Muscle Repair
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton
Introduction[edit | edit source]
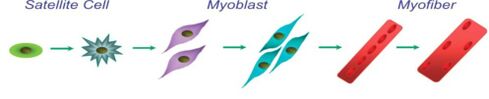
Skeletal muscle repair requires the activation of satellite cells, which are the residential muscle stem cells. The repair/regeneration is a highly coordinated process, involving cell-cell, cell matrix and extracellular matrix interactions. Immune, fibrotic, vascular and myogenic cells all play a role in the three phases of muscle repair/ regeneration. These phases
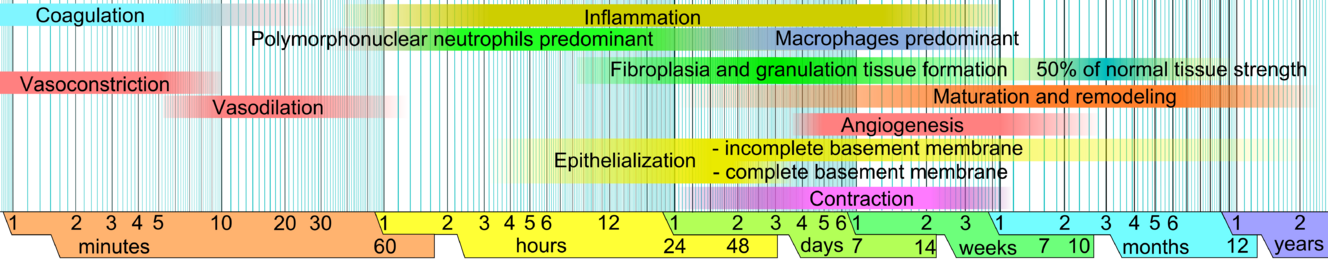
- Destruction phase : distinguished by rupture and necrosis of the myofibers, formation of a hematoma and an critical inflammatory reaction.
- Regeneration phase: phagocytosis of damaged tissue preceding myofibers regeneration, leading to satellite cell activation.
- Remodelling phase: maturation of regenerated myofibers with recovery of muscle functional capacity and fibrosis and scar tissue formation.
Skeletal muscle injuries can be caused by a multitude of events that may be direct trauma eg muscle lacerations and contusions or indirect eg strains and degenerative diseases. With minor muscle injuries regeneration naturally repairs eg post quadriceps strain. On the other hand post severe trauma or degeneration, muscle healing is incomplete, often resulting in the fibrotic tissue with reduced functional capacity.[1]
Physiotherapy Implications[edit | edit source]
Following muscle injury a few days of rest is useful, when the aim is to control inflammation, oedema and pain. This immobilisation time gives the newly formed scar tissue a necessary tensile strength to withstand the forces caused by muscle contractions. Longer immobilisation has adverse effects namely atrophy of healthy muscle, excessive deposition of connective tissue in the muscle tissue and a delay in the return of the injured muscle strength.
In the remodelling phase of muscle healing the actual repair of the injured muscle takes place. Myofibres start regenerating out of satellite cells and a connective tissue scar is being formed in the gap between the torn muscle fibres. In the first 10 days after the trauma, this scar tissue is the weakest point of the affected muscle. After 10 days, however, eventual re-rupture will rather affect adjacent muscle tissue than the scar tissue itself, although full recovery (up to the point of pre-injury strength) can take a relatively long time. Vascularisation of the injured area is a prerequisite for recovering from a muscle injury. New capillaries originate from the remaining injured blood vessels and find their way to the centre of the injured area. Early mobilisation plays a very important role since it stimulates the vascularisation process. Similarly ,intramuscular nerves will regenerate to re-establish the nerve-muscle contact.
The remodelling phase is the longest and the phase in which physiotherapists have the greatest participation and contribution. This phase includes the breaking down of tissue injury components eg fibrotic tissue and restoration of the functional and biomechanical deficits.[2]
Physiopedia has many great muscle repair related pages. Take a look at the following links to get a deeper understanding.
References[edit | edit source]
- ↑ Thomas Laumonier and Jacques Menetrey Muscle injuries and strategies for improving their repair Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4958098/ (accessed 1.7.2022)
- ↑ Medcrave online Physical Rehabilitation of Muscles, Tendons and Ligaments Available: https://medcraveonline.com/MOJOR/physical-rehabilitation-of-muscles-tendons-and-ligaments.html (accessed 1.7.2022)