10.0 10.1 10.2 Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstetrics and Gynecology Clinics. 2009 Sep 1;36(3):707-22.
- ↑ Doggweiler-Wiygul R. Urologic myofascial pain syndromes. Current pain and headache reports. 2004 Dec 1;8(6):445-51.
- ↑ Gentilcore-Saulnier E, McLean L, Goldfinger C, Pukall CF, Chamberlain S. Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. The journal of sexual medicine. 2010 Feb 1;7(2):1003-22.
- ↑ Neville CE, Fitzgerald CM, Mallinson T, Badillo SA, Hynes CK. Physical examination findings by physical therapists compared with physicians of musculoskeletal factors in women with chronic pelvic pain. Journal of Women’s Health Physical Therapy. 2010 Sep 1;34(3):73-80.
- ↑ Prather H, Spitznagle TM, Dugan SA. Recognizing and treating pelvic pain and pelvic floor dysfunction. Physical Medicine and Rehabilitation Clinics of North America. 2007 Aug 1;18(3):477-96.
- ↑ Tu FF, As-Sanie S, Steege JF. Prevalence of pelvic musculoskeletal disorders in a female chronic pelvic pain clinic. The Journal of reproductive medicine. 2006 Mar;51(3):185-9.
- ↑ File:1115 Muscles of the Pelvic Floor.jpg. (2018, June 18). Physiopedia, . Retrieved 14:57, September 29, 2020 from https://www.physio-pedia.com/index.php?title=File:1115_Muscles_of_the_Pelvic_Floor.jpg&oldid=191214.
- ↑ Rouviere H. Anatomía Humana. 2, tronco. Editorial Masson. 2005.
- ↑ Sobotta J. Atlas de anatomía humana: Cabeza, cuello, miembro superior. Vol. 1. Ed. Médica Panamericana; 2006.
- ↑ Kisner C, Kolby L. Therapeutic Exercise: Foundations and Techniques. 6th ed. Philadelphia, PA: FA Davis Company. 2012:315-29.
- ↑ 20.0 20.1 Fernandez-de-Las-Penas C, Alonso-Blanco C, Miangolarra JC. Myofascial trigger points in subjects presenting with mechanical neck pain: a blinded, controlled study. Manual therapy. 2007 Feb 1;12(1):29-33.
- ↑ 21.0 21.1 De Souza Montenegro ML, Mateus‐Vasconcelos EC, Candido dos Reis FJ, Rosa e Silva JC, Nogueira AA, Poli Neto OB. Thiele massage as a therapeutic option for women with chronic pelvic pain caused by tenderness of pelvic floor muscles. Journal of Evaluation in Clinical Practice. 2010 Oct;16(5):981-2.
- ↑ Hägg GM. Corporate initiatives in ergonomics—an introduction. Applied ergonomics. 2003 Jan 1;34(1):3-15.
- ↑ Sjøgaard G, Jørgensen LV, Ekner D, Søgaard K. Muscle involvement during intermittent contraction patterns with different target force feedback modes. Clinical Biomechanics. 2000 Jan 1;15:S25-9.
- ↑ 24.0 24.1 24.2 Dommerholt J, Bron C, Franssen J. Myofascial trigger points: an evidence-informed review. Journal of Manual & Manipulative Therapy. 2006 Oct 1;14(4):203-21.
- ↑ Berberich HJ, Ludwig M. Psychosomatic aspects of the chronic pelvic pain syndrome. Der Urologe. Ausg. A. 2004 Mar;43(3):254-60.
- ↑ Harden RN, Bruehl SP, Gass S, Niemiec C, Barbick B. Signs and symptoms of the myofascial pain syndrome: a national survey of pain management providers. The Clinical journal of pain. 2000 Mar 1;16(1):64-72.
- ↑ Simons DG, Travell J, Simons LS. Myofascial pain and dysfunction: the trigger point manual: volume 1.
- ↑ Dommerholt J. Persistent myalgia following whiplash. Current pain and headache reports. 2005 Oct 1;9(5):326-30.
- ↑ Diakow PR. Differentiation of active and latent trigger points by thermography. Journal of manipulative and physiological therapeutics. 1992 Sep;15(7):439-41.
- ↑ Guercini F, Pajoncini C, Bard R, Fiorentino F, Bini V, Costantini E, Porena M. Echoguided drug infiltration in chronic prostatitis: results of a multi-centre study. ARCHIVIO ITALIANO DI UROLOGIA ANDROLOGIA. 2005 Jun;77(2):87.
- ↑ Tüzün EH, Albayrak G, Eker L, Sözay S, Daşkapan A. A comparison study of quality of life in women with fibromyalgia and myofascial pain syndrome. Disability and rehabilitation. 2004 Feb 18;26(4):198-202.
- ↑ Banks K, Hengeveld E. Maitland's Clinical Companion E-Book: An Essential Guide for Students. Elsevier Health Sciences; 2009 Oct 20.
- ↑ Grinberg K, Weissman-Fogel I, Lowenstein L, Abramov L, Granot M. How Does Myofascial Physical Therapy Attenuate Pain in Chronic Pelvic Pain Syndrome?. Pain Research and Management. 2019 Dec 12;2019.
- ↑ 34.0 34.1 FitzGerald MP, Anderson RU, Potts J, Payne CK, Peters KM, Clemens JQ, Kotarinos R, Fraser L, Cosby A, Fortman C, Neville C. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. The Journal of urology. 2013 Jan;189(1S):S75-85.
- ↑ 35.0 35.1 FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, Nickel JC, Hanno PM, Kreder KJ, Burks DA, Mayer R. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. The Journal of urology. 2012 Jun;187(6):2113-8.
- ↑ Ortiz DD. Chronic pelvic pain in women. American family physician. 2008 Jun 1;77(11):1535-42.
- ↑ Myofascial Pain Syndrome in the Pelvic Floor. Dr Itza