Myocardial Infarction
Original Editors - Jessica King & Melissa Tuemler from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jessica King, Melissa Tuemler, Lucinda hampton, Vidya Acharya, Kim Jackson, Admin, Elaine Lonnemann, WikiSysop, Wendy Walker, Evan Thomas, Venus Pagare and Karen Wilson
Definition/Description[edit | edit source]
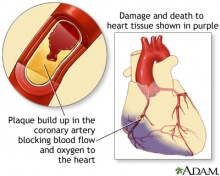
A Myocardial Infarction (MI) occurs when an area of the heart does not receive enough blood flow and is subsequently damaged or dies. An MI is commonly referred to as a heart attack and is always a medical emergency. Many times an MI occurs when one of the main arteries to the heart, specifically the coronary arteries, become blocked due a build up of plaque. Plaque build up occurs when cholesterol and other large cells attach to the arterial walls, and cause narrowing of the arterial canals. When the arteries becomes increasingly narrow due to plaque build up there is no longer adequate blood and oxygen control to the heart, and an MI occurs. Often times an MI can occur suddenly, and without warning signs. Some identified causes of an MI include sudden physical exertion, recent illness, and emotional stress.[1]
Prevalence[edit | edit source]
Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.[2]
Characteristics/Clinical Presentation[edit | edit source]
According to the American Heart Association (AHA), heart attacks can occur in a variety of fashions. Some begin suddenly with severe pain or other symptoms, while others have a slower onset with only mild pain or discomfort. Pain toward the center of the chest is the most common symptom experienced by patients. This pain is typically uncomfortable and resembles the feeling of squeezing or a pressure on the anterior chest. Patients experiencing an MI may also experience pain in the jaw, shoulder, arms, stomach, neck, or back. The other common signs and symptoms of heart attack are listed below. [3]
Signs and symptoms of MI include:
- Chest pain lasting longer than a few minutes
- Anxiety
- Cough
- Fainting
- Lightheadedness/ Dizziness
- Nausea/ Vomiting
- Heart palpitations
- Shortness of air (SOA)
- Sweating
- MI can also be "silent" in which there are no symptoms. [1]
Signs and symptoms vary based on gender. The most common symptom experienced by both genders is chest pain or discomfort. Women typically experience other symptoms such as SOA, nausea and vomiting, and neck or jaw pain.
[3][edit | edit source]
Associated Co-morbidities[edit | edit source]
Associated Co-morbidities for Myocardial Infarction include:
- Hypertension
- Coronary Artery Disease (CAD)
- Congestive Heart Failure (CHF)
- Arthritis
- Diabetes
Medications[edit | edit source]
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives.
|
Anticoagulants (Warfarin) |
Blood thinner. Decreases clotting ability of the blood, but do not dissolve existing clots. |
| Antiplatelet agents (Aspirin) |
Keeps blood clots from forming by preventing blood platelets from sticking together. |
| ACE inhibitors (Benazepril, Captopril, Enalapril) |
Expands blood vessels and decreases resistance by lowering levels of angiotensin II. Allows blood to flow more easily and makes the heart's work easier or more efficient. |
| Angiotension II Receptor Blockers (Candesartan) |
Prevent angiotension II from having any effects on the heart and blood vessels. This keeps blood pressure from rising. |
| Beta Blockers (Acebutolol) |
Decreases the heart rate and cardiac output, which lowers blood pressure and makes the heart beat more slowly and with less force. |
| Calcium Channel Blockers (Amlodipine) |
Interrupts the movement of calcium into the cells of the heart and blood vessels. May decrease the heart's pumping strength and relax blood vessels. |
| Diuretics (Amiloride) |
Causes the body to rid itself of excess fluids and sodium through urination. Helps to relieve the heart's workload. Also decreases the buildup of fluid in the lungs and other parts of the body, such as the ankles and legs. Different diuretics remove fluid at varied rates and through different methods. |
| Vasodilators (Nitrates) |
Relaxes blood vessels and increases the supply of blood and oxygen to the heart while reducing its workload. Can come in pills to be swallowed, chewable tablets and as a topical application (cream). |
| Digitalis Preparations (Lanoxin) |
Increases the force of the heart's contractions, which can be beneficial in heart failure and for irregular heartbeats. |
| Statins |
Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood. |
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
The diagnosis of a heart attack can be completed with the following assessment tools:
- Complete patient medical history
- Physical exam
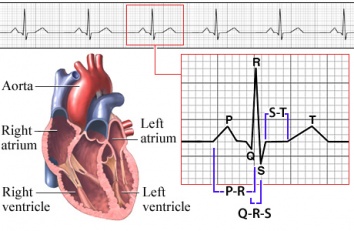
- EKG
- Blood testing to be sure there are no abnormal levels of enzymes in the blood
Diagnostic tests for determining if a patient has had an MI can be invasive or non-invasive.
Non-invasive tests:
- EKG: records the electrical activity of the heart.
- Ambulatory EKG and Holter Monitoring: records the electrical activity of the heart during ADL’s.
- Chest X-ray: photograph of the heart and lungs that helps determine if the heart is enlarged or if fluid is accumulating in the lungs.
- Echocardiogram: hand held device placed over the chest that uses ultrasound to produce images of the heart.
- CT or MRI
- Exercise Stress Test: monitor with electrodes that are attached to chest and monitor the heart response while an individual walks on a treadmill.
Invasive tests:
- Blood Tests: may include cardiac enzymes such as troponin and creatine kinase, C-reactive protein, fibrinogen, lipoproteins, triglycerides, BNP, and prothrombin
- Cardiac Catheterization: examines the inside of the heart and blood vessels using an angiogram and dye. This can measure the blood pressure in side the heart, detect where a narrowing in the vessel is located, and evaluates overall heart function.[5]
Etiology/Causes[edit | edit source]
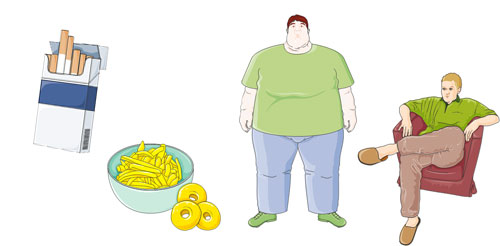
Heart disease has many risk factors, some that can be changed and others that cannot.
Risk factors that cannot be changed include:
- Age (Increased risk after age 65)
- Gender (Males at increased risk)
- Race/ethnicity (African Americans, Mexican Americans, American Indians, Hawaiians and Asian Americans at increased risk)
- Genetics/ Family History
Risk factors that can be changed:
- Smoking
- High cholesterol (diet, exercise, and medication)
- High blood pressure (diet, exercise, and medication)
- DM management
- Exercising at least 30 min/day
- Eating a healthy, nutritious diet
- Stress management
- Limiting alcohol consumption to 1 drink/day for women and 2 drinks/day for men [6]
Systemic Involvement[edit | edit source]
Cardiovascular:
Damage to the heart can lead to some serious effects on the cardiovascular system including decreased peripheral blood flow, dangerous heart arrhythmias, congestive heart failure, and an increased risk for another MI.
Pulmonary:
The pulmonary system is also affected by an MI because there is a decreased level of oxygen saturation due to the damaged heart. Often times during an MI fluid can accumulate in the lungs which could result in damage or infection.
Endocrine:
Many times during an MI the insulin levels spike in individuals, even if they do not have diabetes. Treatment to control the increase in insulin is often required.
Integumentary:
Often times these individuals need to undergo emergency heart surgery, and the incisions need to be monitored for infection.
Medical Management (current best evidence)[edit | edit source]
| Tests | Surgeries | Implanted Medical Devices |
|---|---|---|
| Thrombolysis |
Angioplasty | Left Ventricular Assist Device |
| Artificial Heart Valve Surgery | Pacemaker | |
| Atherectomy | Implantable Cardioverter Defibrillator | |
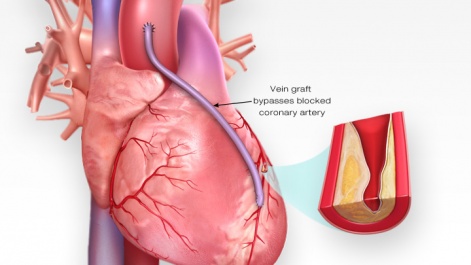
| Bypass Surgery | ||
| Cardiomyoplasty | ||
| Heart Transplant | ||
| Radiofrequency Ablation | ||
| Stent Placement | ||
| Transmyocardial Revascularization |
Tests/Procedures
- Thrombolysis: procedure typically administered within 3-4 hours of an MI. A clot-dissolving agent is injected into a coronary atery to restore normal blood flow.
Surgeries
- Angioplasty: This procedure greatly increases blood flow through a blocked artery. A balloon is threaded into the blocked artery and is inflated to expand the blocked area so blood flow can be restored. A stent is also commonly placed into the blocked artery during this procedure to ensure that a blockage does not happen again.
- Artificial Heart Valve Surgery: procedure replaces unhealthy or deceased heart valves with new, healthy ones.
- Atherectomy: a catheter is threaded through a blocked artery. The catheter has a rotating sharp end that is used to cut away at plaque formation in the wall of an artery.
- Bypass Surgery: one of the most common treatment strategies for managing blocked arteries. New passageways are created by using grafts from veins or arteries from other areas of the body to pass the blocked site so blood can flow freely.
- Cardiomyoplasty: currently an experimental treatment where skeletal muscles are wrapped around the patient body over a weak heart. This will improve the heart's pumping motion when stimulated byb a pacemaker type of device.
- Heart transplant: removal of a diseased heart that is replaced by a human heart from a donor.
- Radiofrequency Ablation: A catheter with an electrode at its tip is guided through the veins to the heart muscle with real-time, moving X-rays displayed on a video screen. The catheter is placed at the exact site inside the heart where cells give off the electrical signals that stimulate the abnormal heart rhythm. Then a mild, painless radiofrequency energy is transmitted to the pathway that carefully destroys selected heart muscle cells in a very small area (about 1/5 of an inch).
- Stent placement: a wire mesh used to hold open an artery during an angioplasty and is then permanently placed in the artery.
- Transmyocardial Revascularization: used to relieve very severe chest pain or angina in patients who are not candidates for a bypass.
Implanted Medical Devices
- Left Ventricular Assist Device: battery operated, mechanical pump device that is surgically implanted into the heart and is used to maintain the pumping ability of a heart that can't effectively work on its own. This device is typically implanted in patients who are on the waiting list for a heart transplant or suffering from end-stage heart failure.
- Pacemaker: device implanted into heart tissue that sends electrical impulses to help maintain a regular heart beat. This device is typically used when the hearts "natural pacemaker" becomes defective and causes the heart to beat at an irregular beat.
- Implantable Cardioverter Defibrillator: a device that is implanted into the heart that can send an electrical shock, detect heart rhythm, and at times pace the hearts rhythm.
Physical Therapy Management (Current Best Evidence)[edit | edit source]
Cardiac Rehab may be beneficial to patients of all ages who have had a heart attack, CAD, angina, or CHF. Other individuals who may gain benefits from this include post- surgical CABG, percutaneous intervention (PCI), or coronary angioplasty patients. A medical examination is completed at the initial consultation to determine the needs and limitations of the patient. After the results of the exam are interpreted, the team creates a rehab program and sets goals for treatment. Treatment typically consists of a physical activity program in a group setting where vital signs can consistently be monitored. As the program progresses, the patient is taught how to monitor their own vitals and progresses to more challenging aerobic activities. Along with physical activity, patient education is also a very important part of cardiac rehab. Patients may work with a dietician or be given advice on how to stop smoking if necessary.
According to the American Heart Association, the benefits of cardiac rehab include:
- Regular physical activity helps your heart and the rest of your body get stronger and work better. Physical activity improves your energy level and lifts your spirits. It also reduces your chances of future heart problems, including heart attack.
- Counseling and education can help you quit smoking, eat right, lose weight, and lower your blood pressure and cholesterol levels. Counseling may also help you learn to manage stress and to feel better about your health.
- You have the advice and close supervision of healthcare professionals to help you improve your health and lower your risk of future problems. These professionals can also communicate with your primary care doctor or cardiologist. [10]
Prevention - Dietary Modification [edit | edit source]
There are alternative/holistic options that can be employed to prevent an MI or additional MIs, which focus around diet and exercise. Regular aerobic exercise can help decrease an individual’s risk for an MI, and promote better overall health and wellness. Meditation and Yoga are two other options that can help cardiac patients recover after an MI and reduce stress that could lead to another MI in the future.
Nutrition is an important factor in reducing an individual’s risk for an MI. A diet low in fatty acids and cholesterol is important to limit the plaque buildup within arteries.
Differential Diagnosis[edit | edit source]
There are many differential diagnoses for patients experiencing an MI, and because there are many distractions an MI can often be missed. All patients that present with symptoms concurrent with an MI should be treated as a medical emergency.
Possible Differential Diagnoses of a MI include:
| Acute Coronary Syndrome | Dissection, Aortic |
Myopericarditis |
| Angina Pectoris |
Dyspepsia |
Pancreatitis |
| Anxiety |
Endocarditis |
Pericarditis and Cardiac Tamponade |
| Anxiety Disorders |
Esophageal reflux |
Pericarditis, Acute |
| Aortic Dissection |
Esophageal Spasm |
Pleurodynia |
| Aortic Regurgitation |
Esophagitis |
Pneumonia |
| Aortic Stenosis |
Gastritis, Acute |
Pneumothorax |
| Asthma |
Gastroenteritis |
Pneumothorax, Iatrogenic, Spontaneous and Pneumomediastinum |
| Biliary tract disease |
Gastroesophageal Reflux Disease |
Pulmonary Embolism |
| Cholecystitis |
Heart arrhythmias |
Pulmonary Hypertension, Primary |
| Cholecystitis and Biliary Colic |
Heart rupture |
Radicular pain |
| Cholelithiasis |
Herpes Zoster |
Shock, Cardiogenic |
| Chronic Obstructive Pulmonary Disease and Emphysema |
Hypotension |
Stroke Imaging |
| Compartment Syndrome, Abdominal |
Mitral Regurgitation |
Tachycardia myopathy |
| Contusions |
Mitral Valve Prolapse |
Unstable Angina |
| Depression |
Myocarditis |
Ventricular Septal Defect |
Case Reports/ Case Studies[edit | edit source]
Chernyavskiy A, Marchenko A, Lomivorotov V, Doronin D, Alsov S, Nesmachnyy A. Left Ventricular Assist Device Implantation. Texas Heart Institute Journal. (2012, Oct), cited February 15, 2013; 39(5): 627-629. Available from: Academic Search Premier.
Marcuccilli L, Casida J. Overcoming alterations in body image imposed by the left ventricular assist device: a case report. Progress In Transplantation (Aliso Viejo, Calif.). (2012, June), cited February 15, 2013; 22(2): 212-216. Available from: MEDLINE.
Narasimhan S, Krim N, Silverman G, Monrad E. Simultaneous Very Late Stent Thrombosis in Multiple Coronary Arteries. Texas Heart Institute Journal. (2012, Oct), cited February 15, 2013; 39(5): 630-634. Available from: Academic Search Premier.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 MedlinePlus. Heart Attack. http://www.nlm.nih.gov/medlineplus/ency/article/000195.htm (accessed 10 Feb 2013).
- ↑ Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)
- ↑ 3.0 3.1 American Heart Association. Warning signs of a Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp (accessed 10 Feb 2013).
- ↑ American Heart Association. Cardiac Medications. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Medications_UCM_303937_Article.jsp (accessed 11 Feb 2013).
- ↑ American Heart Association. Symptoms and Diagnosis of Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/SymptomsDiagnosisofHeartAttack/Symptoms-and-Diagnosis-of-Heart-Attack_UCM_002041_Article.jsp (accessed 10 Feb 2013).
- ↑ MedlinePlus. Heart Disease-risk factors. http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000106.htm (accessed 11 Feb 2013)
- ↑ Beautiful. About Coronary Artery Disease. http://www.beautiful-study.com/static/html/general/about_coronary.asp (accessed 15 Feb 2013).
- ↑ Patient.co.uk. Myocardial Infarction (Heart Attack). http://www.patient.co.uk/health/myocardial-infarction-heart-attack (Accessed on 12 Feb 2013)
- ↑ American Heart Association. Cardiac Procedures and Surgeries. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Procedures-and-Surgeries_UCM_303939_Article.jsp (accessed 11 Feb 2013).
- ↑ American Heart Association.What is Cardiac Rehab? http://www.heart.org/HEARTORG/Conditions/More/CardiacRehab/What-is-Cardiac-Rehabilitation_UCM_307049_Article.jsp (accessed 11 Feb 2013).
- ↑ Medscape. Myocardial Infarction Differential Diagnosis. http://emedicine.medscape.com/article/155919-differential (accessed 14 Feb 2013).