Moving and Handling
Original Editors - Samuel Winter
Top Contributors - Leana Louw, Samuel Winter and Lucinda hampton
Description[edit | edit source]
Moving and handling forms a key part of most occupations. It refer to moving and handling loads like objects or people.[1] This page will look into the ergonomics behind the safe moving and handling practices relating to physiotherapy.
Ergonomics works to optimise the efficiency, health, safety and ease of people or interactive components in the everyday personal, work and leisure activities.[2] It is the study of a person in their work or home environments to balance work equipment, work pattern and work environment to optimally function in ideal circumstances. Incorrect or improper moving and handling can have a massive personal and economical burden, which makes optimal ergonomics and kinetic handling of utmost importance. If not followed properly, it can lead to an increase in injuries, which can have the following results:[3][4]
- Dysfunction/disability
- Absenteeism from work
- Poor quality of life for individuals
- Impact role in community (as per ICF model)
- Loss of manpower leading to financial losses
- Depleted workforce which impacts on the economy.
Physiotherapists has a role to play in the prevention and minimisation injury risk from poor moving and handling.[1]
Ergonomics[edit | edit source]
Factors relating to ergonomics[3][edit | edit source]
- Influenced by a person's susceptibility to injury
- Higher levels of stress
- Intra-individual factors:
- Age - increased risk for injury with increase in age
- Sex - women are more prone to injury
- Personality and mood
- Body type
- Physical abilities
- Nutritional and health status
- Work satisfaction and motivation
- Work pressure
- Previous experiences of similar work activities and/or repeated or boring work
- Habitual overwork pattern
- New demands (physical or psychological)
- Other psychological factors - including home, family and community
- Extra-individual factors: Refers to physical workload and effect on the functional abilities of the individual[3]
- Factors influencing load: Size, weight, method of packaging
- Specific handling methods
- Frequency and amount of repetitions of movement or activity
- Time worked without rest period
- Availability of mechanical aids (such as hoists, trucks, cranes, etc.)
- Isometric muscle function (maintained static posture)[5]
- Posture at work being influenced by furniture or equipment
- Workplace setup[6]
- Environmental factors (e.g. temperature, humidity, noise, vibration, quality of light, chemical irritants, etc.)[5]
Kinetic handling principles[7][edit | edit source]
- Be prepared - know where the load is going, have the correct attitude, knowledge, skill and clothing
- Take note of floor surface and surroundings, as well as area moving to
- Test the weight that you know what to expect
- Use a firm grip
- Keep the weight close to your body ensuring the center of gravity is close to your base of support
- Pre-position your feet in the direction of movement
- Use a stable, broad base of support (bending your knees as a lower center of gravity is more stable)
- Maintain your lumbar lordosis to avoid excessive lumbar flexion) and activate your abdominal stabilizers (transverse abdominus)
- Bend your knees and lift the weight by extending your knees
- Avoid fast, uncontrolled movements, especially with turning
- Do not rotate your body during the movement, lift and rotate your feet - make sure your footware is appropriate
- Use your body weight and an appropriate lever where applicable
- If more than one person involved, clear instructions should be given - e.g. leader and follower
- Use mechanical aids for extra heavy objects
- ABC:
- Alignment (bend your knees, keep your pelvis neutral)
- Breathe (normal)
- Control (1/3)
Selecting Appropriate Techniques[edit | edit source]
To determine the task, it is important to take the following interactions and roles with the person doing the task into consideration:[8]
- Environment
- Task
- Task performance
- Equipment
Aim[3]
- Ensure the safety of the patient and staff
- Minimise patient dependence
Consider[3]
- If there really is a need for moving and handling
- Carry out a moving and handling risk assessment
- Task: Consider the involvement of risky movement, twisting, stooping, bending, pushing, pulling, sudden movement of the load, team handling or seated work. Try and avoid or minimize the task itself and associated risk.
- Individual: Consider who could be/will be performing the task, injuries, previous injury and younger workers
- Load: The person moving, balance, size, skin integrity
- Environment: Floor conditions, floor levels, space constraints and lighting
- Other factors: Protective equipment, help, hindrance
- Review the technique consistently, especially if:
- There are changes in a patients condition
- Manual handling needs change
Overview of Techniques[edit | edit source]
Preparation[3]
- Ensure clothing (including footwear) are appropriate
- Ensure all participants are aware of the task, including the order of specific task and end position of the patient
- Get the equipment ready and in order, with required accessories
- Prepare the environment, clear route and access ways are clear, move objects, and the destination is ready
- Prepare client, explain what will happen and what they are expected to do. Ensure clothes, including footwear, are appropriate, ensure they have any aids they need
- Choose a lead caregiver
- Count down "ready, steady, move" prior to the task
Communication between caregiver and patient[3]
- Talk through the steps prior
- Ask if OK as being moved
- Ask how they felt after the transfer
Moving and handling[edit | edit source]
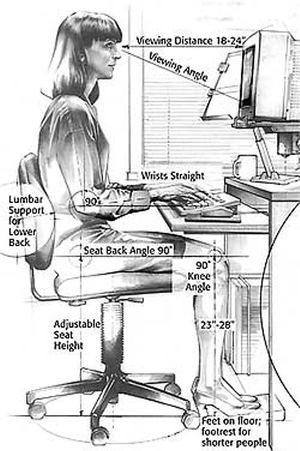
Work stations[edit | edit source]
Workstation adjustment is a very important aspect to aim to prevent repetitive strain injuries for desk workers by improving posture. The following principles need to be taken into account:[9]
- Keep your head in a balanced position with chin tucked
- Computer screen:
- Positioned to be able to look down at a 15 degree angle
- Screen and work surface should be glare and reflection free
- Tiltable screen
- Height adjustable swivel stand screen
- Keyboard should be detached and flat
- Thin based desk with maximum thigh space
- Feet should be flat on ground or footrest available for positioning
- Shoulders relaxed
- Forearms horisontal
- Keep wrists in balanced position
- Chair:
- Adequate lower back support at belt level
- Ideally height and angle adjustable backrest
- Adjustable height (e.g. gas lift)
- 5 star stable base (wheels)
- No obstructions to leg movement
- Adequate illumination, ideally from the side
Mobilisation[edit | edit source]
Sitting[8][edit | edit source]
Preparation[edit | edit source]
- Check a patients weight-bearing status with colleagues, medical notes, the client and family if needed
- Consider hoisting if non-weight bearing, never put weight through a patients non-weight bearing leg
- Make sure the patient knows what to expect during the transfer
Supervising sitting repositioning[edit | edit source]
- Patient places feet flat of the floor and slightly under the chair
- Patient leans forwards so weight is over their knees
- Patient stands, moves as far back into the seat as possible OR pushes back on armrests and their feet to slide back into the seat
Assistance Sitting[edit | edit source]
- Ask client to feel for chair on back of legs, reach for armrests and slowly lower themselves
- Encourage client to bend at the hips
Standing[8][edit | edit source]
Supervising standing[edit | edit source]
- Patient places hands on armrests, feet flat of the floor and slightly under the chair
- Pt moves slightly closer to the edge of the seat
- Pt sits forwards, "nose over toes"
- If needed, the patient rocks backwards and forwards
- Patient leans forwards so weight is over their knees
- Carer counts down "ready, steady, stand". On stand, the patient pushes up into a standing position
Assistance Standing[edit | edit source]
- Caregiver adopts the lunge position, beside the patient
- Outside hand is flat on the front of patients shoulder, inside arm across lower back
- With weight starting on the back foot, carer rocks forward with the client
- Check clients arms are free and in front
Making use of a hoist
- Apply hoist sling
- Position hoist sling
- Position hoist
- Position sling bar and attach sling straps to hoist
- Instruct client to stand
- Reposition hoist
- Instruct client to sit
Bed Mobility[edit | edit source]
Rolling in bed[edit | edit source]
Supervised[8]
- Patient turns head in direction of roll
- Patient flexes knee further from the direction of roll
- Places arm across their chest in direction of roll
- Client rolls over, pushing with outside of foot and reaching across body
- Client completes roll
Assistance[8]
- Patient turns head in direction of roll
- Patient flexes knee further from the direction of roll
- Patient crosses arms against chest
- Therapist stands in direction of roll and places one hand on furthest shoulder, other on the furthest hip
- Client is rolled onto their side
Moving in bed[8][edit | edit source]
- Teach the patient to do a bridge to move up and down in the bed
- Patient to hold on to head of bed with arms and pull themselves up. This can be done in combination with a bridge, and works well in patients with an increased BMI, or that have specific lower limb weight bearing limitations/pain, preventing them to do an optimal bridge.
1 x assistance:
- Assist to lift pelvis
- Place patient in crook lying
- Put one around patient's shoulders and the other at the back of the scapula
- Assist with pulling upwards when the patient does a bridge
Sitting over the edge of a bed[edit | edit source]
Supervised[10]
- Patient turns to their side, facing the carer
- Patient places outside hand and inside elbow flat on the bed
- Client puts legs over the edge of the bed
- Uses hands and elbow to push up whilst lowering legs to floor
Slide sheets[edit | edit source]
Applying[8]
- Place slide sheets underneath a bed sheet
- Keep edges of slide sheet to edge of the bed
- Push slide sheet under the patient, pushing down on the mattress
- Roll patient to the side and pull through the slide sheets
Pushing client up the bed with slide sheets[8]
- Apply slide sheets
- Place extra pillow at head of the bed
- Enter a lung position
- Patient pushes up the bed with their feet, whilst carers slide up the bed
Removing slide sheets[8]
- Tuck in both sheets on one side
- In a lunge position, a therapist pulls out diagonally from the other side
- Place sheets neatly for next use
Lateral Transfers[edit | edit source]
Sitting to sitting[edit | edit source]
Supervision[8]
- Patient leans forward and slides to the front of the chair
- Client places leading foot in the direction they're going
- Patient reaches forwards to take the far arm of the chair
- The client pushes through their arms and legs
- Client transfers to the other chair
- Client lowers into chair
Therapist stays close by throughout
Assistance without an aid[8]
- Assisted sit to stand (as above)
- Patient instructed to walk or step to another chair
- Patient instructed to reach for the armrests
- Patient sits down
Transfer board and slide sheets[edit | edit source]
- Beds moved together
- Side sheets positioned on transfer board
- Assistance to roll onto the side away from the direction of transfer
- Transfer board placed underneath the patient
- Patient rolled back to neutral
- Patient slide to target bed
- Transfer board and slide sheets removed
Hoisting[edit | edit source]
Applying a sling in bed[8][edit | edit source]
Therapist one:
- folds the sling with labels and handles on the outside
- Position the sling from the base of the spine upwards
- Feed the upper strap under the client's neck
- Fold the upper shoulder loop into sling and roll the upper portion of the sling into the space behind the client's back
Therapist two:
- Locate the loop from under the patient's neck and pull towards you
Both therapists:
- Pull slings towards themselves, removing creases
- Complete the sling positioning, crossing leg loops between legs
Applying a sling to a client in a chair[8][edit | edit source]
- Ask the client to lean forward in the chair
- Place the sling behind the client
- Ensure the bottom of the sling reaches the base of the spine and that the sling is positioned correctly
- Put the leg straps under each leg one at a time
Hoisting from bed to chair[8][edit | edit source]
- Lower the sling bar above the client's chest
- Attach the sling to the bar,
- Slowly raise the patient off the mattress
- Move hoist so the client is over the chair
- Place a hand on the sling bar whilst lowering the patient
- Remove the sling from the bar and move the hoist away
- Remove sling
Resources[edit | edit source]
- Manual Handling Assessment Charts
- Risk Assessment Tool for Pushing and Pulling
- Manual handling at work: A brief guide
- Getting to grips with hoisting people == A brief guide ==
References[edit | edit source]
- ↑ 1.0 1.1 Health and Safety Executive. Moving and handling in health and social care. Available from: https://www.hse.gov.uk/healthservices/moving-handling.htm (accessed 28/06/2020).
- ↑ Stevenson M. Readings in RSI. The ergonomics approach in repetitive strain injuries. New South Wales University Press, 1987.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Bridger R. Introduction to ergonomics. Crc Press; 2008.
- ↑ Levangie PK, Norkin CC. Joint Structure and Function; A Comprehensive Analysis. 3rd. Philadelphia: FA. Davis Company. 2000.
- ↑ 5.0 5.1 Sanders MJ. Ergonomics and the management of musculoskeletal disorders. Butterworth-Heinemann Medical; 2003 Dec 1.
- ↑ Kendall FP, McCreary EK, Provance PG, Rodgers M, Romani WA. Muscles, testing and function: with posture and pain. Baltimore, MD: Williams & Wilkins; 1993.
- ↑ Early Childhood Education Training and Resource Centre. Correct manual handling principles. Available from: http://www.ectarc.com.au/cybertots/toolbox12_11/shared/resources/html/res_correctmanhand.htm (accessed 26/06/2020).
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 Turner A, Foster M, Johnson SE, editors. Occupational therapy and physical dysfunction: principles, skills and practice. Edinburgh: Churchill Livingstone; 2002.
- ↑ Ergonomics Health Association. How To Create The Ideal Ergonomic Workstation Setup In 2020. Available from: https://ergonomicshealth.com/ergonomic-workstation-setup/ (accessed 28/06/2020).
- ↑ Pedretti LW, Early MB, editors. Occupational therapy: Practice skills for physical dysfunction. St. Louis, MO: Mosby; 2001 Feb.