Multiple Organ Dysfunction Syndrome
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Uchechukwu Chukwuemeka
Introduction[edit | edit source]
Multiple organ dysfunction syndrome (MODS) is a systemic, dysfunctional inflammatory response that requires long intensive care unit (ICU) stay. It is characterized with high mortality rate depending on the number of organs involved.
It has been recognized that organ failure does not occur as an all-or-none rule, but rather a range of organ dysfunction exists resulting in clinical organ failure.[1]
Multiple organ dysfunction syndrome is the clinical consequence of a dysregulated inflammatory response, triggered by clinically diverse factors with the main pillar of management being invasive organ support.
During the last years, the advances in the clarification of the molecular pathways that trigger, mitigate, and determine the outcome of MODS have led to the increasing recognition of MODS as a distinct disease entity with distinct etiology, pathophysiology, and potential future therapeutic interventions.
Given the lack of effective treatment for MODS, its early recognition, the early intensive care unit admission, and the initiation of invasive organ support remain the most effective strategies of preventing its progression and improving outcomes[2].
Causes[edit | edit source]
Initial Injury: Almost any disease that results in tissue injury may result in MODS examples below:
Sepsis; Major trauma; Burns; Pancreatitis; Aspiration syndromes; Extracorporeal circulation (e.g. cardiac bypass); Multiple blood transfusion; Ischaemia–reperfusion injury; Autoimmune disease; Heat-induced illness; Eclampsia; Poisoning/toxicity[3]
Mechanism and Types of MODS[edit | edit source]
In general, the cause of post injury MODS involves a mixed layering of patient, injury and treatment factors. The dysregulated immunological response is the crucial factor in the pathophysiology of post injury MODS.
Following the initial injury the following changes are proposed to occur
- Shock: Medical emergency in which the organs and tissues of the body are not receiving an adequate flow of blood. This deprives the organs and tissues of oxygen (carried in the blood) and allows the buildup of waste products. Shock can result in serious damage or even death[4]
- Whole body Hyperfusion: A condition of acute peripheral circulatory failure due to derangement of circulatory control or loss of circulating fluid. It is marked by hypotension and coldness of the skin, and often by tachycardia and anxiety, can be fatal
- Resuscitation[1]: The restoration of consciousness to a person who appears dead.
- Reperfusion of ischaemic gut leads to cascade of events: gut translocation of micro-organisms precipitating and/or perpetuating this inflammatory response -compensatory anti-inflammatory response (CARS) results in immunosupression and anergy
- Coagulation cascade - triggered by tissue factor, endotoxins, cytokines and bacterial antigens.
- Cyrokines (image 2 cytokine release): Pro-and anti-inflammatory cytokines are released excessively during the initial phase of trauma. The role of the anti-inflammatory cytokines is to down-regulate the production of pro-inflammatory cytokines. Normally, the balance of pro- and anti-inflammatory cytokines is in equilibrium, however, when this natural balance is unbalanced with the release of predominantly pro-inflammatory cytokines, this leads to Systemic inflammatory response syndrome, while predominance of anti-inflammatory cytokines causes immunosuppression.[1]
- Neuro-endocrine factors - neurally mediated immune-suppression - stress responses involving adrenal hormones - hypothyroid state due to production of inert reverse T3 (Reverse T3 is sort of a hibernation hormone, in times of stress and chronic illness, it lowers your metabolism)[5]
- Mitochondrial dysfunction: may be mediated by humoral factors and may contribute to cellular dysoxia and organ dysfunction[3]
Other factors include:
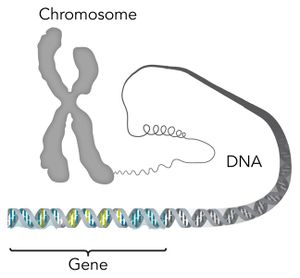
- differences in gene expression and the proteome may account for individual differences in the likelihood and severity of MODS following a given stimulus
- patients with premorbid organ dysfunction are more likely have further deterioration of organ function
Medications, therapies and ICU supports
- ventilator-induced lung injury contributing to pulmonary cytokine release and acute respiratory distress syndrome (ARDS)
- also: fluid therapy, hypothermia, ECMO, immobility, inotropes, blood products, etc[3]
Symptoms[edit | edit source]
The patient may display some of the following symptoms depending on which organs are affected:
- An altered mental state;
- A decrease in renal perfusion (decrease in urine output);
- Respiratory deterioration;
- A decrease in cardiac function;
- Deranged metabolic status;
- A compromised fluid balance;
- Pale, clammy, peripherally cool skin and faint pedal pulses; and
- A decrease in cardiac output (e.g. low blood pressure, arrhythmia)[6].
Management and Treatment[edit | edit source]
MODS is difficult to treat, escalates quickly and is often fatal. Therefore, early detection is crucial in preventing its progression (Wang et al. 2017).
Positive patient outcomes rely on immediate recognition, ICU admission and invasive organ support.
Management and treatment may include:
- Identifying and treating the underlying causes, comorbidities or complications;
- Fluid resuscitation to increase perfusion
- Support care and monitoring:
- Multi-organ support;
- Mechanical or non-invasive ventilation;
- Maintaining fluid homeostasis; and
- Renal replacement therapy.[6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 El-Menyar A, Al Thani H, Zarour A, Tuma M, AbdulRahman H, Parchani A, Peralta R, Latifi R. Multiple Organ Dysfunction Syndrome (MODS): is it preventable or inevitable?.Available from:https://file.scirp.org/pdf/IJCM_2013010210123433.pdf (accessed 28.2.2021)
- ↑ Gourd NM, Nikitas N. Multiple organ dysfunction syndrome. Journal of intensive care medicine. 2020 Dec;35(12):1564-75.Available from: https://journals.sagepub.com/doi/10.1177/0885066619871452 (accessed 28.2.2021)
- ↑ 3.0 3.1 3.2 In the fast lane MODS Available from:https://litfl.com/multiple-organ-dysfunction-syndrome/ (accessed 28.2.2021)
- ↑ The free dictionary Shock Available from: https://medical-dictionary.thefreedictionary.com/shock(accessed 28.2.2021)
- ↑ THYROID LAB INTERPRETATION GUIDE Reverse 3 Available from: https://www.thyroidlabguide.com/reverse-t3.html (accessed 28.2.2021)
- ↑ 6.0 6.1 Ausmed MODS Available from:https://www.ausmed.com/cpd/articles/multiple-organ-dysfunction-syndrome (accessed 28.2.2021)